- David Geffen School of Medicine at UCLA, Los Angeles, California, USA
- Department of Neurosurgery, Shanghai Children's Medical Center, Shanghai, China
- UCLA Center for World Health at the David Geffen School of Medicine, Los Angeles, California, USA
Correspondence Address:
Jorge Lazareff
David Geffen School of Medicine at UCLA, Los Angeles, California, USA
UCLA Center for World Health at the David Geffen School of Medicine, Los Angeles, California, USA
DOI:10.4103/sni.sni_384_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrew Campion, Clement Lee, Nan Bao, Jorge Lazareff. A parental perspective concerning barriers to care for neural tube defects in China. 22-Aug-2017;8:195
How to cite this URL: Andrew Campion, Clement Lee, Nan Bao, Jorge Lazareff. A parental perspective concerning barriers to care for neural tube defects in China. 22-Aug-2017;8:195. Available from: http://surgicalneurologyint.com/surgicalint-articles/a-parental-perspective-concerning-barriers-to-care-for-neural-tube-defects-in-china/
Abstract
Background:The People's Republic of China (PRC) has the highest incidence of neural tube defects (NTDs) in the world. NTDs remain a significant contributor to the global burden of disease amendable to surgical care; however, no studies to date have evaluated the patients’ perspective regarding perceived barriers to care.
Methods:The study was conducted at the Shanghai Children's Medical Center (SCMC) between 6/11/2014 and 7/17/2014. Surveys were administered to families presenting to the clinic of the SCMC director for Pediatric Neurosurgery. Additionally, orphaned patients under the care of the Baobei Foundation were surveyed for comparison. Participants were allowed to mark as many barriers on the survey as they deemed relevant to their experience.
Results:A total of 69 patients were surveyed. The most frequently chosen barrier to care, with a P value -5, was that the referring physician did not know enough about the child's condition. As compared to the Baobei Foundation orphans, surveyed patients presented at an older age for initial treatment (7 months versus 1 month, P value = 0.001), and visited more hospitals before reaching SCMC (3.14 versus 1.0, P value -5).
Conclusions:The results of this study highlight the referring physician as a primary barrier to care. The younger age at time of treatment for Baobei orphans born with NTDs supports this finding, as they essentially bypassed the referral process. An elaboration on reasons for this real or perceived barrier may provide insight into a means for expedited diagnosis and treatment of NTDs within the PRC.
Keywords: Barriers to care, neural tube defect, People's Republic of China, referral system, surgery, survey
INTRODUCTION
The People's Republic of China (PRC) has the highest incidence of neural tube defects (NTDs) in the world.[
The more severe manifestations of NTDs demand medical attention within the first 24–72 hours of life for ideal long-term neurologic function.[
Access to surgical care for NTDs remains a broad subject that has not been extensively addressed in the literature. To date, the evaluation of barriers to timely surgical treatment has come primarily from retrospective institution-based analysis of gaps in care.[
We had the opportunity to explore this issue at the Shanghai Children's Medical Center (SCMC), a tertiary care hospital in the PRC with one of the country's premiere neurosurgical units. Those surveyed presented to SCMC through one of two primary routes: either as patients with their family member(s) or as orphans through the assistance of the Baobei Foundation, a horizontal program orchestrating the medical care of children in the PRC orphanage system. SCMC coordinates care for children from a wide geographic range centered in eastern China and, given its diverse patient population, represents an ideal location to ascertain the perceived barriers to surgical care for both of these groups.
MATERIALS AND METHODS
Study setting and participants
The study was conducted at SCMC, one of the premiere tertiary care centers for neurosurgery in the PRC. Study participants were the birth or foster parents of children presenting to the office of the director for Pediatric Neurosurgery at SCMC, Nan Bao, MD for treatment of a NTD between the dates of 6/11/2014 and 7/17/2014. Given that Dr. Bao was seeing patients in differing stages of the treatment process, patients surveyed in a single day included those presenting to the clinic for the first time, those presenting for the operation itself or those in various stages of postoperative follow-up. Regardless of the stage of treatment a patient was in, anyone presenting during the study timeframe was considered eligible for the survey.
