- Departments of Neurosurgery, Hospital Privado de Rosario, Rosario, Santa Fe, Argentina.
- Departments of Anesthesiology, Hospital Privado de Rosario, Rosario, Santa Fe, Argentina.
Correspondence Address:
Ignacio J. Barrenechea
Departments of Neurosurgery, Hospital Privado de Rosario, Rosario, Santa Fe, Argentina.
DOI:10.25259/SNI_442_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ignacio J. Barrenechea, Héctor Rojas, Marco Nicola, Luis Marquez, Roberto Herrera, Facundo Van Isseldyk. A novel temporary cranial fixation device for awake cranial surgery: Technical report of 14 cases. 24-Jan-2020;11:12
How to cite this URL: Ignacio J. Barrenechea, Héctor Rojas, Marco Nicola, Luis Marquez, Roberto Herrera, Facundo Van Isseldyk. A novel temporary cranial fixation device for awake cranial surgery: Technical report of 14 cases. 24-Jan-2020;11:12. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9857
Abstract
Background: Awake craniotomy has become the gold standard in various cranial procedures. As part of the awake technique, three-point pin fixation of the patient’s head is important. One of the issues we encountered is the problem of matching the scalp infiltration site with the final pin position. To overcome this problem, we developed a flat plunger type fixator that adapts to the Mayfield holder.
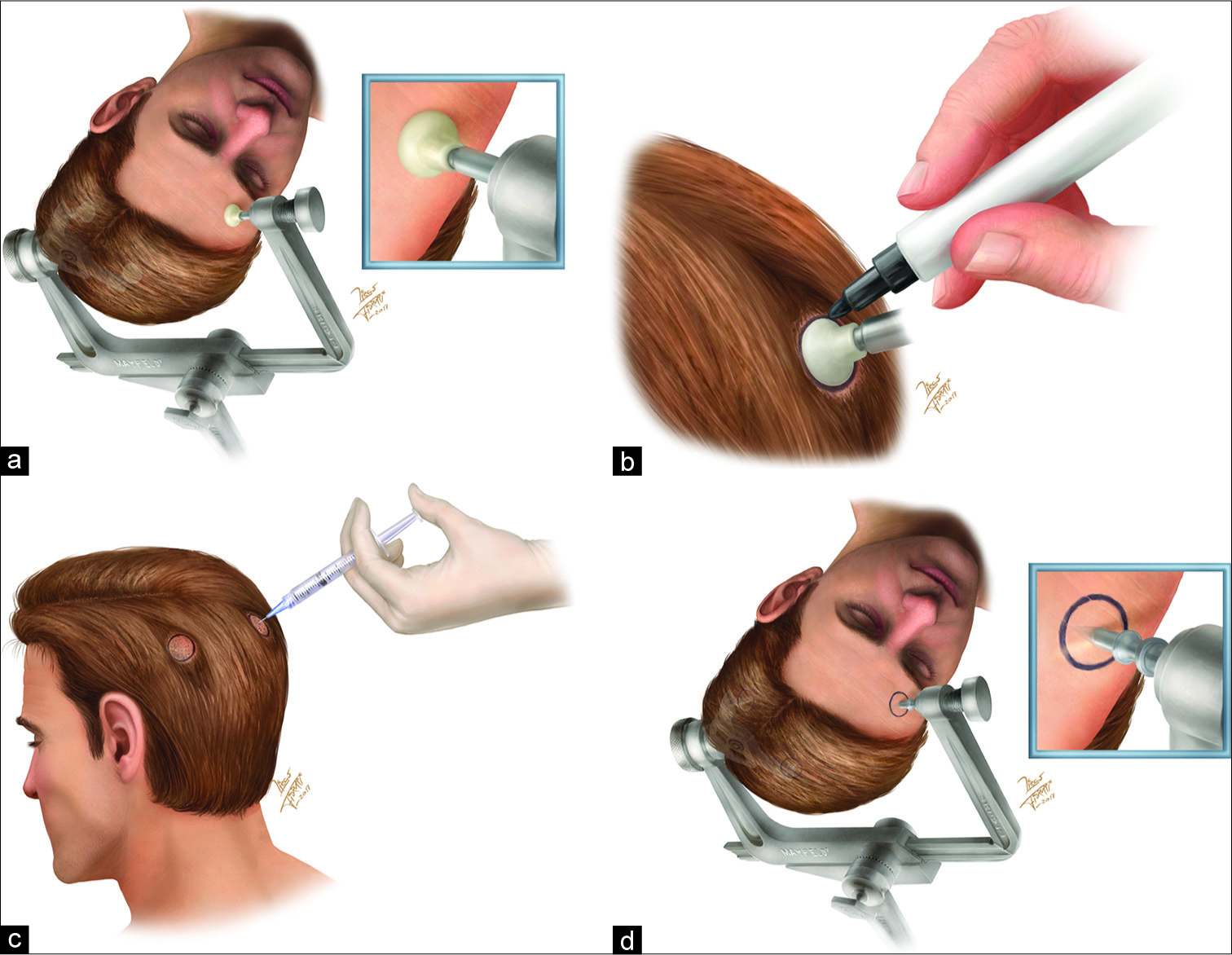
Methods: Our fixator has a 2.5 cm metallic shaft that articulates in a ball and socket joint to allow its concave surfaces to adapt to the patient’s scalp. After placing the patient in the desired position, the head is fixed with the three plungers, circles are drawn around each plunger, and they are then removed for the circles to be infiltrated with bupivacaine. Standard fixation pins are then placed in the Mayfield holder and aimed at the center of the circles.
