- Department of Neurosurgery, Wenxi People's Hospital, 99 Tai-Feng Xi-Lu, Wenxi, Shanxi, 043800, China
- Shangxi Mental Health Center, 55 Nan-Shi-Fang Street, Taiyuan, Shanxi, 030001, China
Correspondence Address:
Jun-Jie Wei
Shangxi Mental Health Center, 55 Nan-Shi-Fang Street, Taiyuan, Shanxi, 030001, China
DOI:10.4103/2152-7806.166847
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wei J, Liu H, Chai S, Kang X. A fast cranial drilling technique in treating severe intracranial hemorrhage. Surg Neurol Int 07-Oct-2015;6:159
How to cite this URL: Wei J, Liu H, Chai S, Kang X. A fast cranial drilling technique in treating severe intracranial hemorrhage. Surg Neurol Int 07-Oct-2015;6:159. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-fast-cranial-drilling-technique-in-treating-severe-intracranial/
Abstract
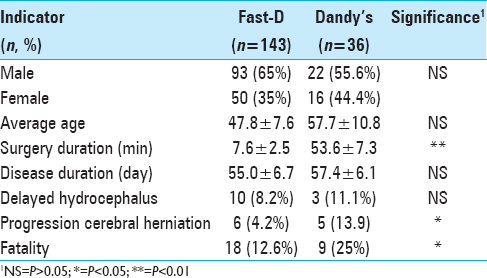
Background:This study is a retrospective case analysis of 143 patients who suffered from severe intracranial hemorrhage and underwent a fast and simple procedure of cranial drilling followed with external ventricle drain treatment (referred as Fast-D here after) during 2003-2013 to evaluate the clinical effectiveness of the treatment.
Methods:Fast-D procedure was conducted on 143 patients with severe acute craniocerebral diseases. Those patients were evaluated using activities of daily living (ADL) scales at hospital discharge and after 6-month of physical therapy, and were compared to 36 patients with similar craniocerebral diseases but received the traditional Dandy's surgical treatment.
Results:At discharge, 11% (16 cases) was classified as ADL I (fully functional for physical and social activities); 26% (37 cases) had ADL II (fully functional for physical activities but partially impaired for social activities); 34% (49 cases) was ADL III (require assistance performing physical activities); 9% (13 cases) was ADL IV (being conscious, but completely lost ability of physical activities); 27% (10 cases) was ADL V (vegetative stage); and 13% (18 cased) was ADL VI (died) among the 143 patients. Six-month physical therapy improved ADL in 88% of the patients. Those outcomes are equal or better than the more complicated Dandy's procedure probably due to the time-saving factor.
Conclusion:Fast-D procedure is much faster (6.7 min vs. 53.6 min of the Dandy's procedure) and can be performed outside operating rooms (computed tomography room or bedside). This technique could serve as a tool to rapidly release intracranial pressure and reduce subsequent morbidity and mortality of severe craniocerebral diseases when resource and condition are limited and more elaborate operating room procedures are not possible.
Keywords: Cranial drill, drainage, intracranial hemorrhages, intracranial pressure
INTRODUCTION
Intracranial hypertension is a common occurrence for patients suffering from craniocerebral diseases. An elevated intracranial pressure (ICP) is very likely to cause severe nonreversible damage to brain tissues and often times is fatal if prolonged. Prompt medical attention and rapid relief of high ICP can prevent impending mortality and may significantly improve functional outcomes of patients with craniocerebral diseases.[
MATERIALS AND METHODS
Patient selection
Between January 2003 and January 2013, a total of 467 patients with severe craniocerebral hemorrhage were admitted to our hospital. Among them 143 patients received the Fast-D treatment. Those 143 patients were selected based on the following combined criteria: (1) Glasgow Coma Scale (GCS, 15-point scale) was between 3 and 8; (2) lack of craniotomy requirement or the operation was refused by family members; and (3) patient's condition was suitable for lateral ventricle external drainage. During the same time period, 36 patients received the traditional Dandy's drilling procedure.
Examinations
Computed tomography (CT) or magnetic resonance imaging (MRI) scans were performed on all the patients. For intracerebral hemorrhage patients, the scans were to determine the location and size (volume) of the bleeding, and the intensity of ventricle penetration. For other patients, the intensity of lateral ventricle compression was evaluated. Those scan images were used to determine whether a patient was suitable for performing the Fast-D procedure. The blood pressure of all patients was within the range of 160–240/100–160 mm Hg.
