- Department of Neurosurgery, Dokkyo Medical University Saitama Medical Center, Koshigaya-Shi, Saitama-Ken, Japan.
Correspondence Address:
Issei Takano, Department of Neurosurgery, Dokkyo Medical University Saitama Medical Center, Koshigaya-Shi, Saitama-Ken, Japan.
DOI:10.25259/SNI_322_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Issei Takano, Tomoji Takigawa, Kei Shimmyo, Toru Anazawa, Takahiro Kanaya, Yoshiko Fujii, Yasuhiko Nariai, Yoshiki Sugiura, Ryotaro Suzuki, Masaya Nagaishi, Akio Hyodo, Kensuke Suzuki. A case of cribriform plate dural arteriovenous fistulas with a rare complication after endovascular therapy. 20-May-2022;13:216
How to cite this URL: Issei Takano, Tomoji Takigawa, Kei Shimmyo, Toru Anazawa, Takahiro Kanaya, Yoshiko Fujii, Yasuhiko Nariai, Yoshiki Sugiura, Ryotaro Suzuki, Masaya Nagaishi, Akio Hyodo, Kensuke Suzuki. A case of cribriform plate dural arteriovenous fistulas with a rare complication after endovascular therapy. 20-May-2022;13:216. Available from: https://surgicalneurologyint.com/surgicalint-articles/11599/
Abstract
Background: Cribriform plate dural arteriovenous fistulas (dAVFs) are rarely encountered. Here, we report a case of cribriform plate dAVF with a rare complication after endovascular therapy.
Case Description: A 60-year-old man presented with severe sudden headache. Head computed tomography showed right subdural hematoma, and magnetic resonance angiography showed dilated bilateral frontal cortical vein. Digital subtraction angiography revealed cribriform plate dAVF fed by the anterior and posterior ethmoidal branches of the bilateral ophthalmic arteries. Transarterial embolization with liquid embolic material was performed and the fistula disappeared. Although magnetic resonance imaging showed the disappearance of the cribriform plate dAVF and subdural hematoma, the patient complained of anosmia after the procedure.
Conclusion: Endovascular embolization is an effective treatment option for treating cribriform plate dAVFs. However, anosmia is a possible complication, and endovascular surgeons should take care of this complication, especially in cribriform plate dAVFs supplied with blood bilaterally.
Keywords: Case report, Endovascular procedures, Ethmoid bone, Hematoma
INTRODUCTION