Results: So far, we have operated on 14 patients with this technique. No patient experienced pain during temporary fixation, and the drawn circles ensured that there were no mismatches between the local anesthetic and pin locations. The technique was particularly useful on hairy scalps, where infiltration sites were hidden. We also used only 22.5 mg bupivacaine at the pin sites, freeing a dose for the field block around the scalp incision.
Conclusion: The temporary plunger type fixator provided a simple method to economize on local anesthetic use, check the patient’s head position before final fixation, and ensure that the Mayfield pins matched with the anesthetized area.
Keywords: Craniotomy, Infiltration, Local anesthesia, Technique, Tumor
INTRODUCTION
Awake craniotomy has become gold standard in various cranial procedures, especially in the surgical management of gliomas. The use of awake mapping has improved neurological outcomes and has increased the potential extent of resection.[
CLINICAL PRESENTATION
We developed a flat plunger type fixator called ARTFIX (Temporary Fixation System) that adapts to the Mayfield head holder [
This technique required the assistants to hold the patient’s head and draw the circles, while the surgeon presented the head holder loaded with the plungers. In this way, the patient’s head could be oriented in the desired position by temporary fixation, allowing for perfect matching of the Mayfield pin sites to the areas treated with a local anesthetic. On postoperative day 1, patients were asked whether they had felt pain related either to the ARTFIX or to pin positioning. They were shown a visual analog scale (VAS) to describe this step of the procedure.
