- Department of Neurosurgery, Oklahoma University Health Science Center, Oklahoma City, United States.
- Department of Otolaryngology, Oklahoma University Health Science Center, Oklahoma City, United States.
Correspondence Address:
Lance Michael Villeneuve, Department of Neurosurgery, Oklahoma University Health Science Center, Oklahoma City, United States.
DOI:10.25259/SNI_658_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lance Michael Villeneuve1, Zoya Voronovich1, Alexander Evans1, Edward T. El Rassi2, Ian F. Dunn1, Zachary A. Smith1. A combined approach for stabilization and endoscopic/ endonasal odontoid and clivus resection for treatment of basilar invagination. 11-Oct-2021;12:511
How to cite this URL: Lance Michael Villeneuve1, Zoya Voronovich1, Alexander Evans1, Edward T. El Rassi2, Ian F. Dunn1, Zachary A. Smith1. A combined approach for stabilization and endoscopic/ endonasal odontoid and clivus resection for treatment of basilar invagination. 11-Oct-2021;12:511. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11172
Abstract
Background: Basilar invagination (BI) is a complex condition characterized by prolapse of the odontoid into the brain stem/upper cervical cord. This lesion is often associated with Chiari malformations, and rheumatoid arthritis (RA). Treatment options for BI typically include cervical traction, an isolated anterior transoral odontoidectomy, anterior endonasal odontoidectomy, an isolated posterior fusion, or combined anterior/ posterior surgical approach.
Case Description: A 45-year-old female with a Chiari I malformation and RA underwent a combined posterior C0-C5 posterior decompression/fusion, followed by an anterior odontoidectomy (i.e. endoscopic/endonasal under neuronavigation). Postoperatively, the patient’s symptoms and neurological signs resolved.
