History
49 y/o right-handed male presents with history of medically controlled seizures for 10 years and progressive visual loss that led to complete blindness for six weeks. History is significant for a right temporal cystoperitoneal shunt seven years prior to presentation, completed at an outside facility. At the time of initial shunting, there was no pathological diagnosis and the lesion was believed to be a benign cyst. Physical exam demonstrated bilaterally dilated and non-reactive pupils and fundoscopic exam showed bilateral papilledema.
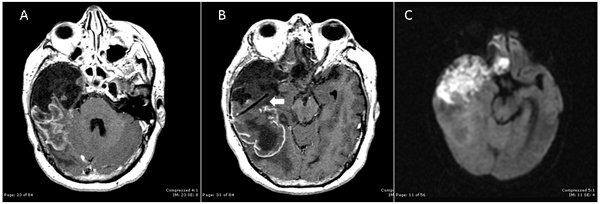
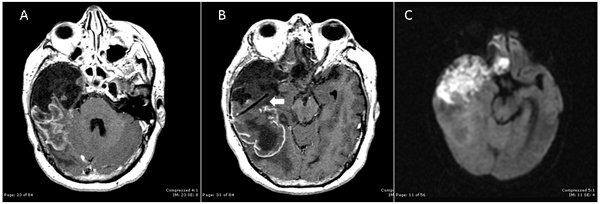
Initially given the extensive nature of the tumor and the patient’s blindness and deficit, no surgery or a biopsy were the choices of treatment suggested. On consultation opthalmology stated that the patient’s blindness was likely secondary to a persistent increased in intracranial pressure (ICP). The patient additionally had left-sided weakness against resistance, more prominent in the upper extremity. Axial cuts of gadolinium-enhanced MRI at presentation are shown in A and B. Diffusion-weighted image, a sequence sensitive for water-based molecular diffusion in the brain, is shown in C. These are often helpful for the neurosurgeon to differentiate CSF filled structures (like an arachnoid cyst) which appear hypointense from tumor which is often iso- or hyper- intense.
The imaging was reviewed extensively with both neurosurgical staff and neuroradiology, and it was felt that this likely represented a highly malignant and invasive tumor. Given this, concerns were raised regarding the goals and potential surgical morbidity of craniotomy for such a large and potentially invasive tumor. As a result, multiple physicians suggested limited tissue biopsy or no surgery at all.
 Differential Diagnosis:
High-grade glioma (grade III or IV astrocytoma)
Oligodendroglioma
Decision
A lengthy discussion with the patient and family was undertaken. A definitive surgical approach was decided. The primary goals of the surgery were to obtain a tissue diagnosis and remove local mass effect, especially upon the optic nerve. The patient was taken to the operating room for fronto-temporal craniotomy. A cystic tumor that consisted of white cheesy material with only minimal invasion of the surrounding brain was encountered. The tumor was debulked and removed subtotally. A region of infiltration which appeared to likely involve the ipsilateral motor cortex was not debulked given concern for potential post-operative morbidity. Following the operation, the patient’s papilledema resolved, and his left-hemiparesis improved. His pupils, while previously non-reactive, had limited reactivity and he was able to see the outline of objects.
Pathological Diagnosis: Epidermoid Cyst with areas of poorly differentiated squamus cell carcinoma
Intracranial epidermoid cysts are benign, slow growing tumors which account for 0.2-1.8% of all intracranial tumors [1]. Malignant transformation is exceedingly rare, but may develop from existing lesions or following incomplete resection [2]. In known cases series, the interval from recognition of the benign cysts until malignant transformation ranged from 3 months to 33 years [2]. It is felt that the chronic inflammatory changes from repeated rupture of intracranial cysts may lead to malignant change [3]. Surgical treatment of squamus cell carcinoma arising from epidermoid cysts often is limited to partial removal given that the tumor capsule is often attached to critical structures. As a result, careful surgical debulking, followed by stereotactic radiosurgery with external beam radiotherapy has been encouraged [4,5].
Zachary A. Smith, M.D.,1,2 Colin Buchanan, M.D.1,2, and Duncan Q. McBride M.D.1,2
1-Division of Neurosurgery; Harbor-UCLA Medical Center; Los Angeles, CA.
2-Department of Neurosurgery, Ronald Reagan-UCLA Medical Center; Los Angeles, CA
Author Contact:
Zachary A. Smith
zsmith@mednet.ucla.edu
Ronald Reagan-UCLA Medical Center, UCLA Dept. of Neurosurgery
310-709-6405
References:
1. Ulrich J: Intracranial epidermoids, A study on their distribution and spread. J Neurosurg, 1964, 21: 1051-1058.
2. Tamura K, Aoyagi M, Wakimoto H, Tamaki M, Yamamoto K, Yamamoto M, Ohno K, Malignant transformation eight years after removal of a benign epidermoid cyst: A case report. J Neurooncol 2006, 79(1): 67-72.
