- Department of Neurosurgery, Mohamed V University, Rabat, Morocco.
DOI:10.25259/SNI_593_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hilal Abboud, Idris Ziani, Adyl Melhaoui, Yasser Arkha, Abdessamad Elouahabi. Traumatic cervical spine injury: Short-and medium-term prognostic factors in 102 patients. 07-Feb-2020;11:19
How to cite this URL: Hilal Abboud, Idris Ziani, Adyl Melhaoui, Yasser Arkha, Abdessamad Elouahabi. Traumatic cervical spine injury: Short-and medium-term prognostic factors in 102 patients. 07-Feb-2020;11:19. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9864
Abstract
Background: Traumatic cervical spine injuries (CSIs) can be defined as osteodiscoligamentous lesions and are frequent in the young and active population. These lesions are often associated with significant devastating neurological deficits. Here, we sought to establish short-and medium-term prognostic factors that could help predict future outcomes.
Methods: We retrospectively reviewed 102 adults admitted for traumatic CSI over an 11-year period (January 2004–December 2014). Patients were graded using Frankel scale as exhibiting good or poor outcomes.
Results: Two risk factors that significantly predicted results for CSI included original poor Frankel grades (e.g., A and B) and initial neurovegetative disorders (e.g., respectively, P = 0.019 and P = 0.001). However, we did not anticipate that two other risk factors, operative delay and mechanism of trauma, would not significantly adversely impact outcomes.
Conclusion: Here, we identified two significant risk factors for predicting poor outcomes following CSI; poor initial Frankel Grades A and B and neurovegetative disorders at the time of original presentation.
Keywords: Cervical spine, Frankel scale, Injury, Neurological deficit, Neurovegetative disorders, Prognostic factors, Trauma
INTRODUCTION
Knowing the significant prognostic factors associated with cervical spine injuries (CSIs) would facilitate early, rapid, and better management. This potentially would minimize risks and complications associated with various therapies and thereby reduce the morbidity and mortality for these patients.
Here, we have analyzed several major risk factors to determine whether they would significantly impact patients’ outcomes following SCI.
MATERIALS AND METHODS
Patients
We retrospectively studied 102 traumatic CSI patients, with/without other trauma, over an 11-year period (e.g., January 2004–December 2014).
They were treated surgically/nonsurgically by neurosurgeons (e.g., undergoing spinal surgery) and a subset required other surgical procedures.
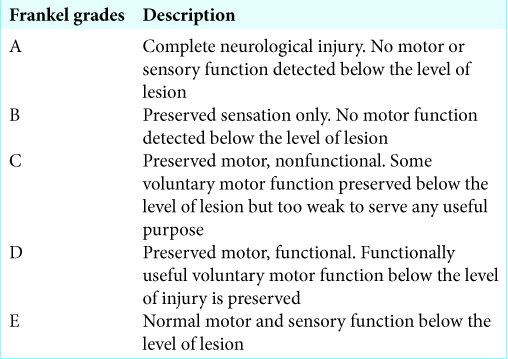
Patients were neurologically evaluated using the Frankel grading system [
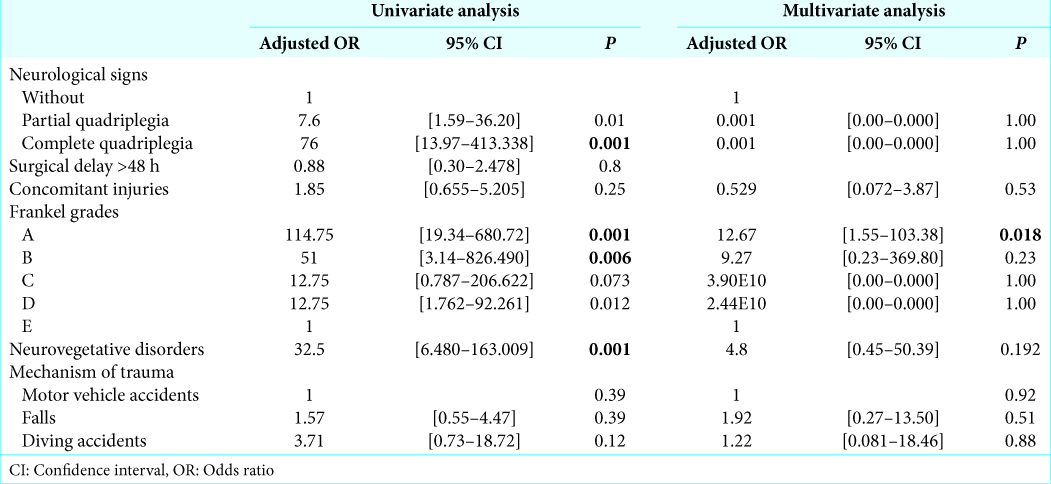
Prognostic factors were assessed utilizing univariate and multivariate logistic regression analysis [
Clinical data
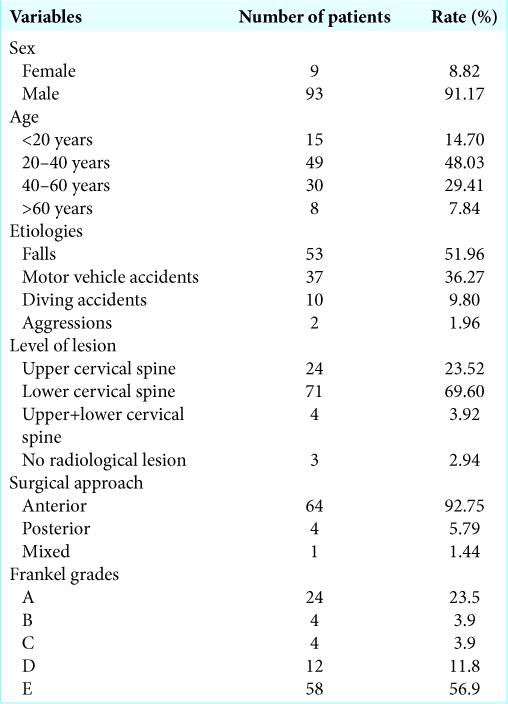
From 350 registries, we identified 102 patients for our CSI series [
Traumatic etiologies included falls 53 cases (52%), motor vehicle accidents: 37 patients (36.3%), and diving: 10 cases (9.8%).
