- Department of Orthopaedics, J. N. Institute of Medical Sciences, Imphal East, Manipur, India.
- Department of Pathology, J. N. Institute of Medical Sciences, Imphal East, Manipur, India.
DOI:10.25259/SNI_469_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Umesh Takhelmayum1, Namjubou Daimai1, Kanchana Laishram1, Nikhil Juneja1, M. L. Yogananda1, Deepa Longjam2. A case of postoperative tubercular spondylitis following microdiscectomy for lumbar disc herniation. 07-Jun-2021;12:265
How to cite this URL: Umesh Takhelmayum1, Namjubou Daimai1, Kanchana Laishram1, Nikhil Juneja1, M. L. Yogananda1, Deepa Longjam2. A case of postoperative tubercular spondylitis following microdiscectomy for lumbar disc herniation. 07-Jun-2021;12:265. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10862
Abstract
Background: Postoperative infections are one of the most common complications of spine surgery. However, following a lumbar microdiscectomy, a postoperative infection involving Mycobacterium tuberculosis (MTB) is extremely rare.
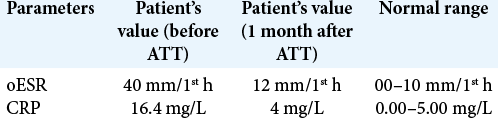
Case Description: One and half months after a L4-5 microdiscectomy, a 47-year-old immunocompromised male with hepatitis B infection presented with low back and bilateral gluteal pain. The MRI revealed a large intraspinal/paraspinal fluid collection spanning from L4 to S1 along with an anterior epidural collection at L5. The patient underwent a L4 lumbar laminectomy for abscess drainage and wound debridement. After obtaining a positive culture for MTB, four antitubercular drug therapies (ATTs) were started, that is, isoniazid (H), rifampicin (R), ethambutol (E), a. One month later, the patient had minimal pain and no residual neurological deficit.
Conclusion: MTB infection, although rare, should be considered among the differential diagnoses of postoperative infections following lumbar spine surgery in immunocompromised patients living in areas where tuberculosis is endemic.
Keywords: Antitubercular drugs, Microdiscectomy, Spine, Tuberculosis
INTRODUCTION
Most postoperative spine infections are bacterial, and majority are attributed to Staphylococcus aureus.[
CASE REPORT
A 47-year-old hepatitis B positive male underwent L4-L5 microdiscectomy 45 days ago. He newly presented with low back and bilateral gluteal pain (i.e., VAS score 8 and 5 respectively) and swelling under the surgical scar. The lumbar ultrasound showed a deep dorsal paraspinal collection extending from L3 to L5 in the subcutaneous and intramuscular region. The MRI additionally revealed diffused vertebral body edema with a large intraspinal/ paraspinal and anterior epidural fluid collection from L4 to S1 [