Additionally, patients presenting under the care of the Baobei Foundation, who were similarly at various stages of their treatment, were considered eligible participants. The Baobei Foundation orphans who were seen at SCMC prior to the 6/11/2014 start date and who had thorough documentation were also eligible for study inclusion, given that the chief of the foundation who coordinated the care of these prior patients was available for interview.
Survey design
A barriers to care survey was created with the assistance of an UCLA-based focus group consisting of Chinese immigrants from both rural and urban areas of the PRC in order to design a culturally relevant survey.
Survey administration
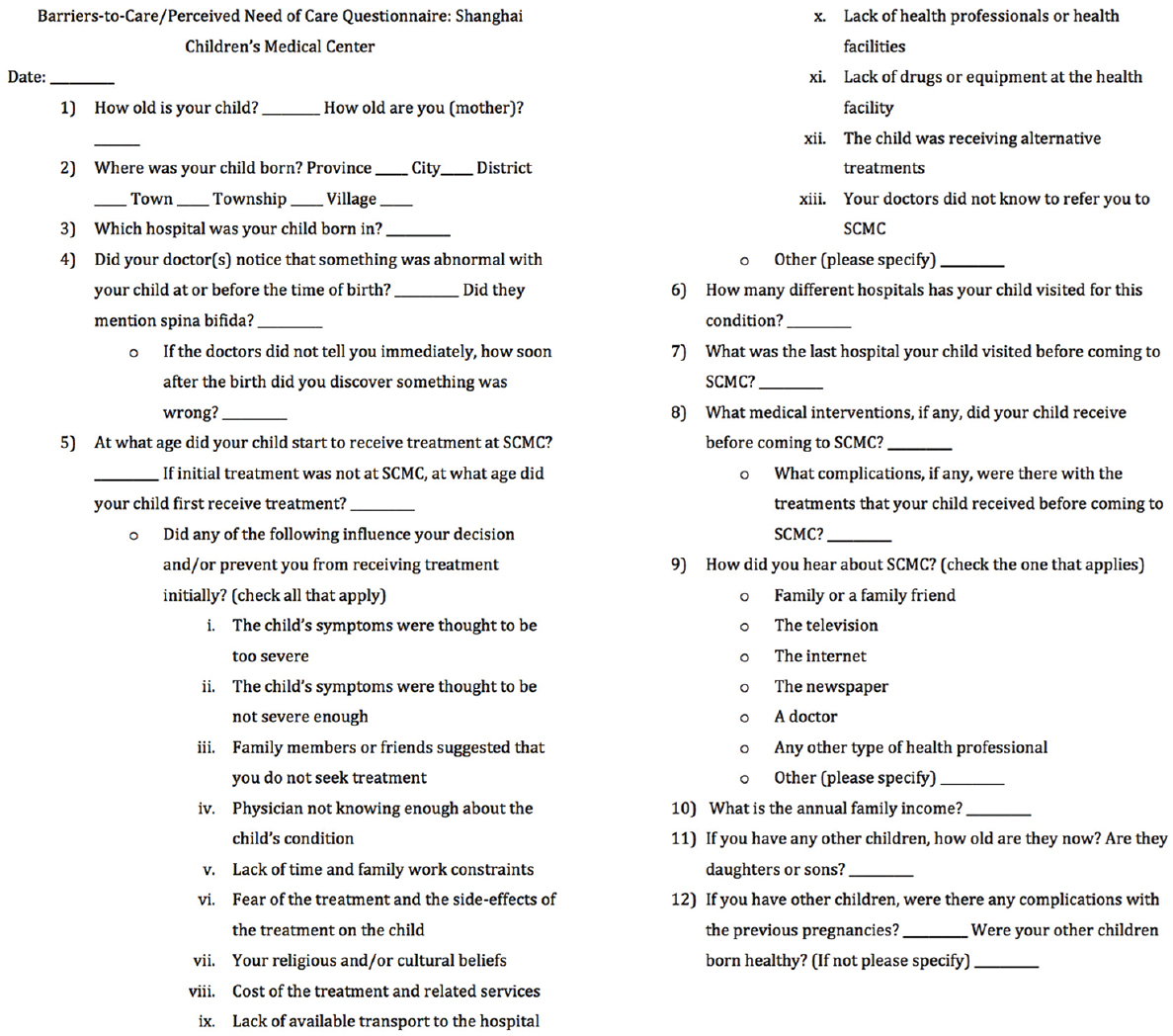
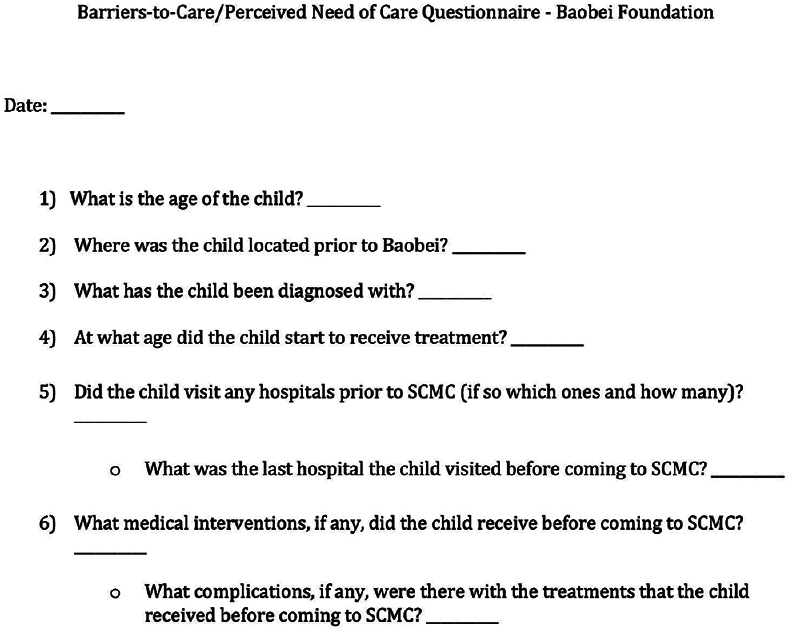
All surveys were administered in a room adjoining Dr. Bao's clinic after proper parental or guardian verbal consent was obtained. Participants were not paid for their participation and it was emphasized that their participation or lack of participation would in no way affect the quality or type of care received at SCMC. The interviewers were two MD candidates at the David Geffen School of Medicine, UCLA with graduate-level training in qualitative methods. A bilingual hospital staff member aided the interviewers in the survey administration. After providing written consent, all participants completed baseline demographic information in addition to a barrier to care questionnaire. The questionnaire consisted of a list of preformed options and participants were permitted to mark as many barriers as they deemed relevant to their experience, including an “other” option where they could elaborate on barriers not contained within the original list. Participants could refuse to answer any questions deemed too sensitive or intrusive. The questionnaire in English is presented in
Statistical analysis
The median length of time from birth to initial medical treatment was calculated for both the patients who presented with their families and for patients who presented through the Baobei Foundation. The significance in the difference between the median lengths of time for the groups was calculated using the bootstrapping method, given the non-Gaussian distribution of the data. Similarly, the significance in the difference between the median numbers of hospitals visited by each group was calculated using the bootstrapping method.
Additionally, the barriers to care options on the survey were numbered 1–14 and bootstrapped to calculate the frequency with which each barrier was selected by patients and families. In so doing, any potential correlation between barriers (e.g., barriers 1 and 2 being linked and chosen together more often than by chance alone) was accounted for, since each family's barrier choices were sampled as a unit as opposed to individually.
To evaluate for any correlation between the type of NTD diagnosed and the perceived barriers to care, a Fisher's exact test was performed, given the relatively small sample sizes within certain groups. In so doing, significance deviation from the null hypothesis could be calculated exactly. The Fisher's exact test was also used to evaluate for significant differences in malformation detection rates by referring physicians with respect to the type of NTD diagnosis.