Cribriform plate dural arteriovenous fistulas (dAVFs) are rarely encountered. The incidence of cribriform plate dAVF is 1–1.5% of intracranial vascular malformations.[
Surgical resection of the fistula is the gold standard approach for treating this disease. Recently, some studies have reported on the efficacy and safety of endovascular embolization for cribriform plate dAVFs. Endovascular embolization is less invasive and is considered safe if the microcatheter is navigated close to the fistula. However, data on the complications of endovascular treatment for these lesions are limited. Thus, here, we present a rare complication after endovascular therapy for cribriform plate dAVF.
CASE PRESENTATION
Clinical history
A 60-year-old man presented with severe sudden headache. The patient had no history of head injury and chronic headache, such as migraine or cluster headache. The patient received regular medications for hypertension and hyperlipidemia. No neurological deficits were observed on general physical examinations.
Imaging findings
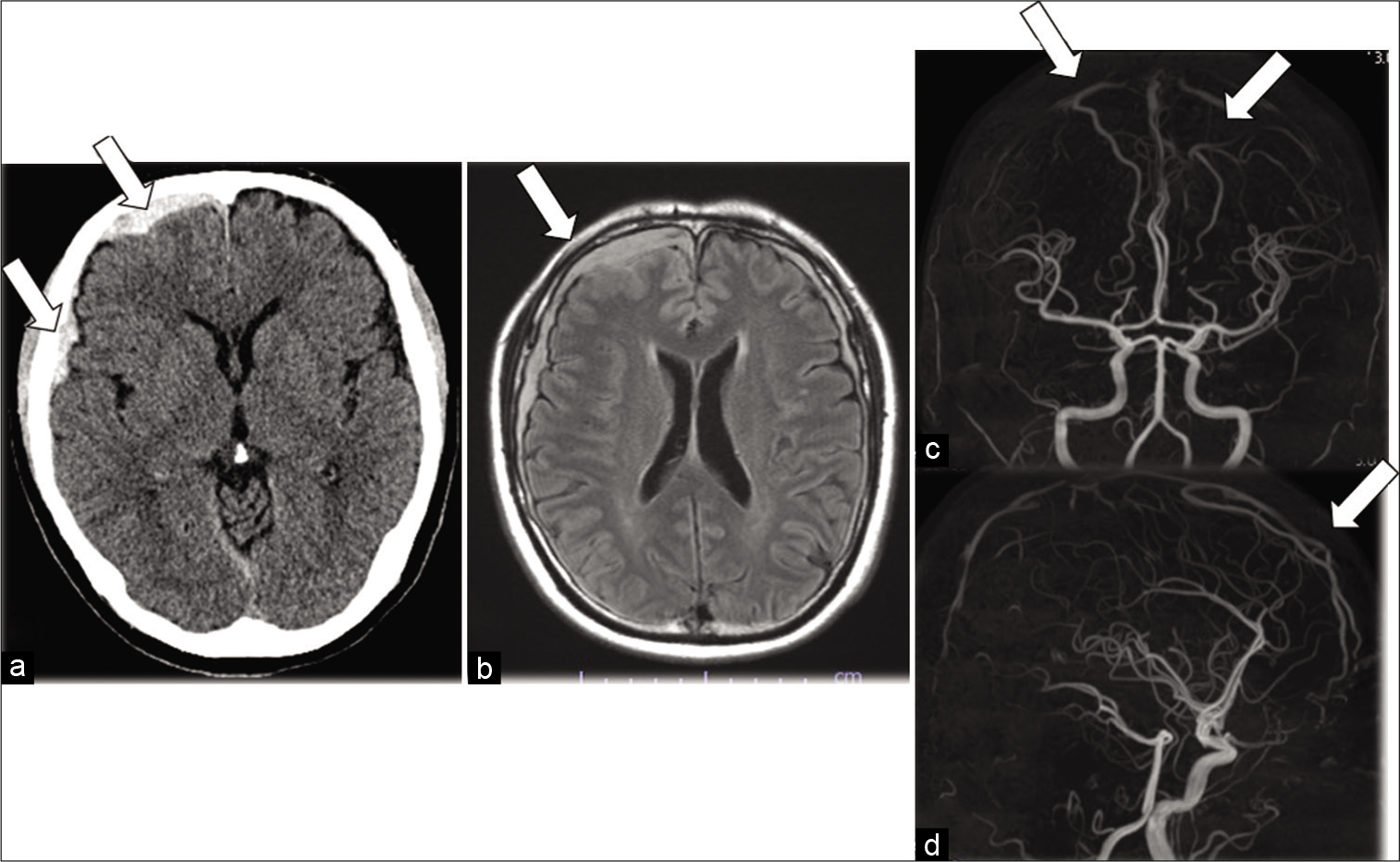
Head computed tomography (CT) and magnetic resonance imaging showed the right subdural hematoma. Magnetic resonance angiography showed bilateral dilated frontal cortical vein [
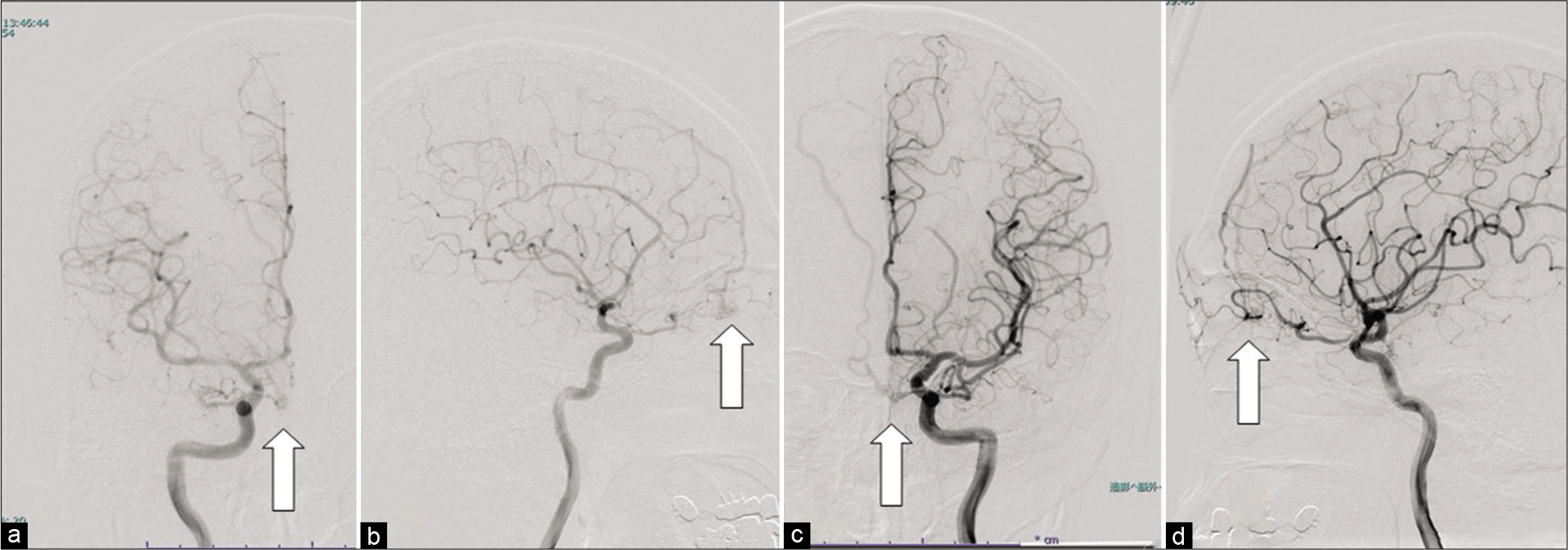
Digital subtraction angiography showed dAVF in the bilateral frontal region supplied by the anterior and posterior ethmoidal branches of the bilateral ophthalmic arteries [
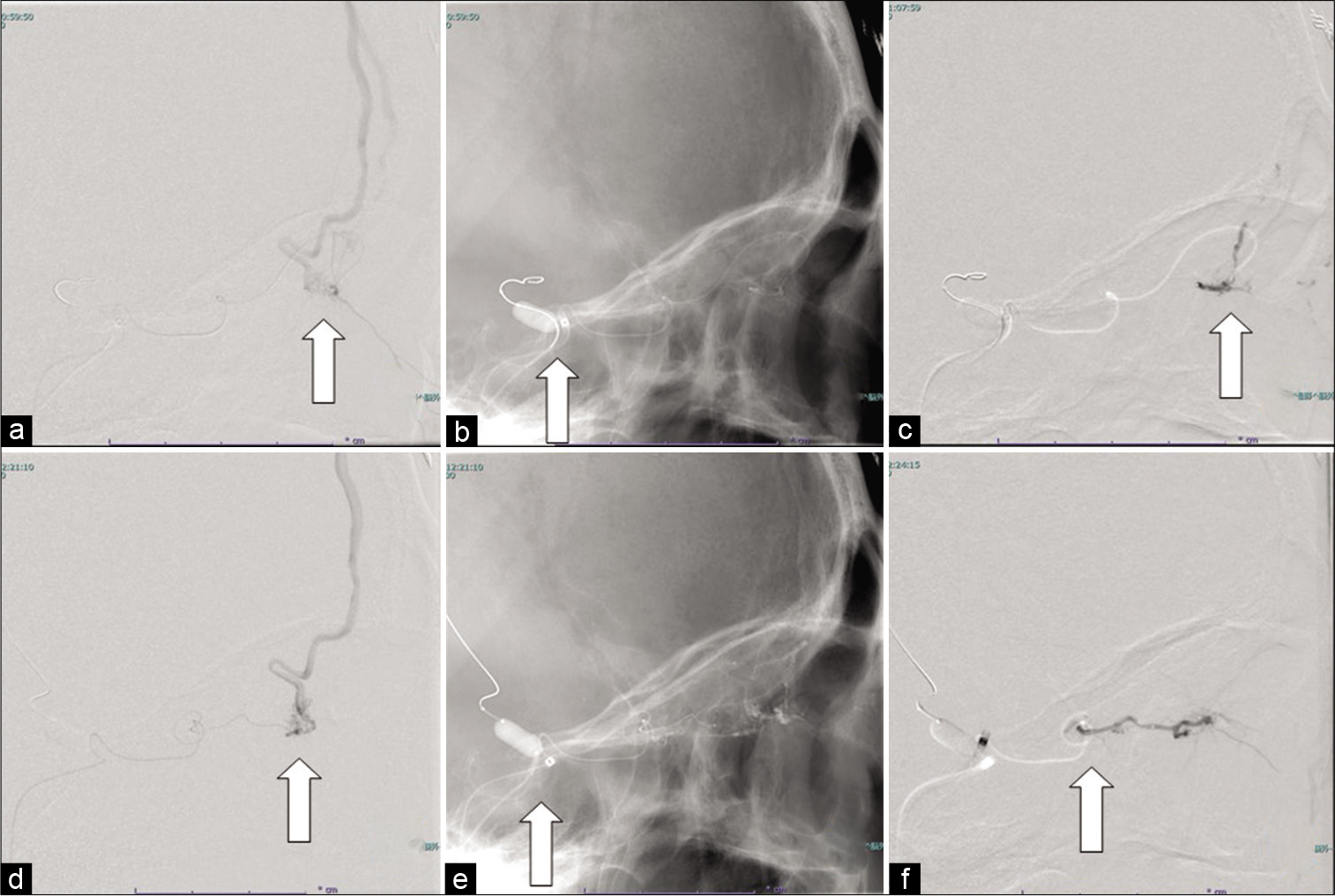
To prevent rebleeding, endovascular therapy was planned. The patient was informed of our therapeutic strategy. When it was difficult to perform safe endovascular therapy, surgery was considered. Under general anesthesia, a 7-Fr guiding sheath (Shuttle, Cook, Bloomington, Indiana, USA) was placed on the origin of the left cervical internal carotid artery. Scepter XC 4 mm/11 mm (MicroVention-Terumo, Tusin, CA, USA) was placed distal to the ophthalmic artery origin because selectively catheterizing DeFrictor (MEDICO’S Hirata, Osaka, Japan) and CHIKAI10 (Asahi Intec, Aichi, Japan) were difficult. After DeFrictor was placed close to the fistula, control contrast injections were performed to confirm the safe position of DeFrictor distal