3. Abramson RC, Morawetz RB, Schlitt M, Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery 1989, 24: 574-578.
4. Murase S, Yamakawa H, Ohkuma A, Sumi Y, Kajiwara M, Takami T, et al., Primary intracranial squamus cell carcinoma- case report. Neurol Med Chir (Tokyo) 1999, 39: 49-54.
5. Link MJ, Cohen PL, Breneman JC, Tew JM Jr, Malignant squamus degeneration of a cerebellopontine angle epidermoid tumor. Case report. J Neurosurg 2002, 97: 1237-1243.
Comments from the Editor-in-Chief:
This case represents a fundamental principle of medicine and neurosurgery regardless of what country in which one lives. The physicians in this case had presumed the diagnosis but had no proof for their opinion. The radiologists made the wrong diagnosis also. No radiologist or neurosurgeon or physician knows with 100% certainty what the TISSUE diagnosis is. Therefore, you must obtain a tissue diagnosis before you determine what the course of treatment will be. Yes, that also applies to brain stem, pineal or third ventricle or difficult lesions to reach. The patient must know the diagnosis in order to plan for his or her life. This patient would have been condemned to die by some physicians who assumed that the diagnosis was a malignant glioma. There was great resistance to operate on this patient. The end result confirms the principle that must never be forgotten. What is the proof for the diagnosis? That is the question the physician must answer and that the patient deserves the right to know.
Differential Diagnosis:
High-grade glioma (grade III or IV astrocytoma)
Oligodendroglioma
Decision
A lengthy discussion with the patient and family was undertaken. A definitive surgical approach was decided. The primary goals of the surgery were to obtain a tissue diagnosis and remove local mass effect, especially upon the optic nerve. The patient was taken to the operating room for fronto-temporal craniotomy. A cystic tumor that consisted of white cheesy material with only minimal invasion of the surrounding brain was encountered. The tumor was debulked and removed subtotally. A region of infiltration which appeared to likely involve the ipsilateral motor cortex was not debulked given concern for potential post-operative morbidity. Following the operation, the patient’s papilledema resolved, and his left-hemiparesis improved. His pupils, while previously non-reactive, had limited reactivity and he was able to see the outline of objects.
Pathological Diagnosis: Epidermoid Cyst with areas of poorly differentiated squamus cell carcinoma
Intracranial epidermoid cysts are benign, slow growing tumors which account for 0.2-1.8% of all intracranial tumors [1]. Malignant transformation is exceedingly rare, but may develop from existing lesions or following incomplete resection [2]. In known cases series, the interval from recognition of the benign cysts until malignant transformation ranged from 3 months to 33 years [2]. It is felt that the chronic inflammatory changes from repeated rupture of intracranial cysts may lead to malignant change [3]. Surgical treatment of squamus cell carcinoma arising from epidermoid cysts often is limited to partial removal given that the tumor capsule is often attached to critical structures. As a result, careful surgical debulking, followed by stereotactic radiosurgery with external beam radiotherapy has been encouraged [4,5].
Zachary A. Smith, M.D.,1,2 Colin Buchanan, M.D.1,2, and Duncan Q. McBride M.D.1,2
1-Division of Neurosurgery; Harbor-UCLA Medical Center; Los Angeles, CA.
2-Department of Neurosurgery, Ronald Reagan-UCLA Medical Center; Los Angeles, CA
Author Contact:
Zachary A. Smith
zsmith@mednet.ucla.edu
Ronald Reagan-UCLA Medical Center, UCLA Dept. of Neurosurgery
310-709-6405
References:
1. Ulrich J: Intracranial epidermoids, A study on their distribution and spread. J Neurosurg, 1964, 21: 1051-1058.
2. Tamura K, Aoyagi M, Wakimoto H, Tamaki M, Yamamoto K, Yamamoto M, Ohno K, Malignant transformation eight years after removal of a benign epidermoid cyst: A case report. J Neurooncol 2006, 79(1): 67-72.
3. Abramson RC, Morawetz RB, Schlitt M, Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery 1989, 24: 574-578.
4. Murase S, Yamakawa H, Ohkuma A, Sumi Y, Kajiwara M, Takami T, et al., Primary intracranial squamus cell carcinoma- case report. Neurol Med Chir (Tokyo) 1999, 39: 49-54.
5. Link MJ, Cohen PL, Breneman JC, Tew JM Jr, Malignant squamus degeneration of a cerebellopontine angle epidermoid tumor. Case report. J Neurosurg 2002, 97: 1237-1243.
