- Clinical Professor of Neurological Surgery, , School of Medicine, State University of New York at Stony Brook, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suit 106, Garden City, NY 11530, United States.
Correspondence Address:
Nancy Epstein,Clinical Professor of Neurosurgery, School of Medicine, State U of NY at Stony Brook, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY 11530, United States.
DOI:10.25259/SNI_402_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy Epstein. A perspective on wrong level, wrong side, and wrong site spine surgery. 14-Jun-2021;12:286
How to cite this URL: Nancy Epstein. A perspective on wrong level, wrong side, and wrong site spine surgery. 14-Jun-2021;12:286. Available from: https://surgicalneurologyint.com/surgicalint-articles/10881/
Abstract
Background: Four of the most common “errors” in spine surgery include: operating on the wrong patient, doing the wrong procedure, performing wrong-level surgery (WLS), and/or performing wrong-sided surgery (WSS). Although preoperative verification protocols (i.e. Universal Protocol, routine Time-Outs, and using the 3 R’s (i.e. right patient, right procedure, right level/side)) have largely limited the first two “errors,” WLS and WSS still occur with an unacceptably high frequency.
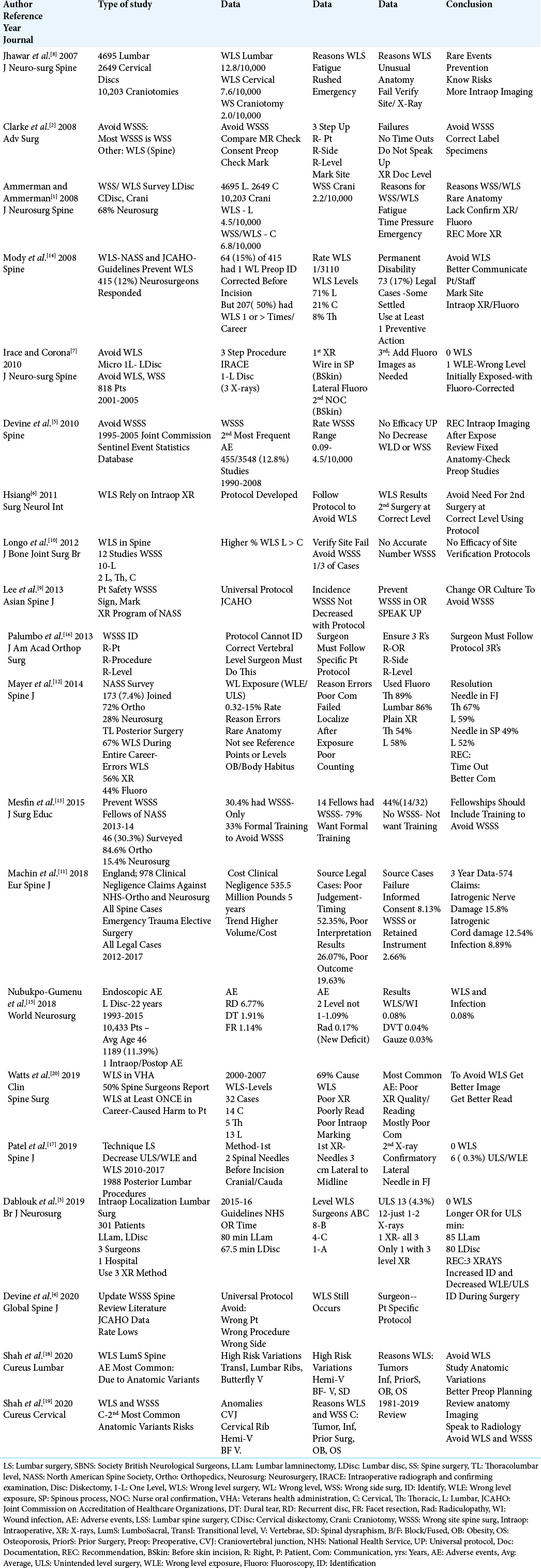
Methods: In 20 studies, we identified the predominant factors contributing to WLS/WSS; unusual/anatomical anomalies/variants (i.e. sacralized lumbar vertebrae. lumbarized sacral vertebra, Klippel-Feil vertebrae, block vertebrae, butterfly vertebrae, obesity/morbid obesity), inadequate/poor interpretation of X-rays/fluoroscopic intraoperative images, and failure to follow different verification protocols.
Results: “Human error” was another major risk factor contributing to the failure to operate at the correct level/side (WLS/WSS). Factors comprising “human error” included; surgeon/staff fatigue, rushing, emergency circumstances, lack of communication, hierarchical behavior in the operating room, and failure to “speak up”.
