- Department of Orthopaedics, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, India.
- Department of Orthopaedics, Seth G.S Medical College and K.E.M Hospital, Mumbai, India.
- Department of Orthopaedics, Chaitanya Spine Clinic, Vasai, Maharashtra, India.
Correspondence Address:
Rudra Mangesh Prabhu, Department of Orthopaedics, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_247_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rudra Mangesh Prabhu1, Tushar N. Rathod2, Shubhranshu S. Mohanty2, Bhushan S. Hadole1, Nandan A. Marathe3, Abhishek K. Rai1. A case of cervical OPLL and DISH mimicking stroke. 22-Apr-2022;13:158
How to cite this URL: Rudra Mangesh Prabhu1, Tushar N. Rathod2, Shubhranshu S. Mohanty2, Bhushan S. Hadole1, Nandan A. Marathe3, Abhishek K. Rai1. A case of cervical OPLL and DISH mimicking stroke. 22-Apr-2022;13:158. Available from: https://surgicalneurologyint.com/surgicalint-articles/11557/
Abstract
Background: Ossification of the posterior longitudinal ligament (OPLL) is a progressive disorder that mostly involves the cervical spine. It is more prevalent in East Asian countries. Patients typically present with the gradual onset of myelopathy, while about 5% show rapid progression.