RESULTS
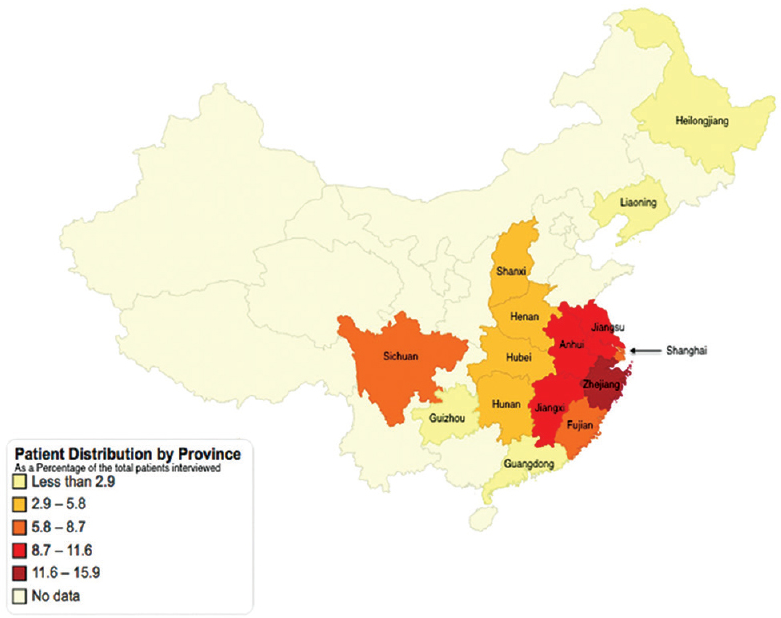
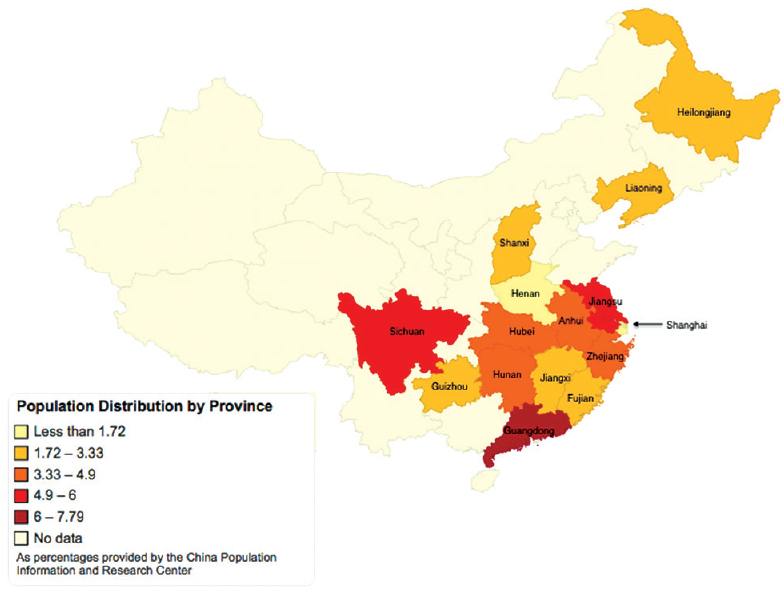
Over a 6-week period, a total of 69 families were interviewed. The patients came from 14 provinces in addition to the city of Shanghai itself, with the furthest province being 2277 km from Shanghai. The number of patients presenting from each province are presented in
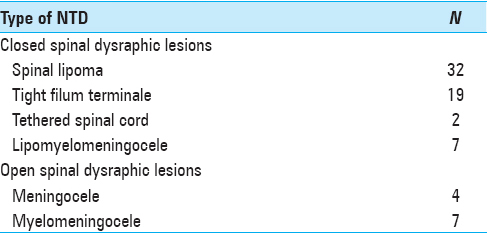
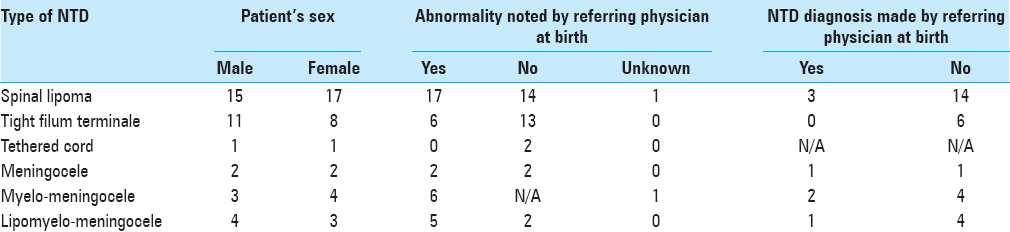
Of the 71 diagnoses seen, 36 reported that the referring physician noted an abnormality at or before the time of birth, 33 reported that the physician did not note any abnormality at or before the time of birth, and two were uncertain when the abnormality was noted. This data is presented in
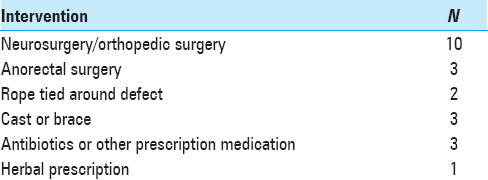
Among the 69 families, 18 children received some form of medical intervention related to their NTD or the sequelae of their disease prior to their arrival at SCMC. Four of the 18 children received two separate medical interventions prior to SCMC, amounting to a total of 22 interventions. The types of interventions recorded and their relative frequencies are presented in
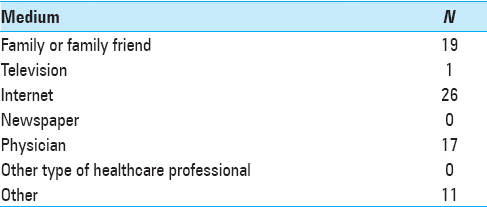
Additionally, each family was asked how they eventually heard about SCMC. All families except for one were willing to answer the question and six families chose two different options, for a total of 74 responses. The results are presented in
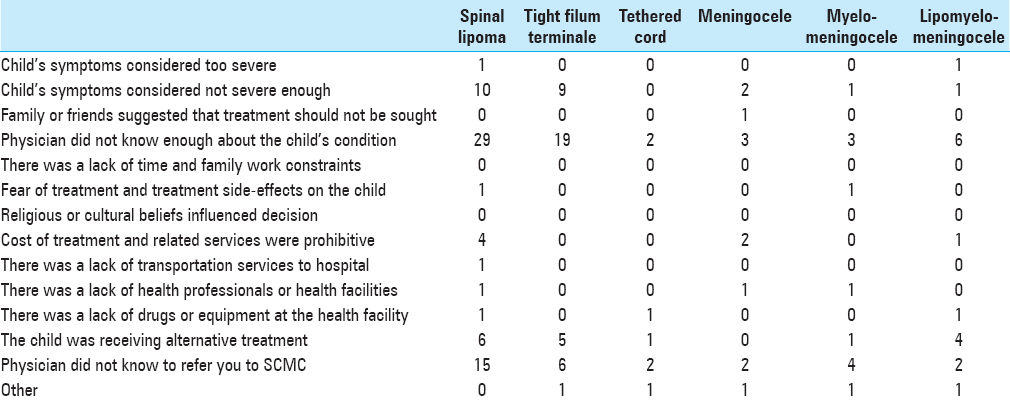