Conclusion: Utilizing the Universal Protocol, routine Time Outs, and the 3 R’s largelly avoid operating on the wrong spine patient, and performing the wrong procedure. However, these guidelines have not yet sufficiently reduced the frequently of WLS and WSS. Greater recognition of the potential pitfalls contributing to WLS/WSS as reviewed in this perspective should better equip spine surgeons to avert/limit such “errors” in the future.
Keywords: Lumbar surgery, Multiple intraoperative X-ray/fluoroscopy techniques, Right level, Right patient, Right procedure, Right (Correct) side, Universal Protocols, Avoid Wrong Level (WLS)/Wrong Side Spine Surgery (WSS)
INTRODUCTION
Four of the most common “errors” in spine surgery include: operating on the wrong patient, performing the wrong procedure, operating at the wrong-level (WLS), and operating on the wrong-side (WSS) (i.e. includes wrong site surgery (WSS) as well).[
INCIDENCE OF WRONG LEVEL SURGERY (WLS)
Wrong level spine surgery (WLS) is not that rare. [
INCIDENCE OF WLS FOR INDIVIDUAL SPINAL SURGEONS OVER THEIR ENTIRE CAREERS
Notably, 50–67% of spine surgeons have directly experienced WLS over their careers [
FREQUENCY OF INITIAL WRONG LEVEL EXPOSURE (WLE) OR UNINTENDED LEVEL SURGERY (ULS)
Little attention has been given to the 0.3–4.3–15% incidence of initial wrong level exposure (WLE) or unintended level spine surgery (ULS). WLE/ULS is defined by recognizing during the index procedure that the initially exposed level was incorrect, but that this “error” was corrected prior to closure [
USE OF THE UNIVERSAL PROTOCOL, TIME OUTS, AND THE 3 R’S TO AVOID WRONG LEVEL SURGERY (WLS), WRONG SIDE SURGERY (WSS), AND WRONG SITE SURGERY (WSSS)
Multiple protocols (i.e. Universal Protocol- JCAHO (Joint Commission on Accreditation of Healthcare Organizations), Time Outs, and the 3R’s) are aimed at avoiding WLS, WSS, and WSSS [
REASONS THE UNIVERSAL PROTOCOL, TIME OUTS, AND 3 R’S FAIL TO AVOID WLS, WSS, AND WSSS
There are multiple causes for the “errors” resulting in WLS, WSS, and WSSS.[
WHICH SPINAL LEVELS ARE MORE SUSCEPTIBLE TO WLS?
Most series documented a higher incidence of WLS involving the lumbar rather than the cervical spine [
AVOIDANCE OF WLS
Multiple authors offered general recommendations for avoiding WLS in the spine.[
Avoidance of WLS with Double Intraoperative X-ray Technique
Patel et al. (2019) recommended that spinal surgeons utilize a double intraoperative X-ray technique to avoid WLS (2010–2017; 1988 posterior lumbar cases).[
Avoidance of WLS Using a Tricple X-ray Method
Other authors used at least 3 intraoperative films to avoid WLS and WLE/ULS [
Author’s 3-4 X-ray Technique to Avoid WLS, WSS, WSSS, and WLE/ULS
Epstein’s recommendation to avoid WLS, WSS, WSSS, and WLE/ULS includes a 3–4 X-ray technique, First, the patient is prepared/draped, and the first Time Out is obtained (i.e. using the 3 R’s to confirm the right patient, right procedure, right level/side). Next, a sterile 18-gauge needle is percutaneously introduced into either a spinous process or an interspinous ligament; the first lateral fluoroscopic image is then interpreted/verified both by the operating surgeon and the assistant (i.e. Physician Assistant/Physician, other). This is followed by a 2nd Time Out. After initial exposure of the wound, a clamp is placed either on a spinous process or an interspinous ligament; the 2nd film is verified both by the operating surgeon and assistant. This if followed by a 3rd Time Out. Note, the patient’s films on the board or TV screen must additionally be consulted to verify the correct operative site/level. Subsequently, for a disc herniation a 3rd intraoperative film is typically obtained with a Penfield elevator in the disc space. Alternatively, if a laminectomy has been performed for stenosis, the 3rd X-ray typically requires the placmeent of either a Penfield elevator or dental too at the most cephalad and caudad ends of the operative decompression (i.e. to further confirm operative levels). Notably, if fusions are being performed, there are typically many additional intraoperative fluoroscopic images taken during the course of surgery to confirm the correct level/ placement of instrumentation.