to the origin of the central retinal arteries and no dangerous anastomosis. Then, 20% N-butyl cyanoacrylate (NBCA) diluted with oily contrast medium was infused into the fistula under road map guidance not to reflux and migrate the ophthalmic artery. Although complete occlusion from the left ophthalmic artery was achieved, feeders from the right ophthalmic artery remained. Embolization with 20% NBCA from the feeder of the right ophthalmic artery was performed using the same method used on the left side. Finally, the control contrast injection in both internal carotid arteries showed complete fistula occlusion [
Figure 3:
(a) Lateral view of a selective injection of the left ophthalmic artery presenting a fistula (arrow). (b) Scepter XC was placed distal to the internal carotid artery to stabilize the guiding catheter and microcatheter (arrow). (c) 20% N-butyl cyanoacrylate (NBCA) diluted with oily contrast medium was infused into the fistula (arrow). (d) Lateral view of a selective injection of the right ophthalmic artery presenting a fistula (arrow). (e) Scepter XC was placed distal to the internal carotid artery to stabilize guiding catheter and microcatheter (arrow). (f) 20% NBCA diluted with oily contrast medium was infused into the fistula (arrow).
One day after the procedure, the patient complained of anosmia. To evaluate olfactory function in this patient, the Alinamin F test was performed and revealed that the patient had an impaired sense of smell.
On the 7th day after the procedure, angiography did not reveal recanalization of the fistula. The patient was discharged 1 month after with anosmia only.
DISCUSSION
Because cribriform plate dAVFs are characterized by a high risk of fatal intracranial hemorrhage due to their cortical venous drainage, almost all patients will be treated with surgical or endovascular therapy. Surgical resection is effective because cribriform plate dAVFs are comparatively located in a surface layer, and fistula can be directly resected. However, surgical treatment is associated with complications related to frontal craniotomy, such as anosmia. Endovascular therapy leads to a high rate of angiographic cure and lower complication rates, but anosmia as a complication has never been reported.[