Regarding the different barriers to care for families, the most frequently chosen barrier, with a P value < 10-5, was that the referring physician did not know enough about the child's condition (options #4). The second most frequently chosen option, with a P value of 0.070, was that the physician did not know to refer to SCMC (option #13). When comparing the most frequently chosen barriers to care between different NTD types (i.e., spinal lipoma versus meningocele, etc.), the only group with a particular barrier chosen significantly more than any other group was lipomyelomeningocele. The families of patients with lipomyelomeningocele indicated on the survey that the patient was receiving alternative treatments (option #12) significantly more frequently than the other NTD groups, with a P value of 0.041. The overall frequency with which various barriers to care were selected by the different NTD groups is presented in
Among the Baobei Foundation orphans, 11 were identified as having been treated for a NTD, six of whom were male and five of whom were female. Ten of these patients were eventually diagnosed with myelomeningocele and one was diagnosed with meningocele. Survey data from patients presenting to SCMC with their families was compared to the data from patients presenting through the Baobei Foundation and two significant differences were found. First, the median age at initial treatment for the Baobei Foundation orphans was 1 month (ranging from 4 days to 5 months) and for children presenting with their families was 7 months (ranging from immediately after birth to 17 years), with a significant difference in the medians of P = 0.001. Second, the median number of hospitals visited (including SCMC) by the Baobei Foundation orphans was 1.0, while the median number of hospitals visited by children with their families was 3.14, a P value < 10-5.