INCIDENCE OF WRONG SIDE SURGERY
Clarke et al. (2008) cited WSS as largely attributable to the failure to use the 3 R protocol; right patient, right level, right side, plus the failure to appropriately mark the operative site preoperatively.[
IS THERE INTEREST IN FORMAL TRAINING TO AVOID WRONG SITE SURGERY?
Mesfin et al. (2015) asked spinal fellows (i.e. through NASS: North American Spine Society) to participate in a survey regarding WSSS; 46 fellows responded.[
IMPORT OF MEDICOLEGAL SUITS AND COSTS OF WRONG SITE SURGERY
There can be significant medicolegal repercussions of WSSS.[
CONCLUSION
The most typical reasons for WLS, WSS, and WSSS include; unusual anatomical variations, failure to follow level/site/ side verification protocols (i.e. the Universal Protocol, Time Outs, and 3 R’s), and “human error”. Remaining vigilant in recognizing the different factors that contribute to WLS, WSS, and WSSS should reduce their incidence in the future.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Commentary
Jamie Baisden, M.D., Professor of Neurosurgery, Medical College of Wisconsin
Milwaukee WI 53226
The rule, measure three times, and cut once, has been an intraoperative standard for my practice. Certainly, junctional anatomy is particularly problematic, and intraoperative X-rays are often suboptimal. Use of oblique fluoroscopy and/or O-arm are helpful in morbidly obese, short necked/wide shouldered patients to prevent wrong level surgery (WLS).
How to Avoid Thoracic WLS By Placing A Coil in the “Correct” Pedicle
WLS is estimated to occur in up to10% of procedures addressing thoracic discs. Use of interventional radiology to place a coil in or near the “correct” pedicle (i.e. including the “correct” side and level of the proposed procedure) has been useful. First, the marking does not wash off like with the preoperative marking pens. Second, the fluoroscopy equipment in the radiology department is typically of better quality than the portable units in the operative suite. Importantly, this additional “procedure” is covered by most insurances and, although more expensive, is very accurate, and may avoid WLS.
Localization Issues with Minimally Invasive Surgery (MIS)
On a smaller scale, minimally invasive surgery has its own set of localization issues (i.e. as with the wanding technique to clear the interlaminar/facet junction). Residual soft tissue and/or a sub-optimally tightened retractors applied during docking may result in slippage. Here, a 1 cm arc at the skin may produce up to a 2–3 level error in the lumbar spine, and even greater level errors in the cervical spine.
Intradural Tumor Resection Utilizing Ultrasound For Site Confirmation
Lastly, for intradural lesions, a quick intraoperative ultrasound after the bony decompression allows for verification that the exposure is adequate while also allowing for level/lesion confirmation.
Conclusion
More thought and intraoperative preparation makes for safer surgery, and the avoidance of WLS, WSS, and WSSS.
Commentary
Benjamin R. Cohen MD; Adjunct Assistant Professor, Department of Neurology, School of Medicine, NYU Long Island School of Medicine, NY 11501
Dr. Mark Agulnick
Adjunct Associate Professor of Orthopedic Surgery, Department of Orthopedics, NYU Long Island School of Medicine, NY 11501
Two spinal surgeons, one a neurosurgeon and the other an orthopedist, offer the following points regarding how to avoid wrong level (WLS), wrong side (WSS), and wrong site spinal surgery (WSSS). They both emphasized the following major points.