Comments from the Editor-in-Chief:
This case represents a fundamental principle of medicine and neurosurgery regardless of what country in which one lives. The physicians in this case had presumed the diagnosis but had no proof for their opinion. The radiologists made the wrong diagnosis also. No radiologist or neurosurgeon or physician knows with 100% certainty what the TISSUE diagnosis is. Therefore, you must obtain a tissue diagnosis before you determine what the course of treatment will be. Yes, that also applies to brain stem, pineal or third ventricle or difficult lesions to reach. The patient must know the diagnosis in order to plan for his or her life. This patient would have been condemned to die by some physicians who assumed that the diagnosis was a malignant glioma. There was great resistance to operate on this patient. The end result confirms the principle that must never be forgotten. What is the proof for the diagnosis? That is the question the physician must answer and that the patient deserves the right to know.
 Differential Diagnosis:
High-grade glioma (grade III or IV astrocytoma)
Oligodendroglioma
Decision
A lengthy discussion with the patient and family was undertaken. A definitive surgical approach was decided. The primary goals of the surgery were to obtain a tissue diagnosis and remove local mass effect, especially upon the optic nerve. The patient was taken to the operating room for fronto-temporal craniotomy. A cystic tumor that consisted of white cheesy material with only minimal invasion of the surrounding brain was encountered. The tumor was debulked and removed subtotally. A region of infiltration which appeared to likely involve the ipsilateral motor cortex was not debulked given concern for potential post-operative morbidity. Following the operation, the patient’s papilledema resolved, and his left-hemiparesis improved. His pupils, while previously non-reactive, had limited reactivity and he was able to see the outline of objects.
Pathological Diagnosis: Epidermoid Cyst with areas of poorly differentiated squamus cell carcinoma
Intracranial epidermoid cysts are benign, slow growing tumors which account for 0.2-1.8% of all intracranial tumors [1]. Malignant transformation is exceedingly rare, but may develop from existing lesions or following incomplete resection [2]. In known cases series, the interval from recognition of the benign cysts until malignant transformation ranged from 3 months to 33 years [2]. It is felt that the chronic inflammatory changes from repeated rupture of intracranial cysts may lead to malignant change [3]. Surgical treatment of squamus cell carcinoma arising from epidermoid cysts often is limited to partial removal given that the tumor capsule is often attached to critical structures. As a result, careful surgical debulking, followed by stereotactic radiosurgery with external beam radiotherapy has been encouraged [4,5].
Zachary A. Smith, M.D.,1,2 Colin Buchanan, M.D.1,2, and Duncan Q. McBride M.D.1,2
1-Division of Neurosurgery; Harbor-UCLA Medical Center; Los Angeles, CA.
2-Department of Neurosurgery, Ronald Reagan-UCLA Medical Center; Los Angeles, CA
Author Contact:
Zachary A. Smith
zsmith@mednet.ucla.edu
Ronald Reagan-UCLA Medical Center, UCLA Dept. of Neurosurgery
310-709-6405
References:
1. Ulrich J: Intracranial epidermoids, A study on their distribution and spread. J Neurosurg, 1964, 21: 1051-1058.
2. Tamura K, Aoyagi M, Wakimoto H, Tamaki M, Yamamoto K, Yamamoto M, Ohno K, Malignant transformation eight years after removal of a benign epidermoid cyst: A case report. J Neurooncol 2006, 79(1): 67-72.
3. Abramson RC, Morawetz RB, Schlitt M, Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery 1989, 24: 574-578.
4. Murase S, Yamakawa H, Ohkuma A, Sumi Y, Kajiwara M, Takami T, et al., Primary intracranial squamus cell carcinoma- case report. Neurol Med Chir (Tokyo) 1999, 39: 49-54.
5. Link MJ, Cohen PL, Breneman JC, Tew JM Jr, Malignant squamus degeneration of a cerebellopontine angle epidermoid tumor. Case report. J Neurosurg 2002, 97: 1237-1243.
Comments from the Editor-in-Chief:
This case represents a fundamental principle of medicine and neurosurgery regardless of what country in which one lives. The physicians in this case had presumed the diagnosis but had no proof for their opinion. The radiologists made the wrong diagnosis also. No radiologist or neurosurgeon or physician knows with 100% certainty what the TISSUE diagnosis is. Therefore, you must obtain a tissue diagnosis before you determine what the course of treatment will be. Yes, that also applies to brain stem, pineal or third ventricle or difficult lesions to reach. The patient must know the diagnosis in order to plan for his or her life. This patient would have been condemned to die by some physicians who assumed that the diagnosis was a malignant glioma. There was great resistance to operate on this patient. The end result confirms the principle that must never be forgotten. What is the proof for the diagnosis? That is the question the physician must answer and that the patient deserves the right to know.