Operational procedure and clinical treatments
For Fast-D, while routine treatment measures were performed, patients were placed in supine position. The drill site was generally located at just inside of frontal hairline and 2 cm away from the center line. The exact puncture location was fine-tuned based on CT or MRI images if necessary. After hair removal followed by povidone-iodine cleansing and local anesthesia with 1% lidocaine hydrochloride, drilling was performed to penetrate the scalp, skull, and dura mater in one thrust using a manually powered drilling device [
Regular Dandy's procedure was performed in operating rooms with general anesthesia on 36 patients. All other cares were kept the same as the Fast-D patients.
Postoperation treatments
The shunt tube was kept blockage-free at all times. The color and the volume of the drainage fluid were recorded, and the constitution was routinely tested and monitored. The duration of the shunt was generally <1-week. If it exceeded 1-week, bacterial culture tests were performed regularly to ensure no intracranial infection. For cases of severe intraventricular hemorrhage, 3 ml 0.9% streptokinase and 30,000 IU urokinase were injected through the tubing followed by 1–2 h of closure. Such practice could be repeated 2–3 times a day to dissolve coagulated blood for easier drainage. The removal of the tubing (end of external drainage) was determined based on the color, volume of the drainage fluid, and the images of CT and MRI scans. After removal, the tubing was cultured for pathogenic bacteria. Antibiotic sensitivity tests were followed if the test was positive. The patients were closely monitored for signs of infection and treated with antibiotics if necessary.
After hospital discharge, all patients with activities of daily living (ADL) of II–V received 6 months of physical therapy treatment.
Evaluation criteria
Patient recovery was evaluated at hospital discharge and a follow-up at 6 months after discharge. ADL scales were used to classify the patients as the following: ADL I-fully functional in performing physical and social daily activities; ADL II-fully functional in performing physical daily activities and slightly impaired in social activities; ADL III-partially functional and requires assistance in performing physical daily activities; ADL IV-being conscious, but completely lost ability of performing physical daily activities; ADL V-vegetative stage; and ADL VI-died.