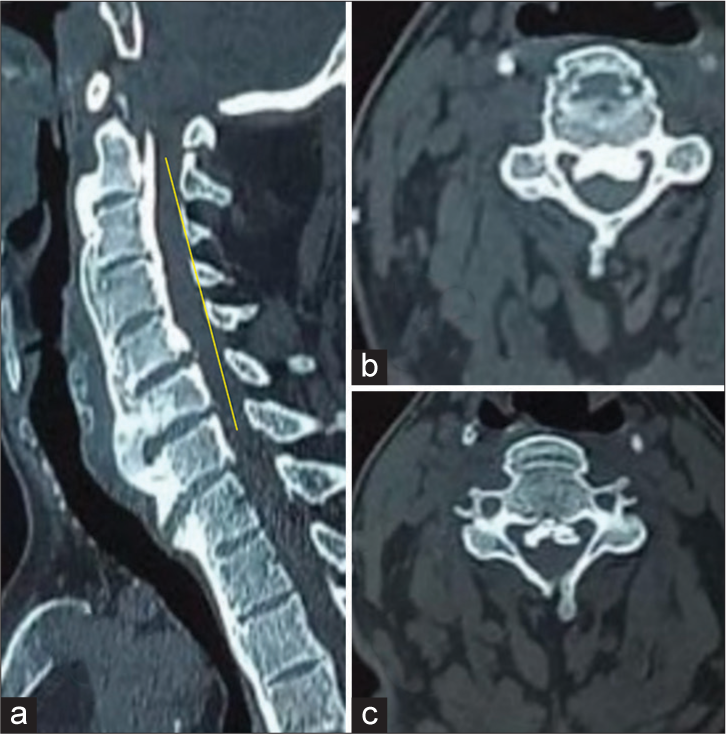
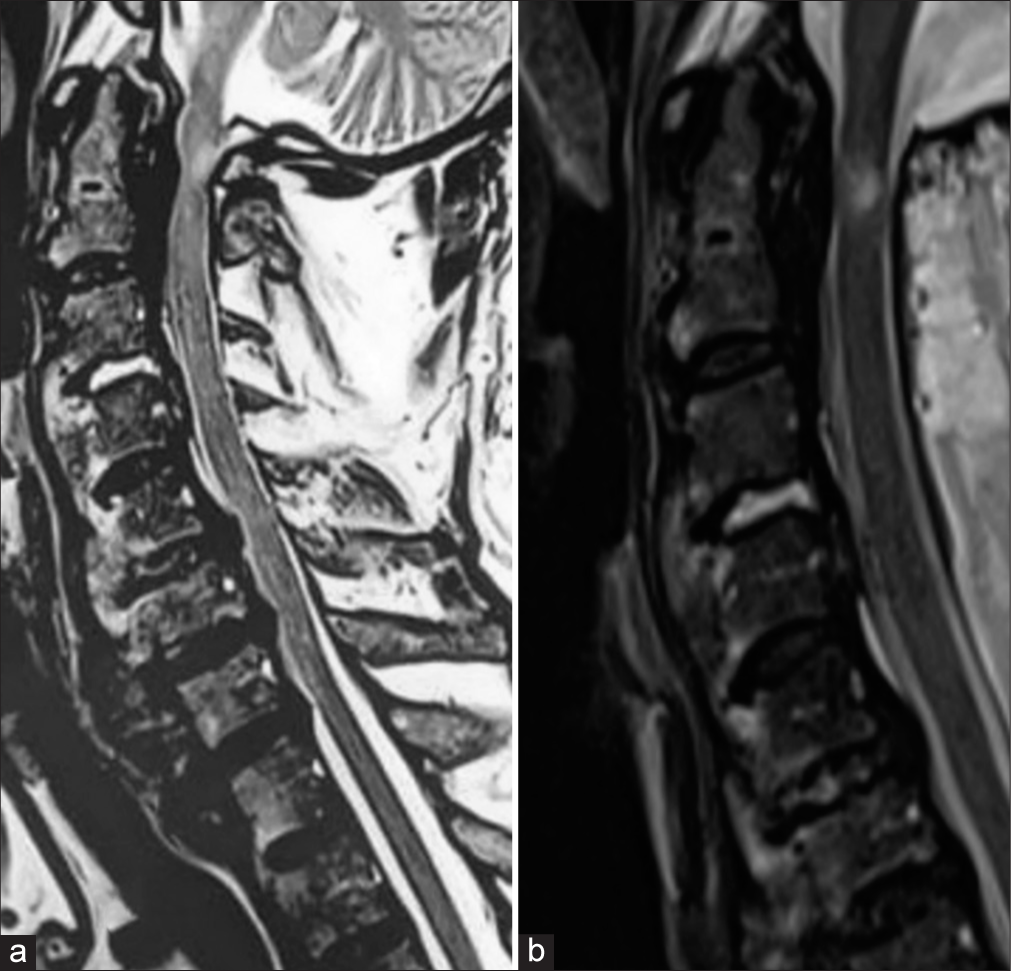
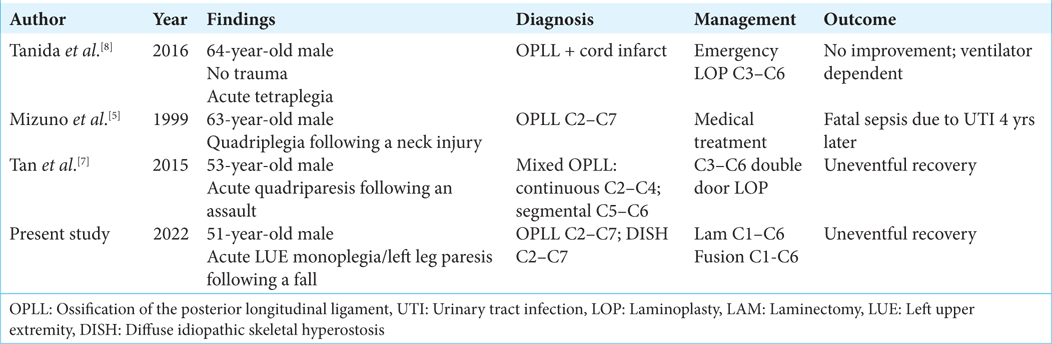
Case Description: A 51-year-old diabetic and hypertensive male presented with a left-sided hemiparesis following trivial trauma. The first diagnosis was a stroke, but the subsequent workup proved negative. Subsequently, the MRI and CT studies demonstrated significant cord compression due to OPLL extending from C2 to C7. There was also a heterogeneous hyperintense intramedullary cord signal indicative of edema/myelomalacia in the retro- odontoid region. The CT also diagnosed C2–C7 diffuse idiopathic skeletal hyperostosis.
Conclusion: Patients with cervical myelopathy due to OPLL rarely present about 5% of the time with the acute onset of neurological deficit following minor trauma. Certainly, one must consider high cervical OPLL as responsible for hemiparesis in a patient whose brain MR has ruled out a stroke.
Keywords: Cervical, DISH, Hemiparesis, Myelopathy, OPLL
INTRODUCTION
Cervical ossification of the posterior longitudinal ligament (OPLL) typically presents as a slowly progressive painless myelopathy. However, 5% of patients may develop rapid progression of a neurological deficit following even minor traumatic events.