DISCUSSION
Families seeking NTD treatment for their children had a less direct route to appropriate surgical care than children in the PRC orphanage system, as evidenced by a median of six additional months to time of treatment, and a median of two additional hospitals visited before SCMC, as compared to PRC orphans. Parents identified the referring physician(s) as the primary impediment to surgical care, either because they perceived the physician had an inadequate understanding of the disease process or because the physician missed an opportunity to refer to SCMC for further evaluation. Comparatively, PRC orphans experienced expedited medical care. The primary difference in their healthcare experience lies in the Baobei Foundation, a horizontal program whose members have well-established connections with physicians in urban-based tertiary medical centers. Using these relations, the Baobei employees coordinate with the orphanages so that they are immediately alerted to the health issues of any new arrivals and arrange their expedited delivery to appropriate tertiary care. Thus, delayed initial diagnosis and referral, the primary issues faced by the surveyed families, were effectively mitigated as significant barriers to surgical care for the PRC orphans.
To understand the primary barriers faced by one of these families, one must consider the position of the referring physicians. Appropriate management of patients with NTDs can be consolidated to three primary tasks: adequate prevision of preventative measures to the mother, accurate diagnosis of the disease should a NTD develop, and appropriate referral of the patient should the hospital not possess adequate means of treatment. Each of these areas has the potential to contribute to the parent's perceived barriers and each will be addressed subsequently.
In recent years the Chinese government has instituted sweeping healthcare reforms that have had a large effect both in the urban and rural settings.[
If a NTD does form in utero, the accurate diagnosis of the malformation is the referring physician's second hurdle. In the United States, the prenatal screening and diagnosis of NTDs is well established, with low-risk pregnancies being offered NTD screening in the form of a maternal serum alpha-fetoprotein (MSAFP) measurement at 16-18 weeks gestation or receiving a screening ultrasound at 18–20 weeks gestation. Characteristic findings on ultrasound are the backbone of the prenatal diagnostic process, should screening prove positive.[
The final task of the referring physician is to know when and where to refer the patient once the diagnosis has been made. The World Health Organization's 2012 service delivery profile of the PRC touched briefly on this topic by commenting on the segmentation of the health information system and the lack of a standardized nationwide referral protocol.[
Of note, defects with characteristically more obvious findings at birth (e.g., myelomeningocele) had significantly higher detection rates by referring physicians compared to defects with more inconspicuous features (e.g., tight filum terminale and tethered cord).[
Edmund Pellegrino, an acclaimed American bioethicist, has proposed seven models of a physician's responsibility toward his patients. The social functionary model is one such framework for evaluating the patient-physician relationship wherein physicians practice medicine to serve society as a whole when treating the individual patient.[
Recent studies analyzing the changing face of the patient-physician relationship over the previous several years describe its dissolution as a result of healthcare commercialization within the PRC.[
There are several limitations to the present study worth noting. First, given the small study size, limited to 69 children in one hospital in the PRC, generalizing these results to the entire PRC may be difficult. Additionally, the barriers to surgical care elicited from our surveyed families represent the insights of those who eventually arrived at a tertiary medical facility to receive treatment. The experiences of families who were unable to receive treatment or received treatment elsewhere may have yielded different perceived barriers had that population been interviewed. To our knowledge, there are no studies to date reviewing the rates of untreated NTDs, making the full spectrum of possible barriers difficult to surmise. Finally, the results of this study are the product of a preformed survey. Thus, while the referring physician was seen as a primary impediment to appropriate surgical care, study participants did not elaborate upon reasons for this perception.