Differential Diagnosis:
High-grade glioma (grade III or IV astrocytoma)
Oligodendroglioma
Decision
A lengthy discussion with the patient and family was undertaken. A definitive surgical approach was decided. The primary goals of the surgery were to obtain a tissue diagnosis and remove local mass effect, especially upon the optic nerve. The patient was taken to the operating room for fronto-temporal craniotomy. A cystic tumor that consisted of white cheesy material with only minimal invasion of the surrounding brain was encountered. The tumor was debulked and removed subtotally. A region of infiltration which appeared to likely involve the ipsilateral motor cortex was not debulked given concern for potential post-operative morbidity. Following the operation, the patient’s papilledema resolved, and his left-hemiparesis improved. His pupils, while previously non-reactive, had limited reactivity and he was able to see the outline of objects.
Pathological Diagnosis: Epidermoid Cyst with areas of poorly differentiated squamus cell carcinoma
Intracranial epidermoid cysts are benign, slow growing tumors which account for 0.2-1.8% of all intracranial tumors [1]. Malignant transformation is exceedingly rare, but may develop from existing lesions or following incomplete resection [2]. In known cases series, the interval from recognition of the benign cysts until malignant transformation ranged from 3 months to 33 years [2]. It is felt that the chronic inflammatory changes from repeated rupture of intracranial cysts may lead to malignant change [3]. Surgical treatment of squamus cell carcinoma arising from epidermoid cysts often is limited to partial removal given that the tumor capsule is often attached to critical structures. As a result, careful surgical debulking, followed by stereotactic radiosurgery with external beam radiotherapy has been encouraged [4,5].
Zachary A. Smith, M.D.,1,2 Colin Buchanan, M.D.1,2, and Duncan Q. McBride M.D.1,2
1-Division of Neurosurgery; Harbor-UCLA Medical Center; Los Angeles, CA.
2-Department of Neurosurgery, Ronald Reagan-UCLA Medical Center; Los Angeles, CA
Author Contact:
Zachary A. Smith
zsmith@mednet.ucla.edu
Ronald Reagan-UCLA Medical Center, UCLA Dept. of Neurosurgery
310-709-6405
References:
1. Ulrich J: Intracranial epidermoids, A study on their distribution and spread. J Neurosurg, 1964, 21: 1051-1058.
2. Tamura K, Aoyagi M, Wakimoto H, Tamaki M, Yamamoto K, Yamamoto M, Ohno K, Malignant transformation eight years after removal of a benign epidermoid cyst: A case report. J Neurooncol 2006, 79(1): 67-72.
3. Abramson RC, Morawetz RB, Schlitt M, Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery 1989, 24: 574-578.
4. Murase S, Yamakawa H, Ohkuma A, Sumi Y, Kajiwara M, Takami T, et al., Primary intracranial squamus cell carcinoma- case report. Neurol Med Chir (Tokyo) 1999, 39: 49-54.
5. Link MJ, Cohen PL, Breneman JC, Tew JM Jr, Malignant squamus degeneration of a cerebellopontine angle epidermoid tumor. Case report. J Neurosurg 2002, 97: 1237-1243.
Comments from the Editor-in-Chief:
This case represents a fundamental principle of medicine and neurosurgery regardless of what country in which one lives. The physicians in this case had presumed the diagnosis but had no proof for their opinion. The radiologists made the wrong diagnosis also. No radiologist or neurosurgeon or physician knows with 100% certainty what the TISSUE diagnosis is. Therefore, you must obtain a tissue diagnosis before you determine what the course of treatment will be. Yes, that also applies to brain stem, pineal or third ventricle or difficult lesions to reach. The patient must know the diagnosis in order to plan for his or her life. This patient would have been condemned to die by some physicians who assumed that the diagnosis was a malignant glioma. There was great resistance to operate on this patient. The end result confirms the principle that must never be forgotten. What is the proof for the diagnosis? That is the question the physician must answer and that the patient deserves the right to know.
James I. Ausman, MD, PhD Editor-in-Chief Surgical Neurology International






Sanjiv Natal
Posted June 18, 2010, 9:00 pm
In my country we would not have treated this patient. The cost is too high for not being able to give him a long life and he would probably live far from medical treatment
Mario Izurieta
Posted July 30, 2010, 8:37 pm
This is a great case. It teaches us that we must do our job based on evidence instead of beliefs. At first sight I would consider as a GBM, but in any case we would prefer to try a subtotal resection or temporal lobectomy, as soon as possible.