- Department of Orthopedic Surgery, Madras Institute of Orthopedics and Traumatology (M.I.O.T) International, Chennai, Tamil Nadu, India.
- Department of Neurosurgery, Madras Institute of Orthopedics and Traumatology (M.I.O.T) International, Chennai, Tamil Nadu, India.
- Department of Pathology, Madras Institute of Orthopedics and Traumatology (M.I.O.T) International, Chennai, Tamil Nadu, India.
Correspondence Address:
Hrishikesh Sarkar, Director of Department of Neurosurgery, Madras Institute of Orthopedics and Traumatology (M.I.O.T) International, Chennai, Tamil Nadu, India.
DOI:10.25259/SNI_47_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prithvi Mohandas1, Hrishikesh Sarkar2, Deepti Jain3, Vanaja Kate Garfin Sundaram2. A case report of conus intramedullary mansoni neuroschistosomiasis. 21-Apr-2023;14:139
How to cite this URL: Prithvi Mohandas1, Hrishikesh Sarkar2, Deepti Jain3, Vanaja Kate Garfin Sundaram2. A case report of conus intramedullary mansoni neuroschistosomiasis. 21-Apr-2023;14:139. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12284
Abstract
Background: Conus schistosomiasis is an extremely rare entity in which patients present with a wide range of neurological symptoms such as low back pain, paresthesia, fever, myalgia, paraparesis, and paraplegia. This neglected tropical parasitic disease causes significant neurological morbidity. The migration of parasitic worms and their eggs into the central nervous system can lead to profound and life-altering disabilities. Early, accurate diagnosis, and treatment can lead to the complete resolution of symptoms.
Case Description: A 5-year-old boy from South Sudan presented with complaints of sudden onset, progressive bilateral lower limb weakness for the past month, inability to walk or stand without assistance, and urinary incontinence. Magnetic resonance imaging spine showed an irregular enhancing lesion within the conus. The various possibilities, such as Astrocytoma, and granulomatous disorders were considered. However, a biopsy revealed the lesion to be Conus schistosomiasis, a rare condition with only a few cases reported in children. Typical clinicoradiological presentation and the treatment paradigm have been discussed in this manuscript. Appropriate management of this lesion can avert surgical intervention needed for either a diagnosis or treatment.
Conclusion: This case report aims to emphasize the importance of considering schistosomiasis as an important differential diagnosis of a conus intramedullary lesion, especially in patients from tropical endemic countries. The neurological recovery in this infestation is directly related to early diagnosis and treatment. Therefore, it is essential to recognize this entity, as early detection and management would result in significant neurological improvement without undergoing surgery.
Keywords: Conus intramedullary schistosomiasis, Schistosoma mansoni, Schistosomal myeloradiculopathy, Schistosomiasis, Spinal neuroschistosomiasis
INTRODUCTION
Neuroschistosomiasis is an unacknowledged, rare disease affecting between 1% and 4% of the estimated 200–300 million people with systemic schistosomal infections.[
CASE PRESENTATION
A 5-year-old boy from South Sudan presented with complaints of sudden onset, progressive bilateral lower limb weakness for the past month, and inability to walk or stand without assistance. Before the onset of symptoms, he could walk and run without support. He has had urinary incontinence since the onset of weakness. He had experienced a few episodes of fever and cough for the past month. His prior medical history did not reveal any other clinical comorbidity. The family was from a peri-urban area of South Sudan known for its endemic intestinal and urogenital schistosomiasis, particularly with Schistosoma mansoni species.
On examination, he was noted to have grade 2 weakness of the lower limbs, right more than left. He could not stand and sit without support but could roll over in bed and had areflexia, which involved absent knee, ankle and plantar reflexes. He was also observed to have no cremasteric reflex, lax anal tone, and neurogenic bladder.
MRI of the brain with the whole spine showed an intramedullary lesion extending from D11 to L1 with irregular margins in conus medullaris and perilesional edema [
Figure 1:
Preoperative magnetic resonance images (a). Axial section T1-weighted, (b). sagittal T1 sequence, (c). sagittal T2-weighted (T2W), and (d). post-contrast sagittal with IV contrast of Gadovist showing heterogeneously enhancing intramedullary lesion D11–L1 level with poorly defined margins in the conus medullaris with expansion and abnormal enhancement of the dorsal and ventral rami at L1 level with perilesional edema. (c) Sagittal T2W showed a typical “String of Bead” appearance due to multiple enhancing nodules within the conus associated with interlacing and matting. Copyright 2022 by MIOT International Hospitals, Chennai.