Conclusion: BI in was successfully managed with a combined posterior C0-C5 decompression/fusion followed by an anterior endoscopic/endonasal odontoidectomy performed under neuronavigation.
Keywords: Basilar invagination, Endoscopic endonasal approach, Intraoperative 3D fluoroscopy, Odontoidectomy
INTRODUCTION
Basilar invagination (BI) resulting in cord compression is often associated with rheumatoid arthritis (RA), Chiari malformations (CM), Down syndrome, Klippel-Feil syndrome, or osteogenesis imperfecta.[
CASE PRESENTATION
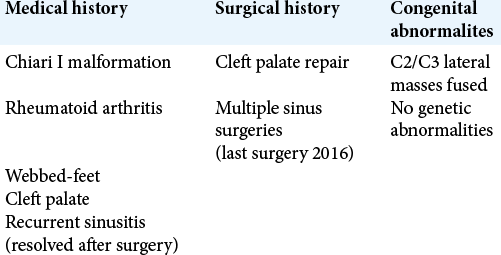
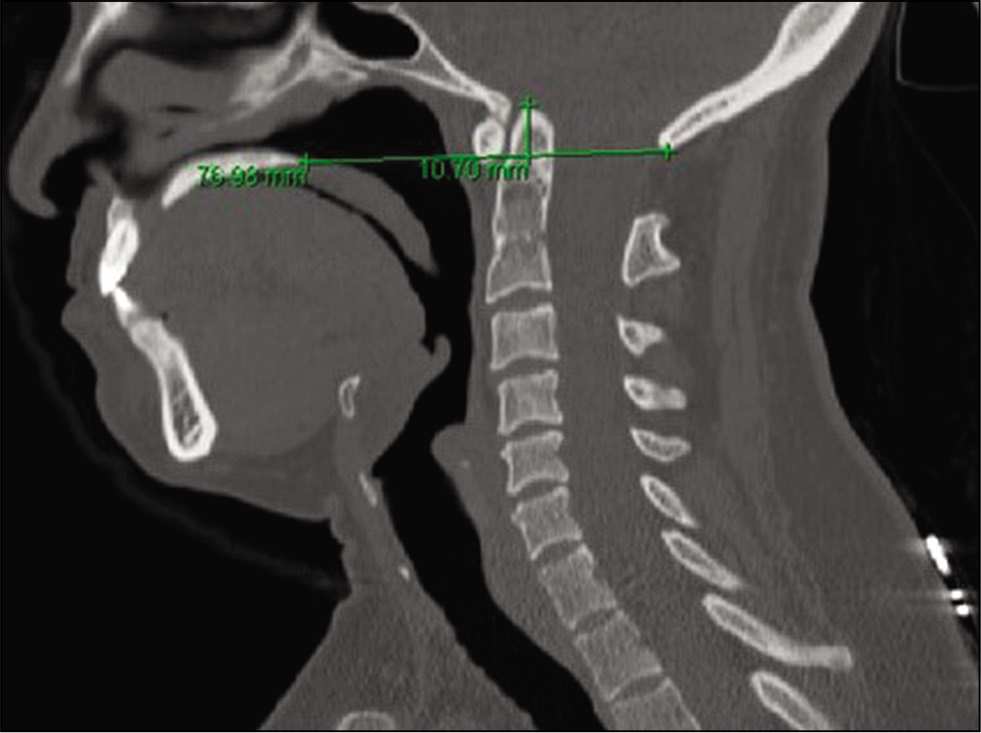
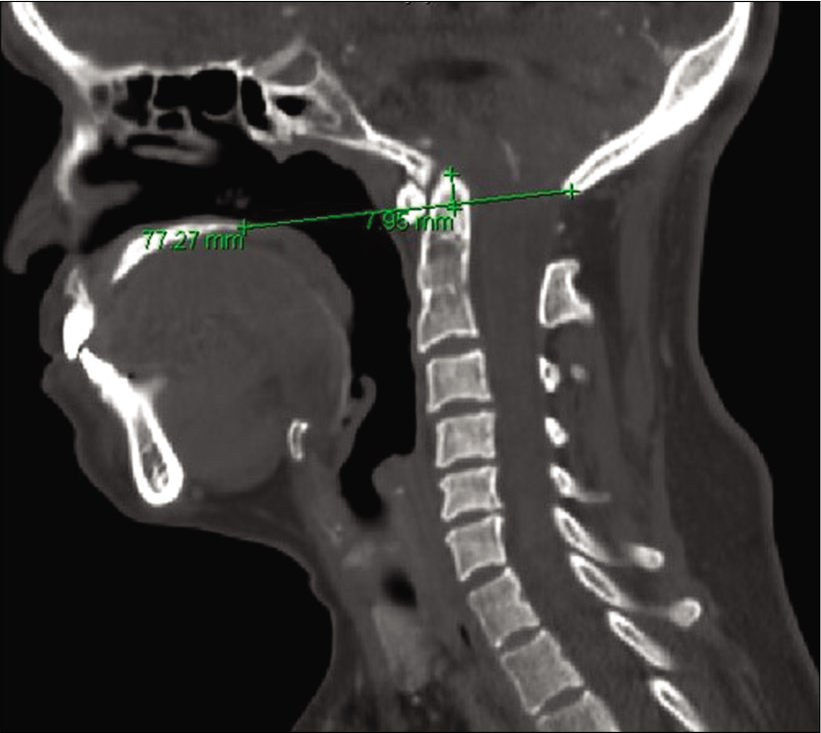
A 45-year-old female presented with a Chiari I malformation (CM) and RA presented with 7-months of progressive suboccipital headaches [
Surgery
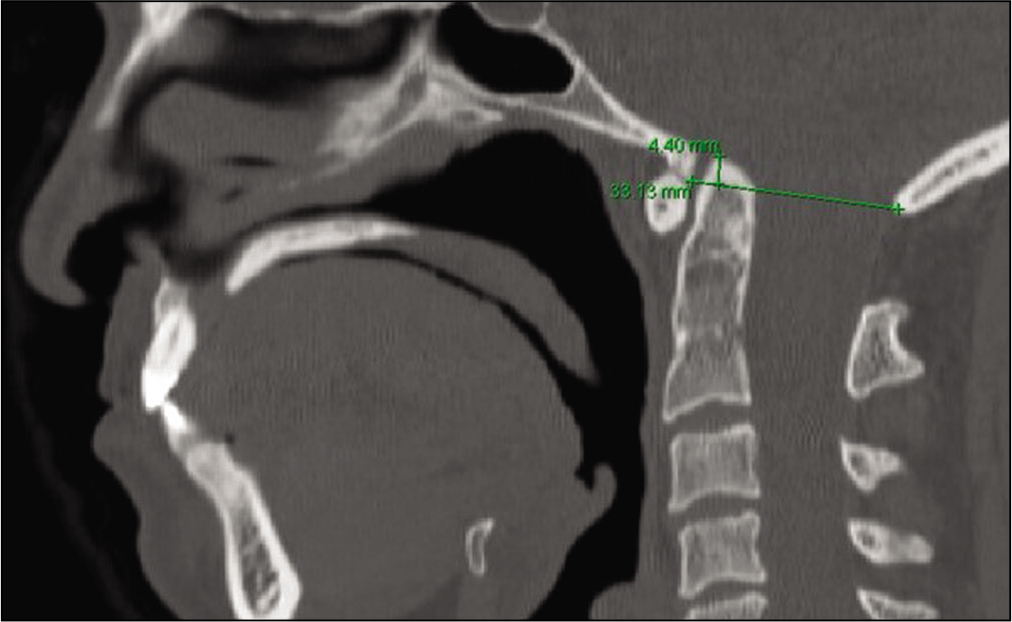
As 48 h of halo ring traction (i.e. secured to a halo vest) resulted in minimal odontoid reduction (i.e. movement of ~2-mm), the patient required posterior followed by anterior cervical surgery [