Data analysis
All data were analyzed using t-test or binomial test in MS-Excel. Statistical significance was set at P < 0.05 for all comparisons.
RESULTS
The 143 Fast-D patients were 93 males (65%) and 50 females (35%) aged between 12 and 86 years old with the mean age of 47.8 [
The entire Fast-D procedure (include drilling and inserting the drainage tube) was completed within 10 min for all the patients with a mean of 6.7 ± 2.5 min. Out of the 143 cases, 136 cases (95.1%) were successful with one attempt. The remaining 7 cases (4.9%) required second attempts. Delayed hydrocephalus occurred in 10 patients (8.2%) requiring a bypass surgery. Six patients (4.2%) suffered progressive cerebral herniation. The Dandy's procedure took an average of 53.6 ± 7.3 min, significantly longer than that of Fast-D. All 36 cases were successful with one attempt. Three patients (11.1%) suffered delayed hydrocephalus, not significantly differ from the Fast-D group. Five patients (13.9%) suffered progressive cerebral herniation, significantly higher than that of the Fast-D patient group (4.2%) [
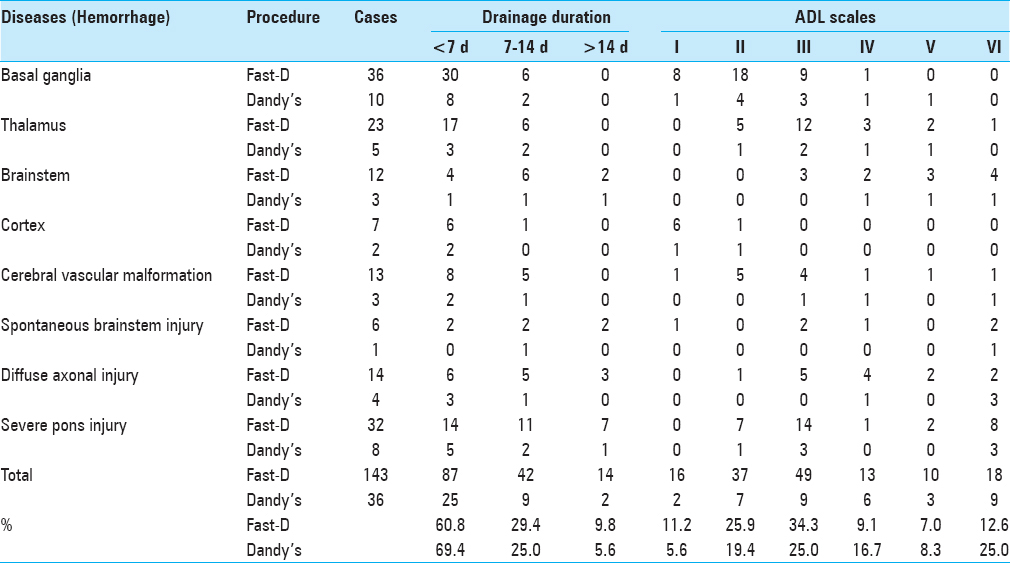
Eighty-seven Fast-D patients (60.8%) required <7 days of the external drainage. Forty-two cases (29.4%) required between 7 and 14 days, and 14 cases (9.8%) required longer than 14 days [
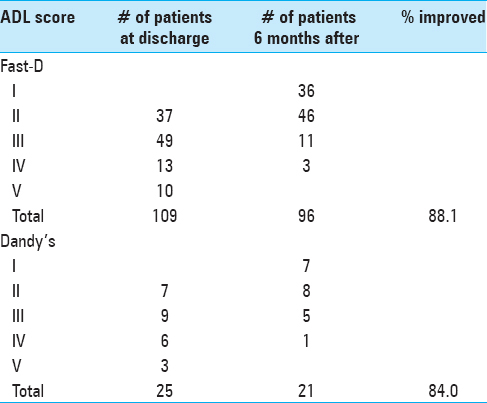
Among the 143 patients, 102 (71.0%) achieved an ADL performance of level III or better, including 16 (11.2%) of ADL I, 37 (25.9%) of ADL II and 49 (34.3%) of ADL III. There were 13 cases of ADL IV, 10 cases of ADL V, and 18 cases (12.6%) of death [
Physical therapy of 6 months improved the ADL scores of 96 patients (88.1%). The ADL scores of 36 out of 37 patients improved from II to I; 46 out of 49 patients improved from III to II; 11 out of 13 patients improved from IV to III; and 3 out of 10 patients improved from V to IV after 6 months of physical therapy [
DISCUSSION
Severe intracranial hemorrhage is an acute condition that constitutes immediate medical emergency as the condition can progress rapidly resulting in diffuse brain edema as fast as in 20–30 min.[
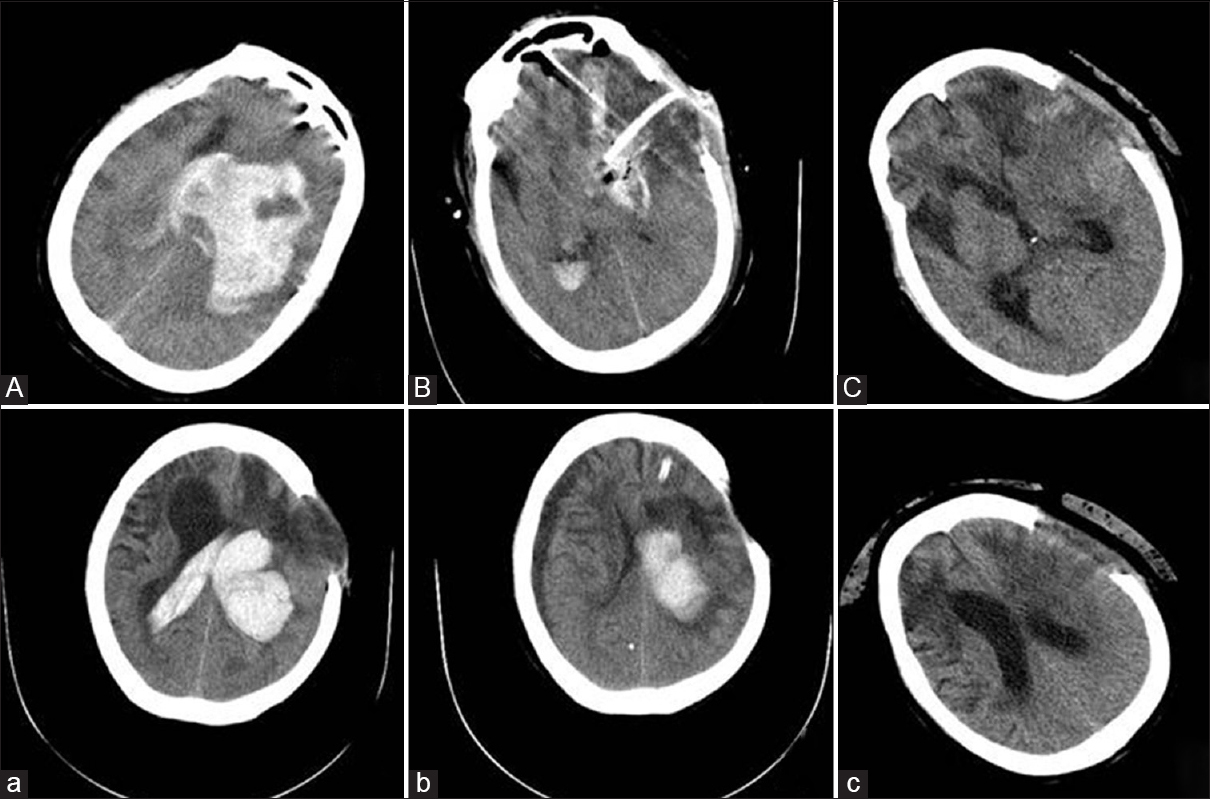
Figure 2
Computed tomography images of a patient who underwent both the craniotomy and the Fast-D treatment. (A) Left basal ganglia hemorrhage (165 ml) before craniotomy; (B) Two days after craniotomy; (C) One month after craniotomy; (a) Left basal ganglia hemorrhage (103 ml) (2 years later); (b) Two days after Fast-D drainage treatment; (c) One month after Fast-D treatment