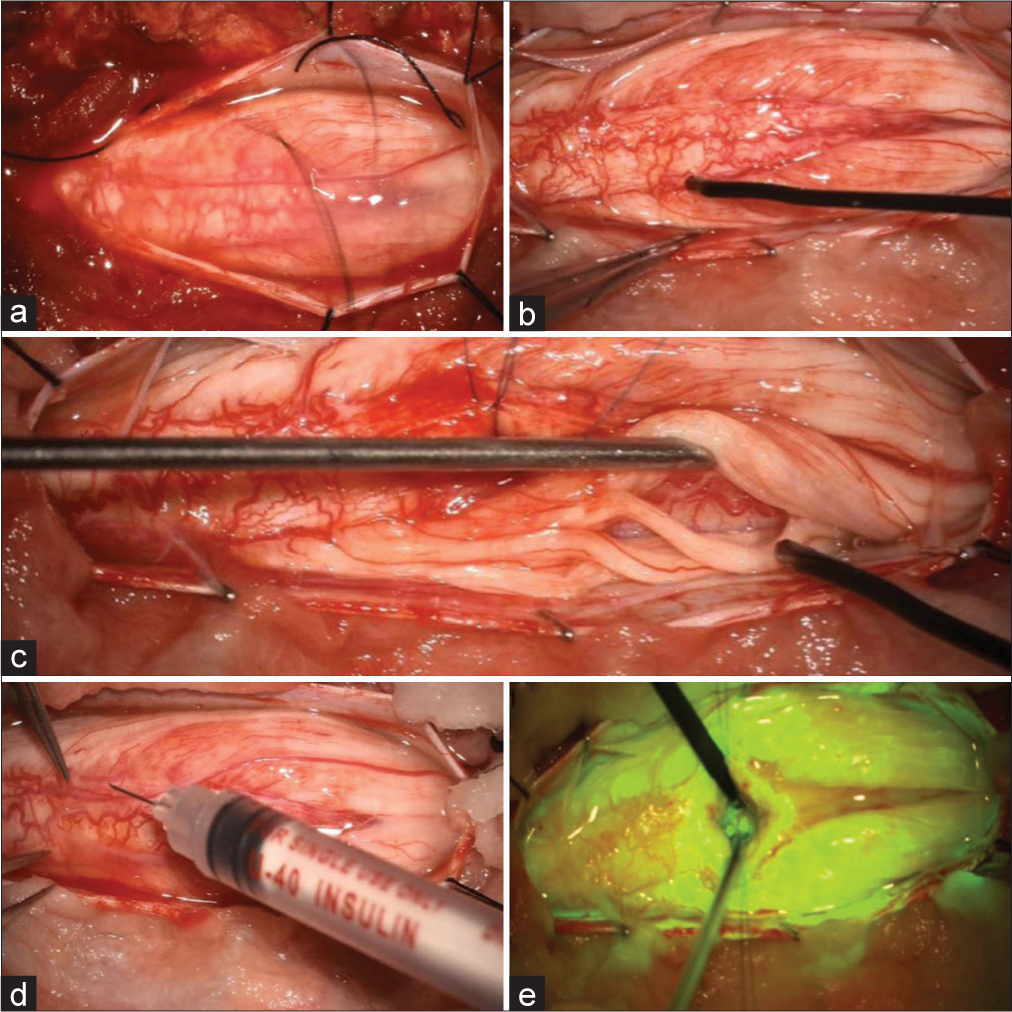
Urine and stool routine examinations were done to observe viable Schistosoma eggs, which were reported negative. Serum angiotensin converting enzyme (ACE) level was done to rule out Sarcoidosis, which was noted to be within normal limits. Serum neuromyelitis optica (NMO) and myelin oligodendrocyte glycoprotein (MOG) levels were done to rule out immune-mediated disorders, Brucella antibodies IgG/IgM to rule out brucellosis and immunoblot antinuclear antibody (ANA) profile to rule out antinuclear antibody-positive disease were reported negative. Systemic involvement of schistosomiasis was ruled out as well. Since there was no definitive diagnosis, a surgical biopsy was contemplated, and therefore, he underwent a laminoplasty proceed biopsy under intraoperative neuromonitoring, C-arm, and fluorescein guidance. Intraoperatively, the edematous and inflamed nerve roots were noted, along with an intramedullary conus lesion [
Figure 2:
Intraoperative images (a) edematous and inflamed root, (b) electrode placed after sectioning, (c) exploration of the nerve roots on the left side, (d) dorsal myelotomy performed, and (e) microscopic vision under fluorescein dye. Copyright 2022 by MIOT International Hospital, Chennai. Copyright 2022 by MIOT Internatinoal Hospital, Chennai.