Of the 102 patients, 58 had no neurological deficits (56.86%), while 44 patients (43.13%) had varying Frankel grade deficits.
The lower cervical spine involved in 71 cases, followed by the upper cervical spine (24 cases), while 4 had mixed proximal/distal lesions and 3 cases did not have any vertebral lesions.
There were 26 patients who were treated with cervical spine traction and/or placement of a cervical collar. Alternatively, 69 had surgery an average of 5 days (range 15 h–20 days) following the traumatic event consisting of anterolateral approaches (64 cases) and posterior approaches (4 cases).
RESULTS
Higher mortality rate with worse Frankel grades and neurovegetative disorders
There were 18 deaths (e.g., 17.7% of all traumatic cervical spine injury (TCSI) patients: 16 deaths for Frankel A, 1 death for Frankel B, and 1 death for Frankel E)
The mortality rate of Frankel Grade A exceeded 70%. The overall mortality for patients with neurovegetative disorders exceeded 75%.
Univariate analysis
Initial presentation with complete quadriplegia was associated with 76-fold increased risk of poor outcome, as well as surgical delay of over 48 h was associated with 8-fold increased risk of poor outcome. Specifically, Frankel Grade A was associated with 114-fold increased risk of poor outcome and Grade B was associated with 51-fold increased risk of bad evolution, while neurovegetative disorders were associated with 32.5-fold increased risk of poor outcome (P < 0.001).
Further, traumatic CSIs due to a diving accident were associated with a 4-fold increase in the risk of bad evolution compared to motor vehicle accidents and other traumatic etiologies.
Multivariate analysis
Adjusting for polytrauma, neurovegetative disorders, Frankel scale, mechanism of the trauma, and neurological signs, poor initial Frankel grades (e.g., A and B) were the most significant prognostic factor to correlate with poor outcomes. For example, a patient with Frankel Grade A is 13 times more likely to have a bad outcome compared to Frankel Grade E (P = 0.018).
DISCUSSION
Several clinicoradiological factors have been reported in the literature to be predictive of prognosis in TCSI, including original neurological deficit, medullary magnetic resonance imaging (MRI) signal, surgical delay, concomitant injuries, and mechanism of trauma.[
As the best independent prognostic factors in TCSI are the original neurological deficit, which correlate well with spinal cord damage severity, the Frankel grading system, which is simple, easily reproducible, and widely used, makes it possible to envisage the outcome according to the initial involvement.
In Frankel Grade A, except some rare cases of transient spinal stasis, neurological recovery is absent and mortality rate is high.[
According to our study, a Frankel Grade A is associated with 114-fold increased risk of poor outcome as well as Frankel Grade B is associated with 51-fold increased risk of poor outcome (e.g., respectively, P = 0.001 and 0.006). Similarly, immediate neurovegetative disorders are associated with 32.5-fold increased risk of bad evolution (P < 0.001) and are also a statistically significant poor prognostic factor.