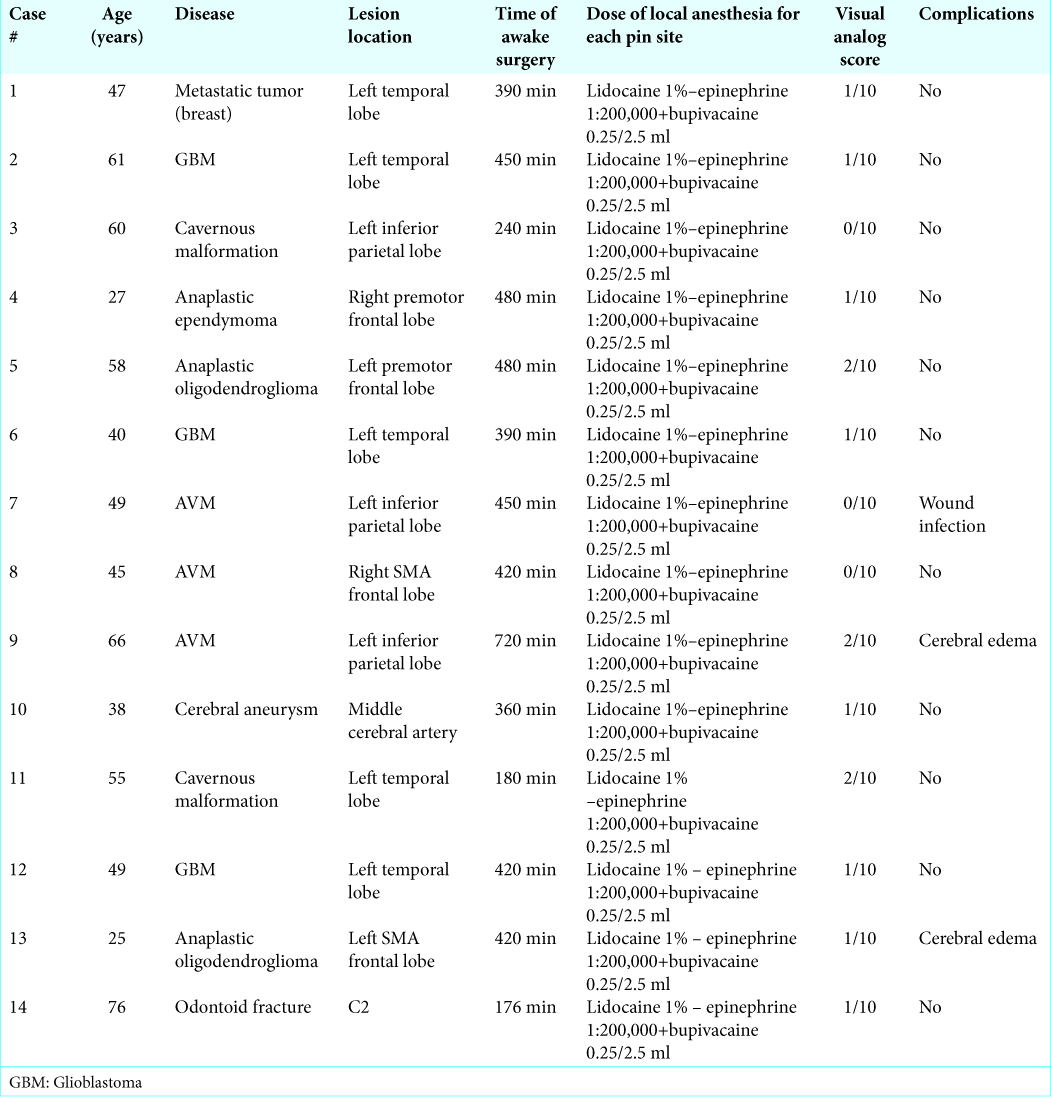
To date, we have used our novel technique for 13 awake craniotomies and one awake C1-C2 fusion [
Figure 3:
Representative images of intraoperative positioning for awake craniotomy using ARTFIX Images for Cases 4 (a-c) and 5 (d and e) are shown. (a) Initial fixation of the patient’s head with ARTFIX, (b) a circle is marked on the frontal scalp, (c) final pin placement inside the marked circle, (d) a marked circle on the occipital scalp, (e) final position before craniotomy.
No patient in this series experienced pain during the placement of the temporary cranial fixation device, which was well tolerated in all cases [
DISCUSSION
Awake craniotomy has become a versatile tool in the treatment of brain tumors. Its use permits maximal tumor resection with a reduction in the risk of postoperative speech and motor deficits.[
Maintaining patients’ comfort during the procedure is essential to ensure adequate brain mapping and optimal tumor resection. However, headache is a common complaint when using fixation devices, and Keifer et al.[
Another important issue that patients must be comfortable during the “awake” part of the procedure, and the surgeon, anesthesiologist, and neurologist/speech therapist must agree on the final position. By fixing the head temporarily, the team can double-check and agree on the patient’s final head position before the pins are placed.