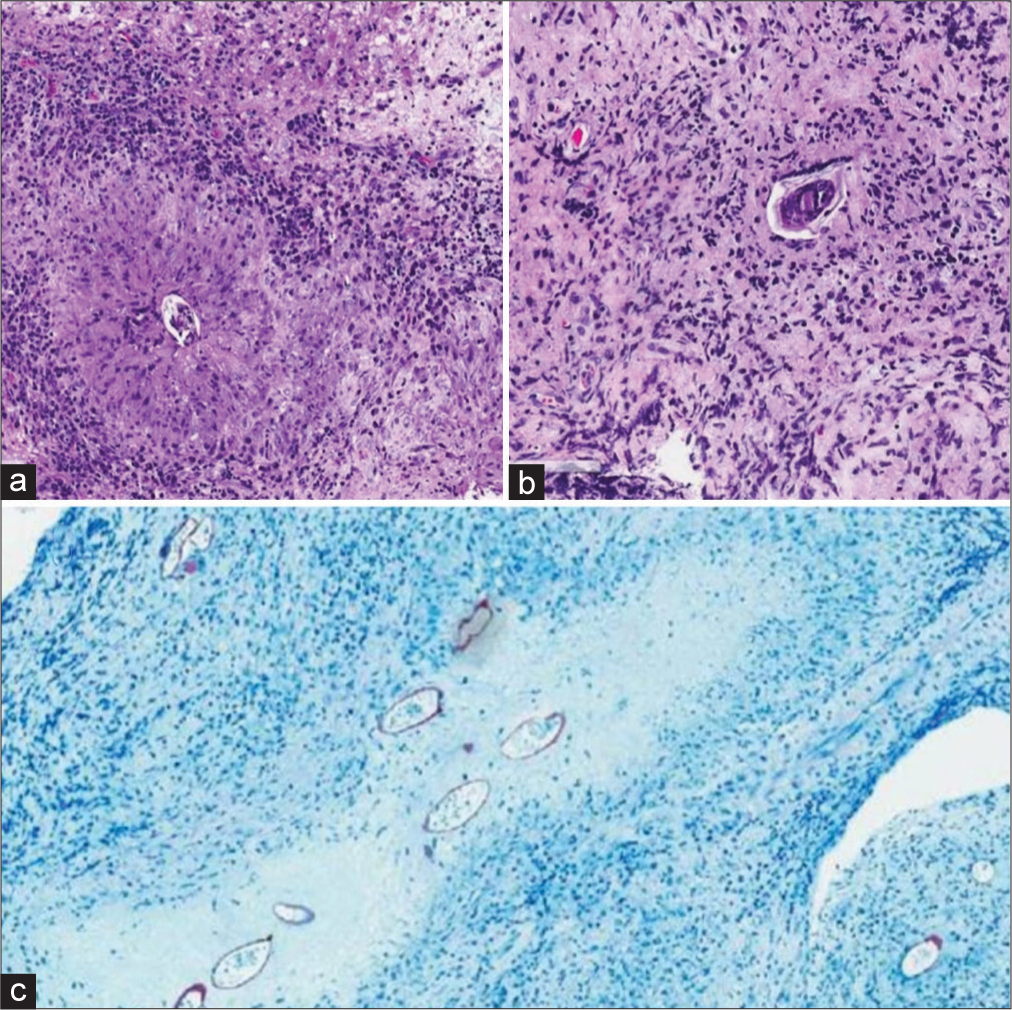
Histopathological examination of the spinal cord lesion showed necrotising granulomatous chronic inflammation with Schistosoma eggs and no evidence of malignancy [
Figure 3:
Histopathological images. (a) The high-power section of Schistosoma eggs, (b) low-power Schistosoma eggs with multinucleated cells showing inflammatory reaction to the egg, and (c) modified Ziehl–Neelsen staining showing Schistosoma eggs. Copyright 2022 by MIOT International Hospital, Chennai.
Postoperatively, he was given regular intensive in-house rehabilitation and physiotherapy. Before his discharge, he became well ambulant and had gross improvement in the power of his lower extremities, the tone of the anal sphincter improved, and he was voiding well by himself. The postoperative MRI scan showed decreased conus swelling and decreased enhancement in the residual conus medullaris lesion with edema cranial to the conus medullaris completely resolved [
Figure 4:
Postoperative magnetic resonance images (a). Axial T2-weighted, (b). sagittal T1-weighted (T1W), and (c). sagittal T1W shows a decrease in conus swelling and decreased enhancement in the residual conus medullaris lesion with edema cranial to the conus medullaris completely resolved. Copyright 2022 by MIOT International Hospital, Chennai.