CONCLUSION
The barriers to surgical care for NTDs in the PRC are complex. Further evaluation and eventual mitigation of those barriers requires the perspective of the affected patients and families. The results of this study highlight the referring physician as a primary barrier to care. The younger age at time of treatment for Baobei orphans born with NTDs supports this finding, as they essentially bypassed the referral process. An elaboration on reasons for this real or perceived barrier may provide insight into a means for expedited diagnosis and treatment of NTDs within the PRC.
Financial support and sponsorship
UCLA Center for World Health at the David Geffen School of Medicine.
Conflicts of interest
There are no conflicts of interest.
References
1. Blaas HG, Eik-Nes SH. Sonoembryology and early prenatal diagnosis of neural anomalies. Prenat Diagn. 2009. 29: 312-25
2. Blumenthal D, Hsiao W. Privatization and its discontents - The evolving Chinese health care system. N Engl J Med. 2005. 353: 1165-70
3. Brock DW, Wikler D, Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB.editors. Ethical Issues in Resource Allocation, Research, and New Product Development. Disease Control Priorities in Developing Countries. Washington (DC): World BankThe International Bank for Reconstruction and Development/The World Bank Group; 2006. p.
4. Cedergren M, Selbing A. Detection of fetal structural abnormalities by an 11-14-week ultrasound dating scan in an unselected Swedish population. Acta Obstet Gynecol Scand. 2006. 85: 912-5
5. Chen G, Song X, Ji Y, Zhang L, Pei L, Chen J. Prevention of NTDs with periconceptional multivitamin supplementation containing folic acid in China. Birth Defects Res A Clin Mol Teratol. 2008. 82: 592-6
6. Chen X, Fan R. The family and harmonious medical decision making: Cherishing an appropriate Confucian moral balance. J Med Philos. 2010. 35: 573-86
7. Cheschier N. ACOG practice bulletin. Neural tube defects. Number 44, July 2003. (Replaces committee opinion number 252, March 2001). Int J Gynaecol Obstet. 2003. 83: 123-33
8. Dane B, Dane C, Sivri D, Kiray M, Cetin A, Yayla M. Ultrasound screening for fetal major abnormalities at 11-14 weeks. Acta Obstet Gynecol Scand. 2007. 86: 666-70
9. Dillon CM, Davis BE, Duguay S, Seidel KD, Shurtleff DB. Longevity of patients born with myelomeningocele. Eur J Pediatr Surg. 2000. 10: 33-4
10. Driscoll DA, Gross SJ. Screening for fetal aneuploidy and neural tube defects. Genet Med. 2009. 11: 818-21
11. Greene ND, Copp AJ. Neural tube defects. Annu Rev Neurosci. 2014. 37: 221-42
12. Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: Cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. 2015. 100: 233-8
13. Jing W, Otten H, Sullivan L, Lovell-Simons L, Granek-Catarivas M, Fritzsche K. Improving the doctor-patient relationship in China: The role of balint groups. Int J Psychiatry Med. 2013. 46: 417-27
14. La Marca F, Grant JA, Tomita T, McLone DG. Spinal lipomas in children: Outcome of 270 procedures. Pediatr Neurosurg. 1997. 26: 8-16
15. Lew SM, Kothbauer KF. Tethered cord syndrome: An updated review. Pediatr Neurosurg. 2007. 43: 236-48
16. Liu J, Jin L, Meng Q, Gao L, Zhang L, Li Z. Changes in folic acid supplementation behaviour among women of reproductive age after the implementation of a massive supplementation programme in China. Public Health Nutr. 2015. 18: 582-8
17. Lo A, Polsek D, Sidhu S. Estimating the burden of neural tube defects in low- and middle-income countries. J Glob Health. 2014. 4: 010402-
18. Lu QB, Wang ZP, Gong R, Sun XH, Gao LJ, Zhao ZT. Investigation of ultrasound screening efficiency for neural tube defects during pregnancy in rural areas of China. Public Health. 2011. 125: 639-44