CASE REPORT
Clinical data
A 51-year-old male acutely presented with what appeared to be a “left-sided hemiparesis” following a fall. The neurological examination showed severe left upper extremity monoplegia (0/5), sensory loss diffusely in the left arm, a mild left leg paresis (4/5 level), and bilateral hyperactive reflexes with Babinski responses in the lower extremities. The brain MR ruled out a stroke, while a lateral radiograph of the cervical spine showed both diffuse idiopathic skeletal hyperostosis (DISH) and OPLL [
Surgical technique
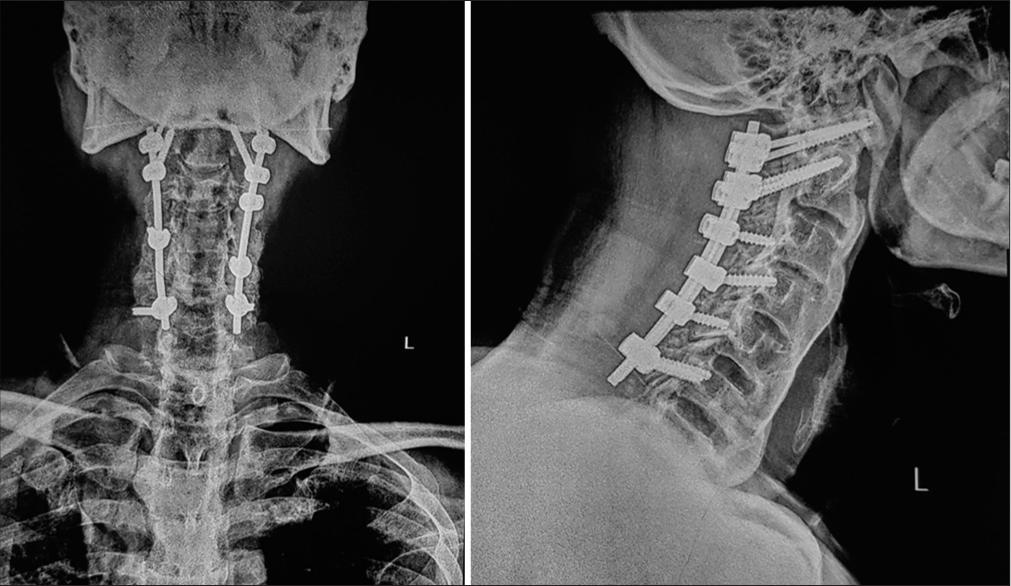
Due to the presence of a positive K-sign [
Figure 4:
(a) MRI at presentation demonstrating cord compression due to the OPLL mass with effacement of the anterior thecal sac. (b) MRI at a follow-up of 1 year showed improvement in the cord compression and a reduction in the myelomalacia cord changes. OPLL: Ossification of the posterior longitudinal ligament.
DISCUSSION
Using the positive or negative K-sign to determine whether anterior or posterior cervical surgery is warranted for OPLL
The positive and negative K-signs are typically utilized to determine whether anterior only or anterior, posterior, or circumferential cervical surgery can be performed to address OPLL and any other pathology. The K-line is drawn vertically from the midpoint of the C2 spinal canal to the midpoint of the C7 spinal canal; if, as in this case, the ventral OPLL mass falls anterior to this line, this constitutes a positive K-sign, and anterior or posterior cervical surgery may be performed. Alternatively, the negative K-sign is present when the ventral OPLL mass extends posterior to the vertical line, thus largely dictating that an anterior cervical approach is warranted, typically a corpectomy rather than a diskectomy.[
Canal occupying ratio influencing surgical approaches: an additional “Check” on the K-signs
A systematic review of the literature indicates that although the anterior approach is associated with more surgical complications, it is preferred where the canal-occupying ratio is >50–60%. On the contrary, the posterior approach has fewer complications and is recommended when the canal-occupying ratio is <50–60%.[
Role of fusion with OPLL
Multiple studies report better results if cervical OPLL is treated with both decompression and fusion. Fusion accelerates recovery and slows/eliminates the rate of OPLL progression.[
5% incidence of acute deterioration seen in OPLL
Around 75% of patients with OPLL deteriorate in a step-wise manner, 20% worsen slowly, while 5% present with acute neurological worsening[
CONCLUSION
Once the brain MR ruled out a stroke, our patient’s acute left hemiparesis was attributed to both MR/CT documented cervical OPLL extending from C2 to C7 that warranted a posterior cervical decompression with fusion.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Clarke E, Robinson PK. Cervical myelopathy: A complication of cervical spondylosis. Brain. 1956. 79: 483-510
2. Feng F, Ruan W, Liu Z, Li Y, Cai L. Anterior versus posterior approach for the treatment of cervical compressive myelopathy due to ossification of the posterior longitudinal ligament: A systematic review and meta-analysis. Int J Surg. 2016. 27: 26-33
3. Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976). 2008. 33: E990-3
4. Mehdi SK, Alentado VJ, Lee BS, Mroz TE, Benzel EC, Steinmetz MP. Comparison of clinical outcomes in decompression and fusion versus decompression only in patients with ossification of the posterior longitudinal ligament: A meta-analysis. Neurosurg Focus. 2016. 40: E9
5. Mizuno J, Nakagawa H, Hashizume Y. Pathology of the spinal cord damaged by ossification of the posterior longitudinal ligament associated with spinal cord injury. Spinal Cord. 1999. 37: 224-7
6. Sugrue PA, McClendon J, Halpin RJ, Liu JC, Koski TR, Ganju A. Surgical management of cervical ossification of the posterior longitudinal ligament: Natural history and the role of surgical decompression and stabilization. Neurosurg Focus. 2011. 30: E3
7. Tan WQ, Wong BS. Clinics in diagnostic imaging (161). Cervical OPLL with cord compression. Singapore Med J. 2015. 56: 373-8
8. Tanida A, Kamimura A, Tanishima S, Mihara T, Takeda C, Nagashima H. Spinal cord infarction at the level of ossification of the posterior longitudinal ligament. Spinal Cord Ser Cases. 2016. 2: 16032