Regarding other prognostic factors, some studies identified early surgery as associated with better neurological recovery compared to delayed surgery or conservative treatment.[
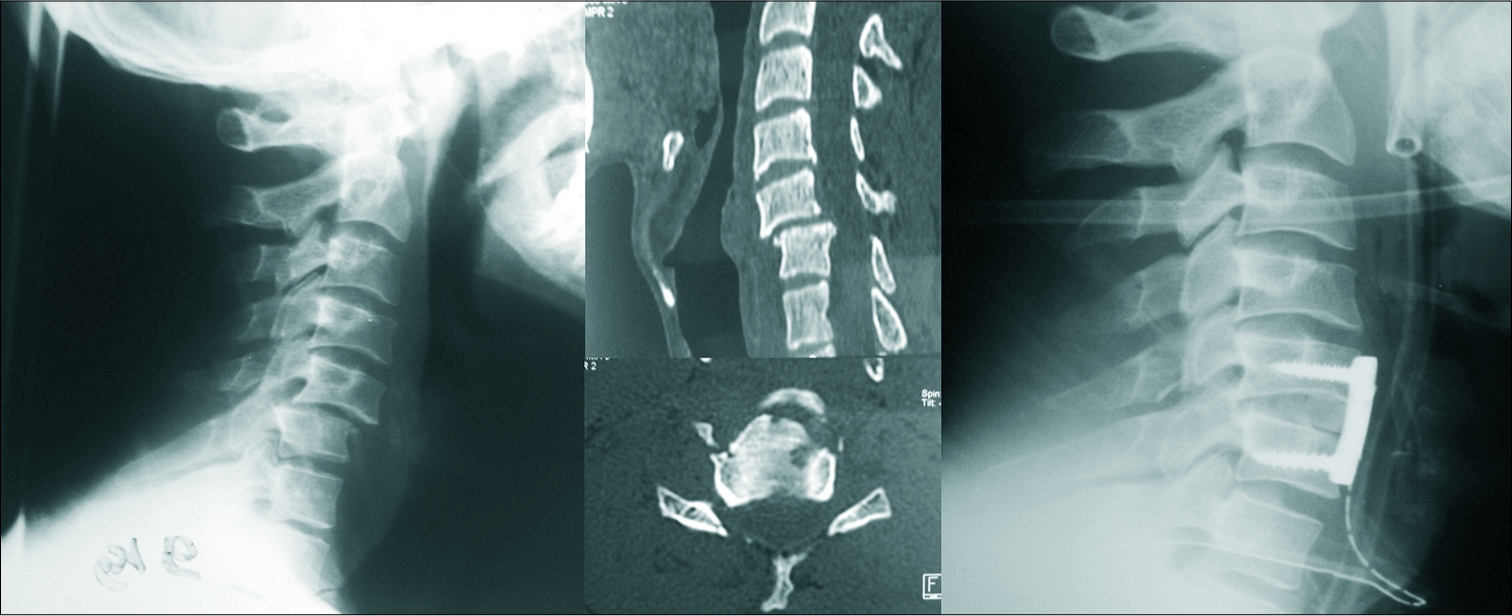
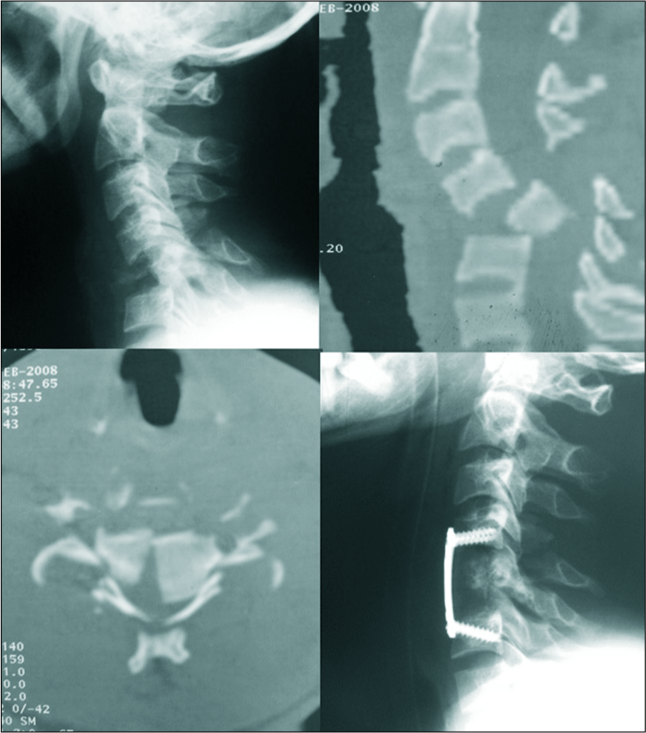
Figure 2:
Motor vehicle accident in a 30-year-old man, preoperative X-ray and computed tomography scan: C5 fracture and C4-C5 and C5-C6 dislocation, with receding of the posterior wall and spinal cord compression, postoperative X-ray: C5 corpectomy and discectomy of C4-C5 and C5-C6 with placement of the graft taken from the iliac crest and fixation by anterior plate on C4-C6.