We speculated that anosmia has two main causes. First, we thought that anosmia was associated with ischemia. Blood supply to the olfactory nerve is associated with the olfactory, accessory olfactory, anterior ethmoidal, and posterior ethmoidal arteries. Functionally, these arteries are end arteries without anastomoses.[
However, a study has reported that subarachnoid hemorrhage is a sufficient factor for developing loss of smell. In the patient in this case report, head CT showed a subdural hematoma, but anosmia occurred after endovascular embolization. Therefore, this hemorrhage is probably associated with anosmia.
CONCLUSION
Endovascular embolization for cribriform plate dAVFs is effective. Especially, in the case of embolization for bilateral ophthalmic arteries, anosmia is a possible complication.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S. Dural arteriovenous shunts: A new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke. 2008. 39: 2783-94
2. Hendrix P, Griessenauer CJ, Foreman P, Shoja MM, Loukas M, Tubbs RS. Arterial supply of the upper cranial nerves: A comprehensive review. Clin Anat. 2014. 27: 1159-66
3. Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg. 1986. 64: 724-30
4. Li C, Wu Z, Yang X, Li Y, Jiang C, He H. Transarterial treatment with Onyx of Cognard Type IV anterior cranial fossa dural arteriovenous fistulas. J Neurointerv Surg. 2014. 6: 115-20
5. Li Q, Fang YB, Huang QH, Zhang Q, Hong B, Zhao WY. Transarterial embolization of dural arteriovenous fistulas of the anterior cranial fossa with Onyx. J Clin Neurosci. 2013. 20: 287-91
6. Mack WJ, Gonzalez NR, Jahan R, Vinuela F. Endovascular management of anterior cranial fossa dural arteriovenous malformations. A technical report and anatomical discussion. Interv Neuroradiol. 2011. 17: 93-103
7. Martin NA, King WA, Wilson CB, Nutik S, Carter LP, Spetzler RF. Management of dural arteriovenous malformations of the anterior cranial fossa. J Neurosurg. 1990. 72: 692-7
8. Newton TH, Cronqvist S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology. 1969. 93: 1071-8
9. Xu K, Ji T, Li C, Yu J. Current status of endovascular treatment for dural arteriovenous fistulae in the anterior cranial fossa: A systematic literature review. Int J Med Sci. 2019. 16: 203-11