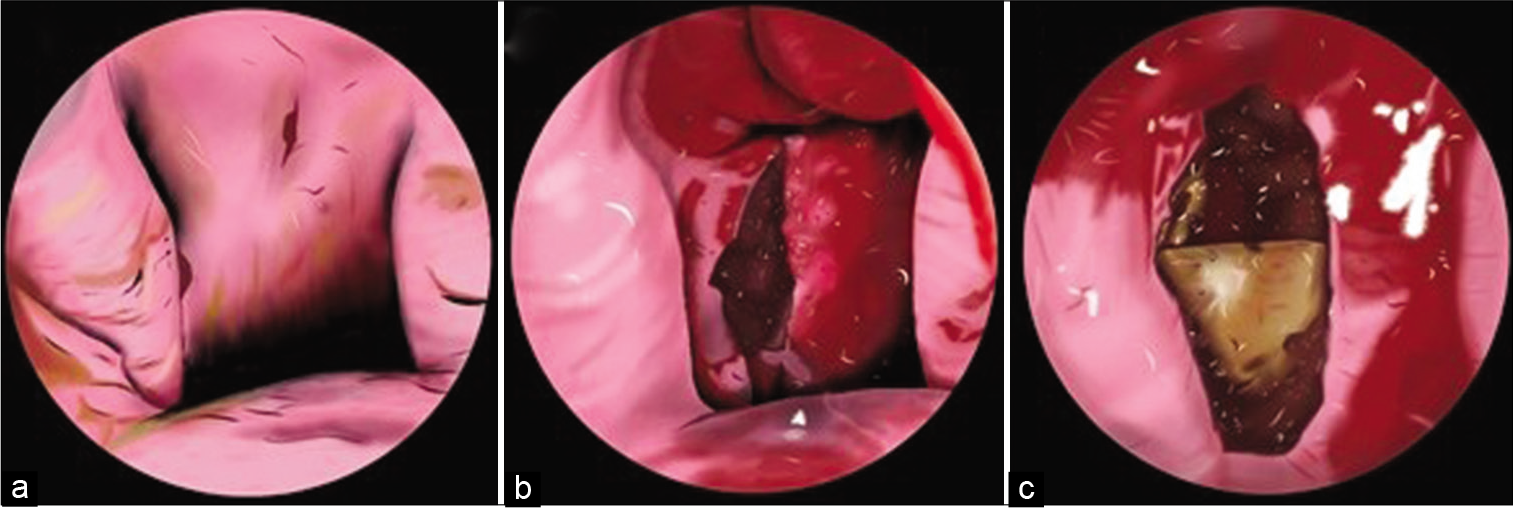
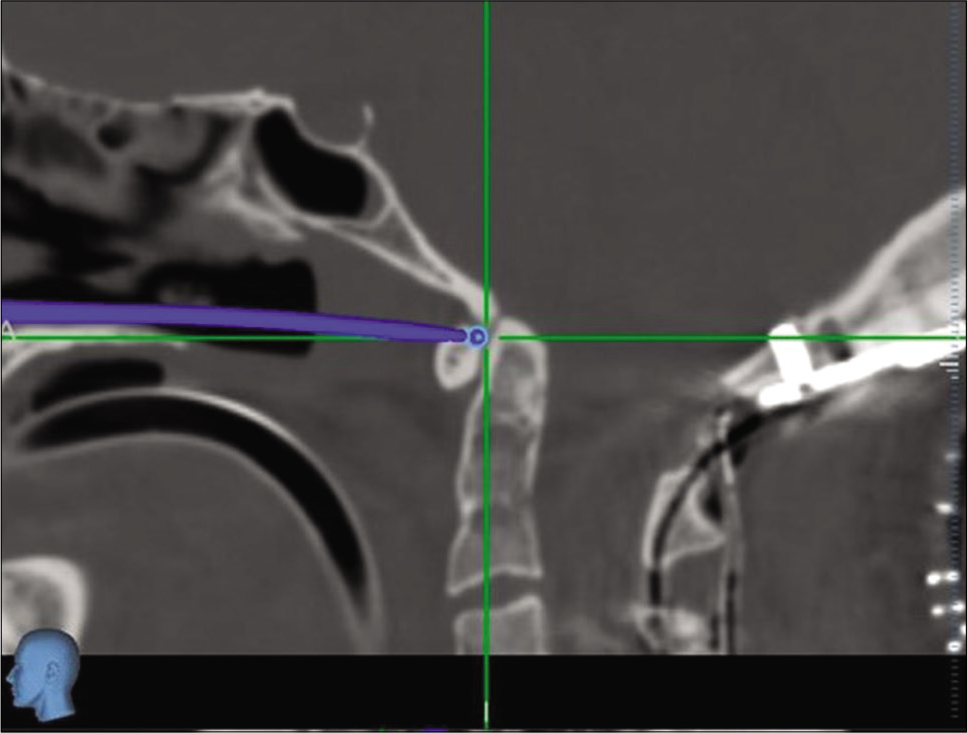
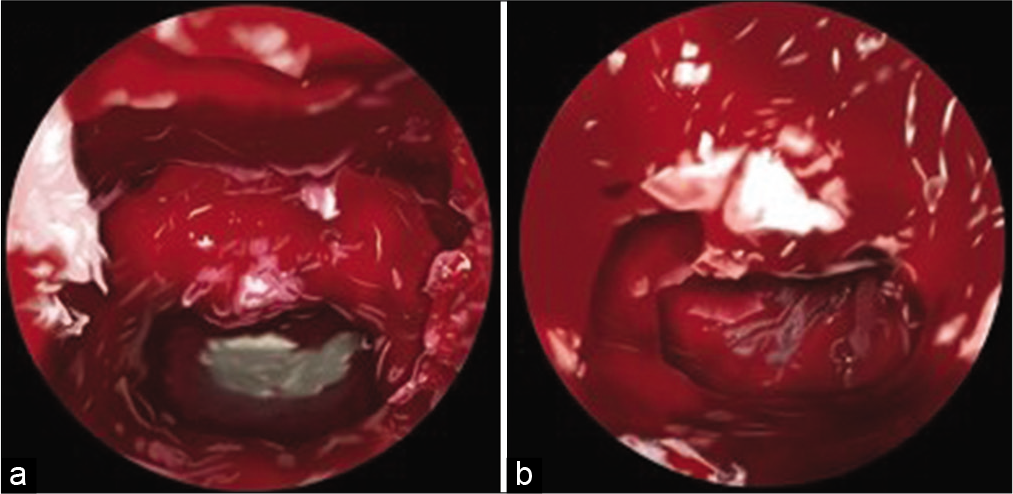
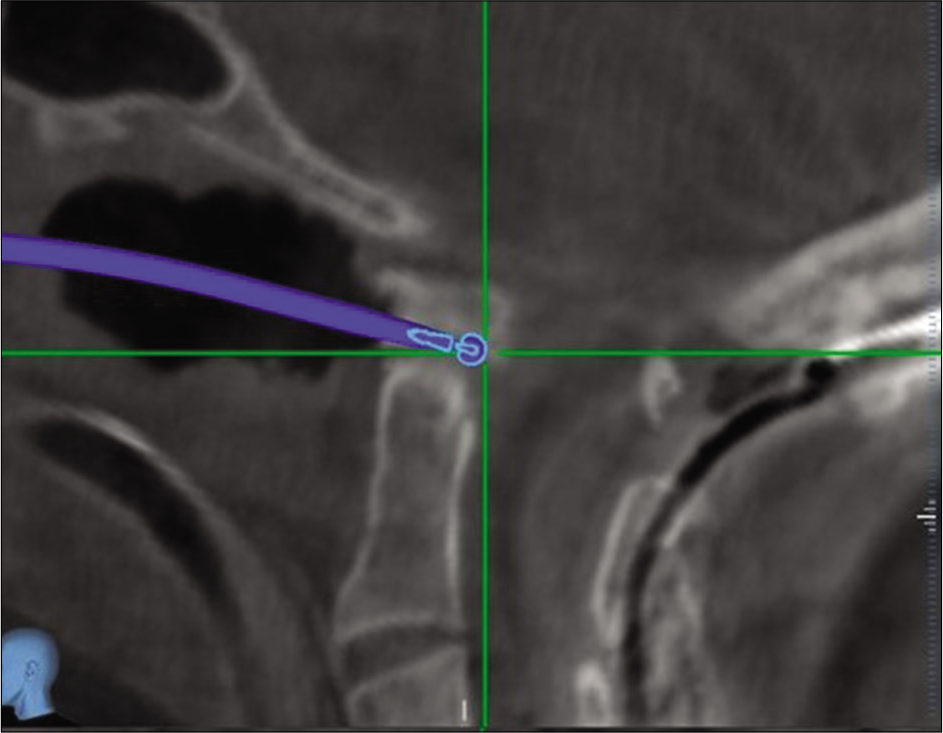
The C0-C5 decompression and fusion revealed underdeveloped lateral masses (i.e., analogous to pediatric lateral masses) and confirmed a congenital C2/3 lateral mass fusion. Despite this finding, 14-mm screws were effectively placed for lateral mass fixation. The second procedure, an endoscopic/endonasal odontoidectomy utilized neuronavigation. A small incision was made in the soft palate, and the posterior portion of the hard palate was removed using the zero-degree endoscope allowing access to remove the inferior odontoid [
DISCUSSION
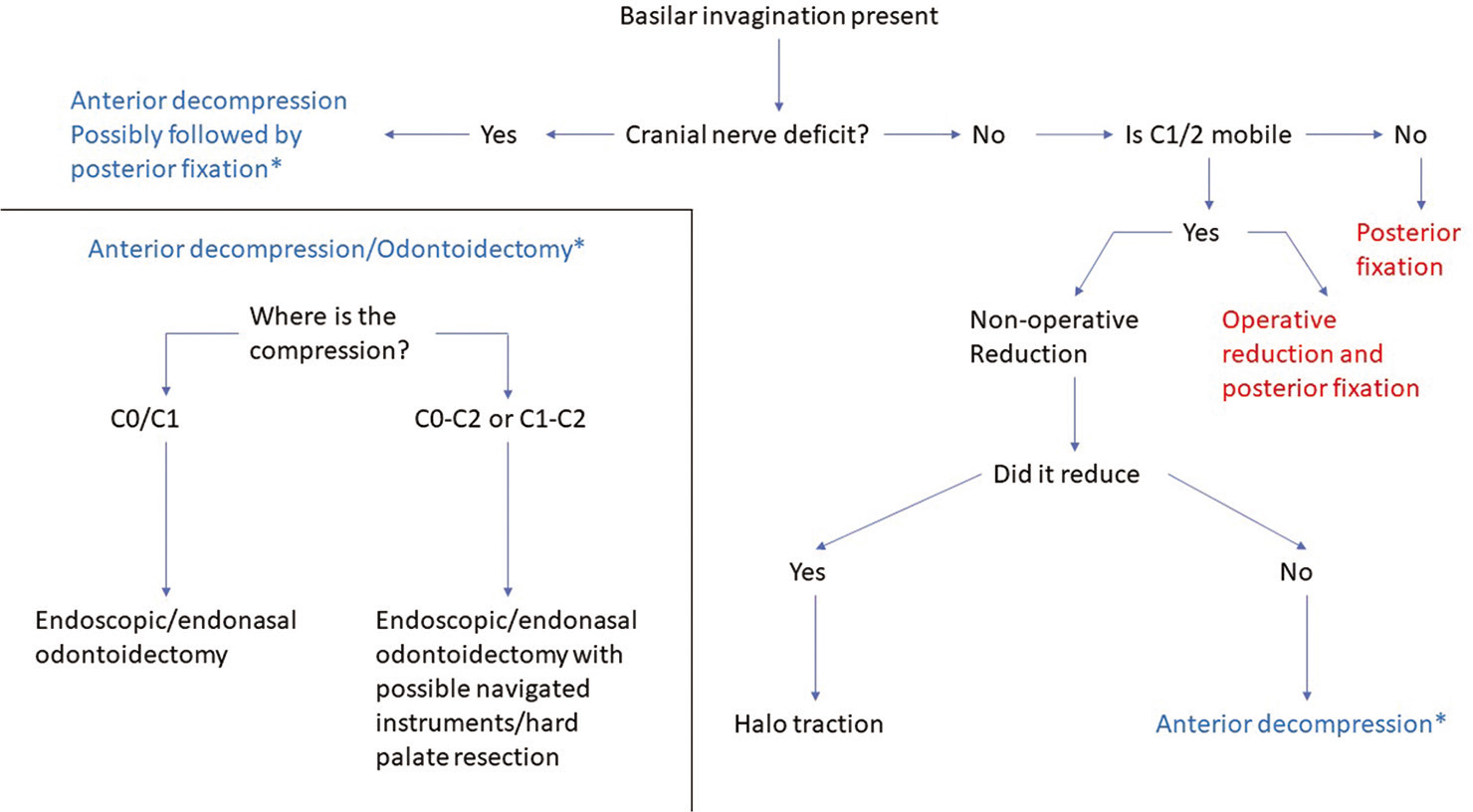