It is not always easy to match the infiltration and pin sites with the standard technique, especially on hairy scalps. Although a wider infiltration field could accomplish this task, the potential toxicity of local anesthetics needs to be considered (e.g., dysrhythmias, hypotension, and depressed cardiac output), with surgeons only having a fixed amount of local anesthetic to use for the entire procedure.[
Scalp infiltration with local anesthetics can protect against potentially dangerous increases in arterial pressure when the Mayfield holder is used.[
The main drawback we found using this new device, is the need for two assistants (one to hold and rotate the patient’s head as required, and the other one to draw the circles with a marking pen). Furthermore, for patients with dense hair, it is sometimes needed to shave a circle about the size of the plungers to draw the circles.
CONCLUSION
Patient comfort during intraoperative stimulation mapping surgery is crucial to improving outcomes. The temporary fixation device reported in this study provides a simple method that can economize on local anesthetic use at the cranial fixation site and allow the patient’s head position to be checked by all team members before final rigid fixation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arshad A, Shamim MS, Waqas M, Enam H, Enam SA. How effective is the local anesthetic infiltration of pin sites prior to application of head clamps: A prospective observational cohort study of hemodynamic response in patients undergoing elective craniotomy. Surg Neurol Int. 2013. 4: 93-
2. Burnand C, Sebastian J. Anaesthesia for awake craniotomy. Contin Educ Anaesth Crit Care Pain. 2014. 14: 6-11
3. De Benedictis A, Moritz-Gasser S, Duffau H. Awake mapping optimizes the extent of resection for low-grade gliomas in eloquent areas. Neurosurgery. 2010. 66: 1074-84
4. De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: A meta-analysis. J Clin Oncol. 2012. 30: 2559-65
5. Duffau H, Lopes M, Arthuis F, Bitar A, Sichez JP, Van Effenterre R. Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: A comparative study between two series without (1985-96) and with (1996-2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry. 2005. 76: 845-51
6. Keifer JC, Dentchev D, Little K, Warner DS, Friedman AH, Borel CO. A retrospective analysis of a remifentanil/propofol general anesthetic for craniotomy before awake functional brain mapping. Anesth Analg. 2005. 101: 502-8
7. Levin R, Hesselvik JF, Kourtopoulos H, Vavruch L. Local anesthesia prevents hypertension following application of the Mayfield skull-pin head holder. Acta Anaesthesiol Scand. 1989. 33: 277-9
8. Meyer FB, Bates LM, Goerss SJ, Friedman JA, Windschitl WL, Duffy JR. Awake craniotomy for aggressive resection of primary gliomas located in eloquent brain. Mayo Clin Proc. 2001. 76: 677-87
9. Poli J, Zoia C, Lattanzi D, Balbi S. Epidural haematoma by Mayfield head-holder: Case report and review of literature. J Pediatr Sci. 2013. 5: e195-
10. Potters JW, Klimek M. Local anesthetics for brain tumor resection: Current perspectives. Local Reg Anesth. 2018. 11: 1-8
11. Sacko O, Lauwers-Cances V, Brauge D, Sesay M, Brenner A, Roux FE. Awake craniotomy vs surgery under general anesthesia for resection of supratentorial lesions. Neurosurgery. 2011. 68: 1192-8
12. Taylor MD, Bernstein M. Awake craniotomy with brain mapping as the routine surgical approach to treating patients with supratentorial intraaxial tumors: A prospective trial of 200 cases. J Neurosurg. 1999. 90: 35-41
13. Yan HJ. Epidural hematoma following use of a three-point skull clamp. J Clin Neurosci. 2007. 14: 691-3








Mario salmon
Posted February 5, 2020, 7:56 pm
In my humble point of view if you’re going to do a surgery on awake patient, a good way of obtaining local anesthesia is by blocking occipital, temporal and supraorbital nerves according to the site of surgery and pin location. So I think this is too much, time wasting which goes by hand on expenses and operating time.