More than 60% of the 143 patients had <7 days of hospitalization period, and the mortality rate was 13% that is, lower than previous reports of patients with GCS of 3–8 (21.2–25.7%) that received other types of treatments such as conservative drug therapy.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cheng HD. Treatment of 67 cases of severe spontaneous intracerebral hemorrhage. Chin J Clin Neurosurg. 2005. 10: 227-
2. Gao XG. Primary intracerebral hemorrhage. Chin Gen Pract. 2005. 8: 1647-8
3. Jia JM, Jiang XF, Xie P. Clinical analysis of 156 cases of severe traumatic brain injury. Clin Med. 2011. 31: 45-7
4. Nieuwkamp DJ, de Gans K, Rinkel GJ, Algra A. Treatment and outcome of severe intraventricular extension in patients with subarachnoid or intracerebral hemorrhage: A systematic review of the literature. J Neurol. 2000. 247: 117-21
5. Roozenbeek B, Chiu YL, Lingsma HF, Gerber LM, Steyerberg EW, Ghajar J. Predicting 14-day mortality after severe traumatic brain injury: Application of the IMPACT models in the brain trauma foundation TBI-trac® New York State database. J Neurotrauma. 2012. 29: 1306-12
6. . Shandong Medical School Hospital Neurosurgical Department. Clinical application and animal study of a cranial fine-drilling device. Chin Med J. 1975. 55: 641-3
7. Sim SK, Lim SL, Lee HK, Liew D, Wong A. Care of severe head injury patients in the Sarawak General Hospital: Intensive care unit versus general ward. Med J Malaysia. 2011. 66: 138-41
8. Todo T, Usui M, Takakura K. Treatment of severe intraventricular hemorrhage by intraventricular infusion of urokinase. J Neurosurg. 1991. 74: 81-6
9. Wei L, Li G, Jin P, Wang CW, Fei C, Wang DK. Rapid pore cranial drilling and ventricular drainage treatment in ventricular hemorrhage: A clinical analysis of 3571 cases. Chin J Neuromed. 2011. 10: 731-4
10. Yang SZ, Li LN, Li SD, Peng YB, Yang XK, Wei YJ. Research of clinical epidemiology of 6690 cases of craniocerebral injury. Chin J Neuromed. 2006. 5: 274-7
11. Yao ML, Lin SH.editors. Cerebrovascular Diseases. Beijing, China: People Health Publishing House; 2002. p.
12. Yoshino E, Yamaki T, Higuchi T, Horikawa Y, Hirakawa K. Acute brain edema in fatal head injury: Analysis by dynamic CT scanning. J Neurosurg. 1985. 63: 830-9