19. McLone DG. Care of the neonate with a myelomeningocele. Neurosurg Clin N Am. 1998. 9: 111-20
20. Munro DThe Concept of Man in Early China: University of Michigan Center for Chinese Studies. 2001. p.
21. Ozgediz D, Poenaru D. The burden of pediatric surgical conditions in low and middle income countries: A call to action. J Pediatr Surg. 2012. 47: 2305-11
22. Pellegrino ED, Lounsbury DE.editors. The Moral Foundations of the Patient-Physician Relationship: The Essence of Medical Ethics. Military Medical Ethics. Washington D.C: Office of the Surgeon General, Department of the Army; 2003. 1 1: 3-21
23. Pierre-Kahn A, Zerah M, Renier D, Cinalli G, Sainte-Rose C, Lellouch-Tubiana A. Congenital lumbosacral lipomas. Childs Nerv Syst. 1997. 13: 298-334
24. Po-Wah JTL, Renzong Q. Confucian and Western Notions of Human Need and Agency: Health Care and Biomedical Ethics in the Twenty- First Century. Bioethics: Asian Perspectives: A Quest for Moral Diversity. Philosophy and Medicine 80: Springer Science. 2004. p. 13-28
25. Qiu R. Economics and medical decision-making: A Chinese perspective. Semin Perinatol. 1987. 11: 262-3
26. Racusin D, Stevens B, Campbell G, Aagaard KM. Obesity and the risk and detection of fetal malformations. Semin Perinatol. 2012. 36: 213-21
27. Ren AG. Prevention of neural tube defects with folic acid: The Chinese experience. World J Clin Pediatr. 2015. 4: 41-4
28. Renna MD, Pisani P, Conversano F, Perrone E, Casciaro E, Renzo GCD. Sonographic markers for early diagnosis of fetal malformations. World J Radiol. 2013. 5: 356-71
29. Rossi AC, Prefumo F. Accuracy of ultrasonography at 11-14 weeks of gestation for detection of fetal structural anomalies: A systematic review. Obstet Gynecol. 2013. 122: 1160-7
30. Saltvedt S, Almstrom H, Kublickas M, Valentin L, Grunewald C. Detection of malformations in chromosomally normal fetuses by routine ultrasound at 12 or 18 weeks of gestation-a randomised controlled trial in 39,572 pregnancies. BJOG. 2006. 113: 664-74
31. Sewell MJ, Chiu YE, Drolet BA. Neural tube dysraphism: Review of cutaneous markers and imaging. Pediatr Dermatol. 2015. 32: 161-70
32. Tarcan T, Onol FF, Ilker Y, Alpay H, Simsek F, Ozek M. The timing of primary neurosurgical repair significantly affects neurogenic bladder prognosis in children with myelomeningocele. J Urol. 2006. 176: 1161-5
33. Tucker JD, Cheng Y, Wong B, Gong N, Nie JB, Zhu W. Patient-physician mistrust and violence against physicians in Guangdong Province, China: A qualitative study. BMJ Open. 2015. 5: e008221-
34. cited 2016 Jul 28. Available from: http://www.wpro.who.int/health_services/service_delivery_profile_china.pdf?ua = 1 .
35. Xiao KZ, Zhang ZY, Su YM, Liu FQ, Yan ZZ, Jiang ZQ. Central nervous system congenital malformations, especially neural tube defects in 29 provinces, metropolitan cities and autonomous regions of China: Chinese Birth Defects Monitoring Program. Int J Epidemiol. 1990. 19: 978-82
36. Zhang X, Sleeboom-Faulkner M. Tensions between medical professionals and patients in mainland China. Camb Q Healthc Ethics. 2011. 20: 458-65
37. Zhao X, Wang P, Tao X, Zhong N. Genetic services and testing in China. J Community Genet. 2013. 4: 379-90
38. Zhou L, Nunes MB. Barriers to knowledge sharing in Chinese healthcare referral services: An emergent theoretical model. Glob Health Action. 2016. 9: 29964-
39. Zhu L, Ling H. National Neural Tube Defects Prevention Program in China. Food Nutr Bull. 2008. 29: S196-204