Preoperative planning Get as many plain films as needed Correlate plain films and CT with the preoperative MR Especially on complex cases, those with anticipated vertebral anomalies, or with problematic physiognomy). Preoperatively review the films (X-rays, MR, CT) with the radiologist/neuroradiologist to clarify the pathology and levels Particularly regarding L5-S1 anomalies Do not be afraid to ask the technologist in the operating room to repeat films Do this as many times as needed where the quality and or level are not clear For multilevel cervical and/or lumbar laminectomies The levels requiring decompression should be confirmed by at least 2 participants (i.e. primary surgeon and assistant surgeon/Physician Assistant) There are instances in which the decompression should be continued based on the intraoperative pathology (i.e. extent of stenosis), not just on the preoperative radiographic imaging studies Penfield or Woodson should be placed in a disc space to confirm a level This especially applies to disc/far lateral disc surgery There are multiple localization techniques The BEST way to localize in the lumbar spine is to put the marker in the pedicle The NEXT BEST technique is to put a Kocher on the correct facet The WORST technique is to put a marker on a spinous process Cervical surgery localization (particularly posterior procedures) may be very difficult Especially with lateral mass screws at the C3 or C4 levels, or C6, C7, T1 levels Thoracic Surgery Localization may be uniquely problematic Most patients are on a Jackson table Best Technique: Use AP Fluoroscopy to count ribs for level confirmation Next Best: Put a clamp on a facet Obtain a wide film to see T12 and count up Note: some patients have anomalous rib counts For ELECTIVE Thoracic Surgery Send the patient for preoperative CT localization Inject the skin and interspinous ligament with methylene blue Obtain additional intraoperetive AP fluoroscopic confirmation of the level Before the incision put a spinal needle into the correct facet joint and take a film Open the incision and take another film to confirm/correlate the level Intradural Tumor Localization Confirmation Do all the above maneuvers especially for thoracic tumor localization Before opening the dura, obtain intraoperative ultrasound to confirm the tumor location Spinal Surgical Localization Multiple techniques involve reepated checks and balances Having two surgeons in the operating room where both must agree Will help confirm the correct level and correct side and site of surgery
References
1. Ammerman JM, Ammerman MD. Wrong-sided surgery. J Neurosurg Spine. 2008. 9: 105-6
2. Clarke JR, Johnston J, Blanco M, Martindell DP. Wrong-site surgery: Can we prevent it?. Adv Surg. 2008. 42: 13-31
3. Dablouk MO, Sajjad J, Lim C, Kaar G, O’Sullivan MG. Intra-operative imaging for spinal level localization in lumbar surgery. Br J Neurosurg. 2019. 33: 352-6
4. Devine JG, Chutkan N, Gloystein D, Jackson K. An update on wrong-site spine surgery. Global Spine J. 2020. 10: 41S-4S
5. Devine J, Chutkan N, Norvell DC, Dettori JR. Avoiding wrong site surgery: A systematic review. Spine (Phila Pa 1976). 2010. 35: S28-36
6. Hsiang J. Wrong-level surgery: A unique problem in spine surgery. Surg Neurol Int. 2011. 2: 47
7. Irace C, Corona C. How to avoid wrong-level and wrong-side errors in lumbar microdiscectomy. J Neurosurg Spine. 2010. 12: 660-5
8. Jhawar BS, Mitsis D, Duggal N. Wrong-sided and wrong-level neurosurgery: A national survey. J Neuorsurg Spine. 2007. 7: 467-72
9. Lee SH, Kim JS, Jeong YC, Kwak KD, Chun JH, Lee HM. Patient safety in spine surgery: Regarding the wrong-site surgery. Asian Spine J. 2013. 7: 63-71
10. Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V. Errors of level in spinal surgery: An evidence-based systematic review. J Bone Joint Surg Br. 2012. 94: 1546-50
11. Machin JT, Hardman J, Harriwon W, Briggs TW, Hutton M. Can spinal surgery in England be saved from litigation: A review of 978 clinical negligence claims against the NHS. Eur Spine J. 2018. 27: 2693-9
12. Mayer JE, Dang RP, Prieto GF, Cho SK, Qureshi SA, Hecht AC. Analysis of the techniques for thoracic-and lumbar-level localization during posterior spine surgery and the occurrence of wrong-level surgery: Results from a national survey. Spine J. 2014. 14: 741-8
13. Mesfin A, Canham C, Okafor L. Prevention training of wrong-site spine surgery. J Surg Educ. 2015. 72: 680-4
14. Mody MG, Nourbakhsh A, Stahl DL, Gibbs M, Alfawareh M, Garges KJ. The prevalence of wrong level surgery among spine surgeons. Spine. 2008. 33: 194-8
15. Nubukpo-Gumenu AA, Segbedji FK, Rue M, Destaudau J. Endospine surgery complications in lumbar herniated disc. World Neurosurg. 2018. 119: e78-9
16. Palumbo MA, Bianco AJ, Esmende S, Daniels AH. Wrong-site spine surgery. J Am Acad Orthop Surg. 2013. 21: 312-20
17. Patel A, Runner RP, Bellamy JT, Rhee JM. A reproducible and reliable localization technique for lumbar spine surgery that minimizes unintended-level exposure and wrong-level surgery. Spine J. 2019. 19: 773-80
18. Shah M, Halalmeh DR, Sandio A, Tubbs RS, Moisi MD. Anatomical variations that can lead to spine surgery at the wrong level: Part I, cervical spine. Cureus. 2020. 12: e8667
19. Shah M, Halalmeh DR, Sandio A, Tubbs RS, Moisi MD. Anatomical variations that can lead to spine surgery at the wrong level: Part III lumbosacral spine. Cureus. 2020. 12: e9433
20. Watts BV, Rachlin JR, Gunnar W, Mills PD, Neily J, Soncrant C. Wrong site spine surgery in the veterans administration. Clin Spine Surg. 2019. 32: 454-7