There are a variety of surgical options for treating craniocervical junctional abnormalities. Indications for surgery include cranial nerve deficits, brainstem/spinal cord compression, craniocervical instability/ligamentous laxity, and autofusion anomalies. Symptomatic BI may be treated with cervical traction, an anterior odontoidectomy, a posterior C0-C2 fusion, or a combination of these approaches [
CONCLUSION
Here, we presented a 45-year-old female with BI, a CM, and RA who was successfully treated with a posterior decompression/fusion from C0-C5 followed by an anterior endoscopic/endonasal odontoidectomy.
Disclosures
The authors report no disclosures or conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclosures
The authors report no disclosures or conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chaudhry NS, Ozpinar A, Bi WL, Chavakula V, Chi JH, Dunn IF. Basilar invagination: Case report and literature review. World Neurosurg. 2015. 83: 1180.e7-11
2. Gande A, Tormenti MJ, Koutourousiou M, Paluzzi A, Fernendez-Miranda JC, Snydermnan CH. Intraoperative computed tomography guidance to confirm decompression following endoscopic endonasal approach for cervicomedullary compression. J Neurol Surg B Skull Base. 2013. 74: 44-9
3. Joaquim AF, Osorio JA, Riew KD. Transoral and endoscopic endonasal odontoidectomies-surgical techniques, indications, and complications. Neurospine. 2019. 16: 462-9
4. Joseph V, Rajshekhar V. Resolution of syringomyelia and basilar invagination after traction. Case illustration. J Neurosurg. 2003. 98: 298
5. Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R. Expanded endonasal approach: Fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus. 2005. 19: E6
6. Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980. 53: 444-55
7. Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and transnasal odontoidectomy complications: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2016. 148: 121-9