- Departments of Neurosurgery, University of Washington, Seattle, Washington, United States.
- Otolaryngology, University of Washington, Seattle, Washington, United States.
Correspondence Address:
Zaid Aljuboori, Department of Neurosurgery, University of Washington, Seattle, Washington, United States.
DOI:10.25259/SNI_1166_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zaid Aljuboori1, Margaret McGrath1, Michael Levitt1, Kris Moe2, Randall Chestnut1, Robert Bonow1. A case series of crossbow injury to the head highlighting the importance of an interdisciplinary management approach. 18-Feb-2022;13:60
How to cite this URL: Zaid Aljuboori1, Margaret McGrath1, Michael Levitt1, Kris Moe2, Randall Chestnut1, Robert Bonow1. A case series of crossbow injury to the head highlighting the importance of an interdisciplinary management approach. 18-Feb-2022;13:60. Available from: https://surgicalneurologyint.com/surgicalint-articles/11399/
Abstract
Background: Penetrating crossbow head injuries are rare with no clear consensus regarding the optimal management paradigm for such injuries. We present three cases of crossbow injury to the head, with emphasis on the need for a comprehensive multidisciplinary management plan.
Case Description: Three cases are presented of patients presenting with self-inflicted penetrating crossbow to head injuries. All three patients presented with intact neurological exam. A comprehensive multidisciplinary plan was created for all three cases with subsequent successful removal of the arrows. All three patients were discharged home with modified Rankin scale score of
Conclusion: Penetrating crossbow brain injuries are rare and require complex management. A comprehensive management strategy is necessary to manage these injuries. Moreover, careful consideration of factors such as the arrow trajectory, complexity of the injuries, and availability of the required expertise is important to increase the chances of success.
Keywords: Cerebrospinal fluid, Leak, Crossbow, Trauma, Vascular
INTRODUCTION
Penetrating injuries to the head are relatively rare; specifically, very few cases of crossbow injury to the head have been described.[