DISCUSSION
Neursochistosmiasis is a neglected and unacknowledged complication of Schistosomiasis infesting the central nervous system by the Schistosoma species, which can provoke severe neurological disability due to the consequence of an immune reaction.
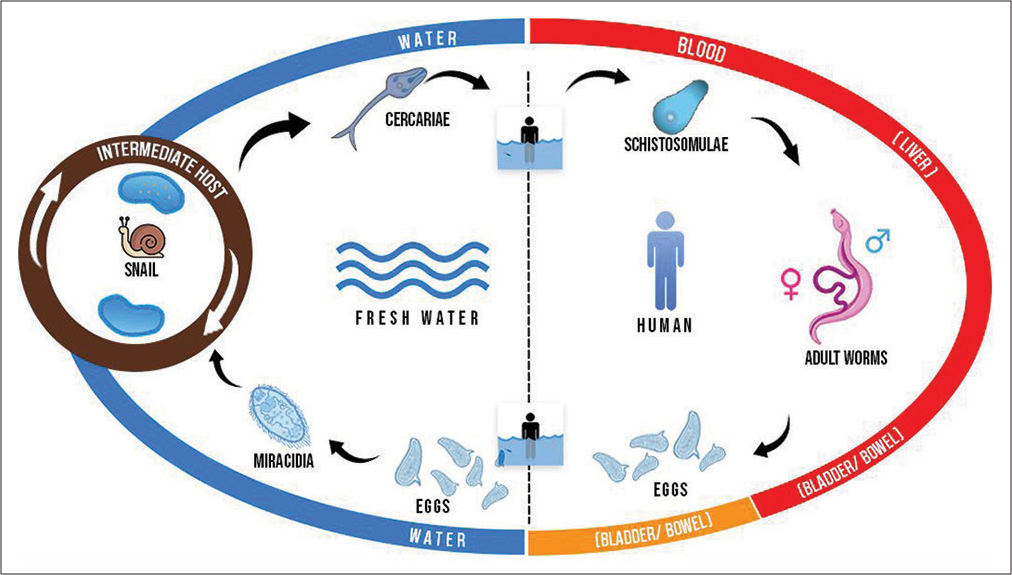
The parasite’s ovum is passed in infected individuals’ urine or feces, contaminating fresh water, where ciliated miracidium is liberated and enters the intermediate host, a species of freshwater snails, where it multiplies [
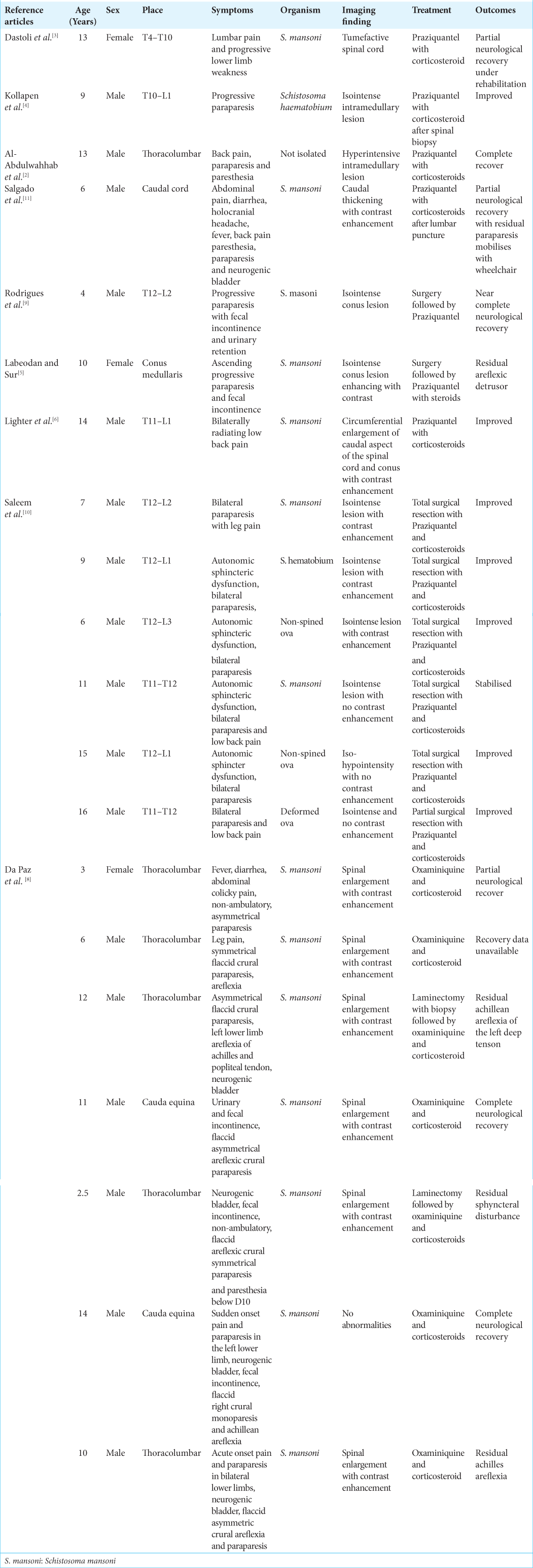
LITERATURE REVIEW OF SPINAL SCHISTOSOMIASIS IN CHILDREN
As noted with the children reported in the literature, our patient also belonged to this particular endemic region and demonstrated classical clinicoradiological findings [
The ideal way to manage this disease would need a high index of suspicion and early institution of anti-helminthic therapy.[
The available evidence and our case can further help advance the knowledge about the spinal manifestation of neuroschistosomiasis, emphasizing its early diagnosis and intervention. As observed in our case, the typical clinical manifestations and radiological findings of “String of Beads” may avoid diagnostic surgical intervention. This will reduce the time for initiation of appropriate anti-parasitic medications and steroids, leading to favorable outcomes.
CONCLUSION
This manuscript provides additional insights into the rare diagnosis of spinal neuroschistosomiasis, which is associated with significant neurological morbidity. Early diagnosis and treatment can improve neurological outcomes. In the presence of characteristic imaging findings, empirical treatment may be warranted to avoid surgical intervention and provide favorable results. This article adds to the importance of awareness of this rare entity in the list of differential diagnoses of conus lesions.
Ethics approval and consent to participate