CONCLUSION
We investigated prognostic factors for outcome following TCSI. We found that worse Frankel grades (e.g., A and B) and immediate neurovegetative disorders are statistically significantly associated with an increased risk of poor outcome in short and medium term. Other factors, such as concomitant injuries and TCSI by diving, were also associated with increased risk of poor outcome, but these results were not statistically significant.
Authors’ contributions
All authors contributed to this work: Abboud Hilal: collecting information and writing of the manuscript, Idris Ziani performed statistical analyses and tests, and the other authors corrected the manuscript. All authors read and approved the final version of this manuscript.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andreoli C, Colaiacomo MC, Rojas Beccaglia M, Di Biasi C, Casciani E, Gualdi G. MRI in the acute phase of spinal cord traumatic lesions: Relationship between MRI findings and neurological outcome. Radiol Med. 2005. 110: 636-45
2. Bötel U, Gläser E, Niedeggen A. The surgical treatment of acute spinal paralysed patients. Spinal Cord. 1997. 35: 420-8
3. Campagnolo DI, Esquieres RE, Kopacz KJ. Effect of timing of stabilization on length of stay and medical complications following spinal cord injury. J Spinal Cord Med. 1997. 20: 331-4
4. Cao BH, Wu ZM, Liang JW. Risk factors for poor prognosis of cervical spinal cord injury with subaxial cervical spine fracture-dislocation after surgical treatment: A consort study. Med Sci Monit. 2019. 25: 1970-5
5. Chipman JG, Deuser WE, Beilman GJ. Early surgery for thoracolumbar spine injuries decreases complications. J Trauma. 2004. 56: 52-7
6. Croce MA, Bee TK, Pritchard E, Miller PR, Fabian TC. Does optimal timing for spine fracture fixation exist?. Ann Surg. 2001. 233: 851-8
7. Duh MS, Shepard MJ, Wilberger JE, Bracken MB. The effectiveness of surgery on the treatment of acute spinal cord injury and its relation to pharmacological treatment. Neurosurgery. 1994. 35: 240-8
8. Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976). 2010. 35: S166-73
9. Fielingsdorf K, Dunn RN. Cervical spine injury outcome--a review of 101 cases treated in a tertiary referral unit. S Afr Med J. 2007. 97: 203-7
10. Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK. Traumatic central cord syndrome: Results of surgical management. J Neurosurg. 2002. 97: 25-32
11. Igun GO, Obekpa OP, Ugwu BT, Nwadiaro HC. Spinal injuries in the Plateau State, Nigeria. East Afr Med J. 1999. 76: 75-9
12. Kawu K, Adebule GT, Gbadegesin AA, Alimi MF, Salami AO. Outcome of conservative treatment of spinal cord injuries in Lagos, Nigeria. Niger J Orthop Trauma. 2010. 9: 21-3
13. La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004. 42: 503-12
14. Malik SA, Murphy M, Connolly P, O’Byrne J. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008. 17: 585-91
15. Matsushita A, Maeda T, Mori E, Yugue I, Kawano O, Ueta T. Subacute T1-low intensity area reflects neurological prognosis for patients with cervical spinal cord injury without major bone injury. Spinal Cord. 2016. 54: 24-8
16. McDonald JW, Sadowsky C. Spinal-cord injury. Lancet. 2002. 359: 417-25
17. Ojo OA, Poluyi EO, Owolabi BS, Kanu OO, Popoola MO. Surgical decompression for traumatic spinal cord injury in a tertiary center. Niger J Clin Pract. 2017. 20: 1455-60
18. Singhal B, Mohammed A, Samuel J, Mues J, Kluger P. Neurological outcome in surgically treated patients with incomplete closed traumatic cervical spinal cord injury. Spinal Cord. 2008. 46: 603-7
19. Srinivas BH, Rajesh A, Purohit AK. Factors affecting outcome of acute cervical spine injury: A prospective study. Asian J Neurosurg. 2017. 12: 416-23