CASE DESCRIPTION
Case 1
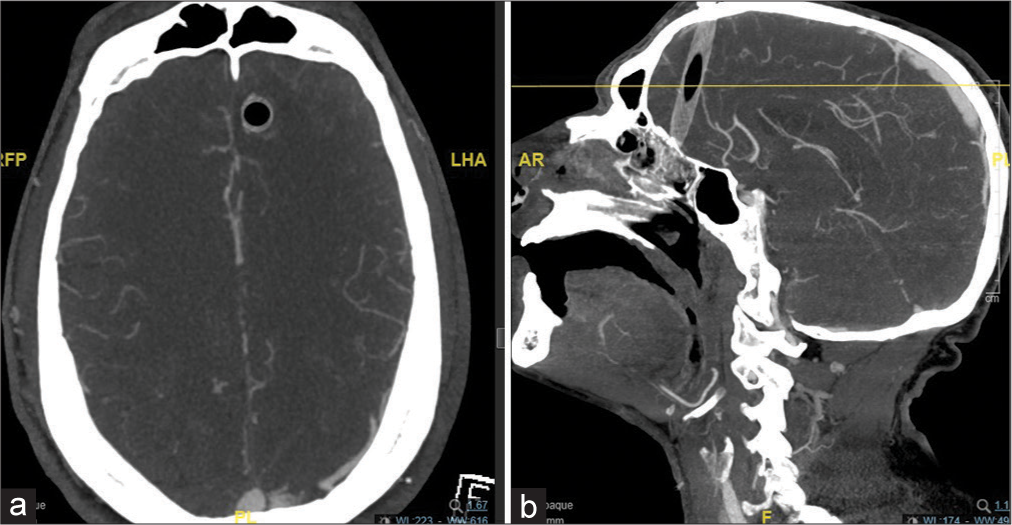
A 36-year-old male with no medical history presented with a penetrating crossbow injury to the head. His Glasgow Coma Scale (GCS) was 15 with intact neurological examination. The arrow (carbon fiber) entered through the left mandible and traversed the cranial vault and partially exited at the level of the vertex about 1 cm off midline. On computed tomography (CT) of the head, the arrow entered through the anterior skull base, passing through the left anterior frontal lobe and exited just lateral to the superior sagittal sinus (SSS) [
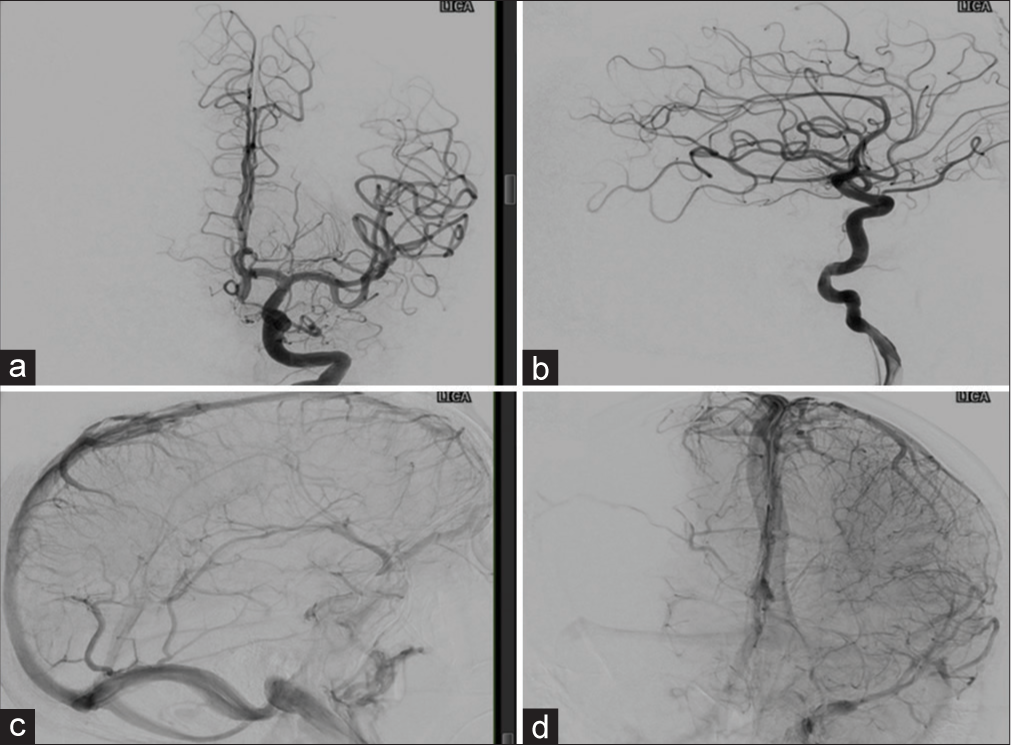
A comprehensive plan was made by the neurovascular, neurotrauma, and otolaryngology teams, which included the use of operating room with angiography capabilities, diagnostic cerebral angiogram before the removal of the arrow, removal of the arrow, and evaluation for and management of cerebrospinal fluid (CSF) leak. The patient underwent endotracheal intubation. Then, a diagnostic cerebral angiogram was done, which showed no evidence of vascular injuries [
Then, an endoscopic examination of the nasal cavity demonstrated the presence of CSF leak, which was repaired using a left middle turbinate flap. The patient tolerated the procedure well and postoperative CT of the head showed no evidence of progression of hemorrhage. The patient was discharged to home on hospital day 6.
Case 2
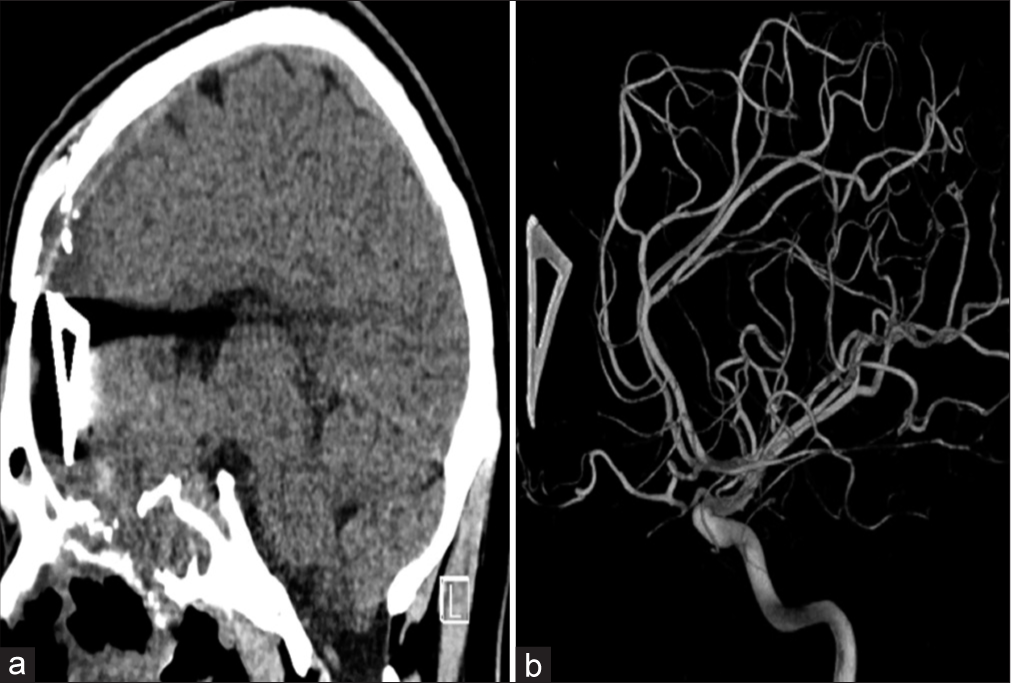
A 22-year-old male with no medical history presented with a penetrating crossbow injury to the head. His GCS was 15 with intact neurological examination. The arrow entered through the floor of the oral cavity and traversed the anterior skull base to exit the cranial vault through the forehead leaving a small metallic fragment intracranially [
Figure 3:
Case 2; (a) a head CT scan image (sagittal view) image that shows the retained arrow fragment on the right side with the associated subarachnoid hemorrhage. (b) a 3D reconstruction image of the diagnostic cerebral angiogram (arterial phase/lateral view) of the right internal carotid artery that shows no arterial injuries.