This manuscript has been reported post approval from the ethics committee of MIOT international and consent from the child’s parents.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adeel AA. Spinal cord schistosomiasis. Sudan J Paediatr. 2015. 15: 23-8
2. Al-Abdulwahhab AH, Al-Sharydah AM, Al-Suhibani SS, Al-Jubran SA, Al-Hailey AK, Al-Hifzi AI. Neuroschistosomiasis mimicking lower back pain: Case report of a rare differential diagnosis in a pediatric patient. Patient Saf Surg. 2018. 12: 28
3. Dastoli PA, Leite AL, da Costa MD, Nicácio JM, Pinho RS, Ferrarini MA. Medullary neuroschistosomiasis in adolescence: Case report and literature review. Childs Nerv Syst. 2021. 37: 2735-41
4. Kollapen K, Suleman FE, Smuts I, Siwela L. Medullary neuroschistosomiasis in a pediatric patient: A case report. Radiol Case Rep. 2021. 17: 462-6
5. Labeodan OA, Sur M. Intramedullary schistosomiasis. Pediatr Neurosurg. 2003. 39: 14-6
6. Lighter J, Kim M, Krasinski K. Intramedullary schistosomiasis presenting in an adolescent with prolonged intermittent back pain. Pediatr Neurol. 2008. 39: 44-7
7. Lo NC, Bezerra FS, Colley DG, Fleming FM, Homeida M, Kabatereine N. Review of 2022 WHO guidelines on the control and elimination of schistosomiasis. Lancet Infect Dis. 2022. 22: e327-35
8. Paz JA, Valente M, Casella EB, Marques-Dias MJ. Spinal cord schistosomiasis in children: Analysis of seven cases. Arq Neuropsiquiatr. 2002. 60: 224-30
9. Rodrigues DB, Rodrigues AB, Queiroz JW, Braga MC, Kita WS, Netto RH. Intramedullary spinal schistosomiasis in a child with acute myelopathy: A case report. Surg Neurol Int. 2020. 11: 371
10. Saleem S, Belal AI, El-Ghandour NM. Spinal cord schistosomiasis: MR imaging appearance with surgical and pathologic correlation. AJNR Am J Neuroradiol. 2005. 26: 1646-54
11. Salgado JV, da Silva Cruz Salgado IA, Braga Júnior LL, Serra SC, de Carvalho Barros VM, Silva MJ. Myeloradicular form of neuroschistosomiasis in a six-year-old boy infected with Schistosoma mansoni. Pediatr Infect Dis J. 2015. 34: 1409-11