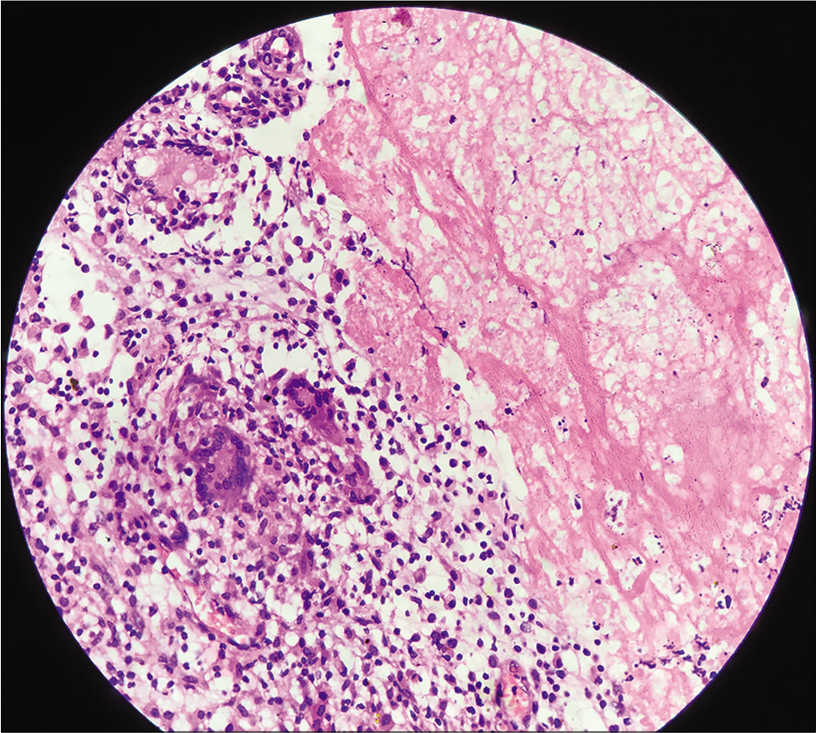
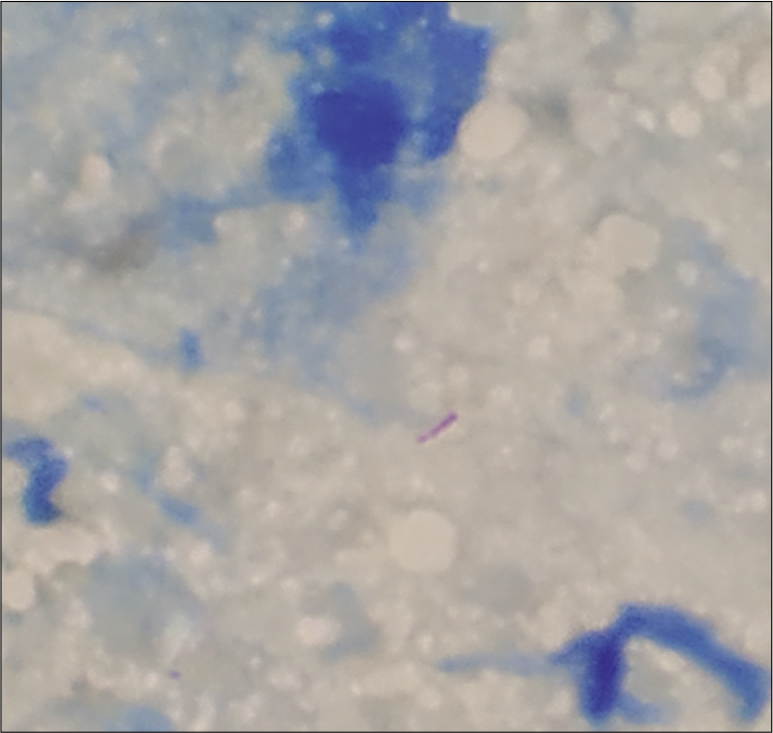
The histopathological report showed epithelioid cell granulomas with central caseation surrounded by Langhans type giant cells [
The plan was to continue the four drugs for 2 months followed by a three drugs (HRE) regimen for another 10 months.
DISCUSSION
It is important to include MTB infection among the differential diagnoses for postoperative spinal infections in areas where tuberculosis is endemic and patients are immunocompromised. We identified six similar cases in the literature so far.[
CONCLUSION
In areas where tuberculosis is endemic, immunocompromised patients undergoing lumbar discectomy may develop postoperative MTB infections.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Babafemi EO, Cherian BP, Banting L, Mills GA, Ngianga K. Effectiveness of real-time polymerase chain reaction assay for the detection of Mycobacterium tuberculosis in pathological samples: A systematic review and meta-analysis. Syst Rev. 2017. 6: 215
2. Celik SE. Pott disease mimics postsurgical pyogenic spondylodiscitis. J Neurosurg Sci. 2009. 53: 161-4
3. Dulani R, Shrivastava S, Singh P. A rare case report: Tubercular spondylodiscitis following lumbar disc surgery. Asian Pac J Trop Med. 2010. 3: 496-8
4. Ivo R, Sobottke R, Seifert H, Ortmann M, Eysel P. Tuberculous spondylitis and paravertebral abscess formation after kyphoplasty: A case report. Spine (Phila Pa 1976). 2010. 35: E559-63
5. Jeon DW, Chang BS, Jeung UO, Lee SJ, Lee CK, Kim MS. A case of postoperative tuberculous spondylitis with a bizarre course. Clin Orthop Surg. 2009. 1: 58-62
6. Kang JH, Kim HS, Kim SW. Tuberculous spondylitis after percutaneous vertebroplasty: Misdiagnosis or complication?. Korean J Spine. 2013. 10: 97-100
7. Lv Z, Zhang M, Zhang H, Lu X. Utility of real-time quantitative polymerase chain reaction in detecting Mycobacterium tuberculosis. Biomed Res Int. 2017. 2017: 1058579
8. Ozger O, Kaplan N. Tuberculous spondylodiscitis after lumbar microdiscectomy. J Coll Physicians Surg Pak. 2020. 30: 983-6
9. Park DY, Kim JY, Choi KU, Lee JS, Lee CH, Sol MY. Comparison of polymerase chain reaction with histopathologic features for diagnosis of tuberculosis in formalin-fixed, paraffin-embedded histologic specimens. Arch Pathol Lab Med. 2003. 127: 326-30