Similar to Case 1, a comprehensive plan was made by the treating teams. The diagnostic cerebral angiogram showed no evidence of vascular injuries. Moreover, the retained metallic fragment was left in place as its removal most likely to incur more damage. Furthermore, an endoscopic examination of the nasal cavity and the anterior skull base demonstrated the presence of CSF leak, which was repaired using a left middle turbinate flap. The patient tolerated the procedure well and was discharged home.
Case 3
A 67-year-old male with no medical history presented with a penetrating crossbow injury to the head. His GCS was 15 with intact neurological examination. The arrow entered through the floor of the oral cavity and traversed the anterior skull base to exit the cranial vault near the vertex on the right side. Preoperative CT showed a tract intraparenchymal hemorrhage with associated skull base and planum sphenoidale fractures [
This case highlights the importance of the comprehensive multidisciplinary surgical planning. The CTA showed normal cerebral arteries with a filling defect within the SSS. In contrast, the DSA showed occlusion of the distal segment of the right ACA with normal venous sinuses. Of note, the differences in the findings between the two studies could have occurred during the time between the two studies. Nevertheless, preoperative DSA can have a better yield, especially with the presence of artifact effect from the foreign body. Moreover, case 3 highlights the importance of concurrent endoscopic evaluation of the anterior skull base for CSF leak. In case 3, the patient was noted to have CSF leak which failed initial conservative management and required a second surgical intervention to repair the defect.
DISCUSSION
Penetrating head injuries are rare and require complex management approach. Intracranial crossbow injuries are extremely rare and present a challenge due to the complexity of the injury patterns. Modern crossbows typically generate a speed between 280 and 350 feet per second, which translates to 50–100 (foot pounds) of kinetic energy.[
The complexity of crossbow injuries depends on several factors such as the distance, entry and exit points, trajectory, arrow material, and others. Therefore, a comprehensive multidisciplinary plan is necessary to optimally manage the afflicted patients. Moreover, it’s crucial to identify the sequence of the procedural steps and prepare a contingency plan for each one.
The main goals of the management of crossbow injuries are stabilizing the patient’s clinical status, removal of the foreign body (arrow) in a safe manner, and management of potential complications. When managing patient with these injuries, we suggest using of the following paradigm: (1) consider airway management and secure a safe airway with the appropriate teams at bedside. (2) Manage the traumatic brain injury (TBI) and associated monitoring needs. (3) Evaluate for vascular injury and treat as necessary. (4) Surgical management of foreign body (arrow) removal. (5) Evaluation for and management of CSF leak. (6) Prevention of infection.
Airway management
It is crucial to assess and secure a safe airway in all settings, especially in the clinical setting of penetrating injury through the oral cavity. In the first two cases, the patient underwent endotracheal intubation by the anesthesia team in the presence of the otolaryngology team for backup. Moreover, we were prepared for an emergent surgical airway. In the third case, the anesthesia team assessed the airway and decided to proceed with intubation without otolaryngology at bedside.
Management of brain injury
For patients with low GCS ≤8, intracranial pressure monitoring is necessary. Furthermore, in the presence of intracranial hematoma (e.g., epidural, subdural, or intraparenchymal), the TBI guidelines should be followed to manage the patient.[
Evaluation of the head-and-neck vascular structures
Penetrating injuries can usually affect branches of the external carotid and/or internal carotid arteries (ECAs/ICAs) as well as the venous sinuses. Therefore, a diagnostic cerebral angiogram should be considered even in the setting of normal CTA/CTV. CTA has limited sensitivity in the setting of penetrating TBI.[
Manner of the arrow removal
Safe removal of a foreign body requires consideration of the trajectory and anatomical structures at risk. In case 1, the arrow entered the cranium at the anterior skull base and the bullet point exited near the vertex, while the fletchings remained outside the oral cavity. Therefore, we decided to cut the arrow shaft in the oral cavity so the inferior portion can be pulled out. Before removal of the superior portion, we set up for a craniotomy and prepared for the possibility of SSS repair. Then, we removed superior part of the arrow with no issues. The wound was copiously irrigated with saline to help reduce risk of infection. Moreover, we performed an intraoperative CT scan of the head to rule out any new intraparenchymal hemorrhage that was instigated by the removal of the arrow. For case 2, the retained fragment was lodged within the right frontal lobe and its removal would have caused more damage to the surrounding neural structures. Therefore, we decided to leave it in place. In case 3, the arrow entered through the oral cavity and exited at the vertex, similar to case 1. Removal of the arrow required a mini-craniotomy around the exit site to dislodge the arrow. The team was prepared for repair of sinus injury but there was no significant bleeding encountered and the patient was closed without issues. Similar to case 1, irrigation was performed for infection risk reduction.
Evaluation for and management of CSF leak
Since the arrow passed through the anterior skull base, there was high likelihood for CSF leak. As such, we performed an endoscopic evaluation for CSF leak, which was evident in all cases. We repaired the anterior skull base defect using a middle turbinate graft in cases 1 and 2 and a nasoseptal flap in case 3 to seal the CSF leak and prevent the complications associated with it (e.g., meningitis).[
Prevention of infection
In penetrating brain injuries, it’s crucial to monitor for the development of infection using patient’s vitals and inflammatory markers (e.g., erythrocyte sedimentation rate, C-reactive protein, and white blood cells count). Patients with penetrating head injuries can develop both superficial (e.g., skin) and deep (e.g., brain abscess). The administration of broad-spectrum antibiotic prophylaxis is controversial with several studies showed no benefits.[
A comprehensive multidisciplinary management plan is necessary to care for patients with penetrating crossbow injuries to the brain. The plan should consider factors such as the patient’s clinical condition, characteristics and complexity of the injury, and the availability of the necessary expertise to manage the potential complications.
CONCLUSION
Penetrating crossbow brain injuries are rare and require complex management. To manage patients with such injuries, a comprehensive management strategy should be created. Moreover, careful consideration of factors such as the arrow trajectory, complexity of the injuries, and availability of the required expertise is important to increase the chances of success.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ares WJ, Jankowitz BT, Tonetti DA, Gross BA, Grandhi R. A comparison of digital subtraction angiography and computed tomography angiography for the diagnosis of penetrating cerebrovascular injury. Neurosurg Focus. 2019. 47: E16
2. Bodanapally UK, Shanmuganathan K, Boscak AR, Jaffray PM, van der Byl G, Roy AK. Vascular complications of penetrating brain injury: Comparison of helical CT angiography and conventional angiography. J Neurosurg. 2014. 121: 1275-83
3. Frank M, Schikorr W, Tesch R, Werner R, Hanisch S, Peters D. Ballistic parameters and trauma potential of pistol crossbows. Int J Legal Med. 2013. 127: 777-82
4. Franklin GA, Lukan JK. Self-inflicted crossbow injury to the head. J Trauma. 2002. 52: 1009
5. Harmon LA, Haase DJ, Kufera JA, Adnan S, Cabral D, Lottenberg L. Infection after penetrating brain injury-an eastern association for the surgery of trauma multicenter study oral presentation at the 32nd annual meeting of the eastern association for the surgery of trauma, January 15-19, 2019, in Austin, Texas. J Trauma Acute Care Surg. 2019. 87: 61-7
6. Hawryluk GW, Rubiano AM, Totten AM, O’Reilly C, Ullman JS, Bratton SL. Guidelines for the management of severe traumatic brain injury: 2020 Update of the decompressive craniectomy recommendations. Neurosurgery. 2020. 87: 427-34
7. Psaltis AJ, Schlosser RJ, Banks CA, Yawn J, Soler ZM. A systematic review of the endoscopic repair of cerebrospinal fluid leaks. Otolaryngol Head Neck Surg. 2012. 147: 196-203
8. Rehulka H, Cechova E, Mottlova J, Valenta M, Mareska Z. Fatal head injury caused by a crossbow arrow with unusually preserved posttraumatic volitional activity-case report. Soud Lek. 2016. 61: 2-4
9. Saafan ME, Albirmawy OA, Tomoum MO. Sandwich grafting technique for endoscopic endonasal repair of cerebrospinal fluid rhinorrhoea. Eur Arch Otorhinolaryngol. 2014. 271: 1073-9
10. Schoentgen C, Henaux PL, Godey B, Jegoux F. Management of post-traumatic cerebrospinal fluid (CSF) leak of anterior skull base: 10 years experience. Acta Otolaryngol. 2013. 133: 944-50