- Department of Neurosurgery, Salford Royal Foundation Trust, Manchester, United Kingdom.
Correspondence Address:
M Saleemi, Department of Neurosurgery, Salford Royal Foundation Trust, Manchester, United Kingdom.
DOI:10.25259/SNI_947_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: M Saleemi, Sahibzada Abrar, Muhammad SA Dherijha, K. Joshi George. A postoperative complication of lumbar discectomy: A discal/annular cyst. 09-Dec-2022;13:572
How to cite this URL: M Saleemi, Sahibzada Abrar, Muhammad SA Dherijha, K. Joshi George. A postoperative complication of lumbar discectomy: A discal/annular cyst. 09-Dec-2022;13:572. Available from: https://surgicalneurologyint.com/surgicalint-articles/12051/
Abstract
Background: A postoperative discal/annular cyst following lumbar discectomy may reproduce the symptoms/signs of a recurrent lumbar disc herniation (i.e., back pain and radiculopathy).
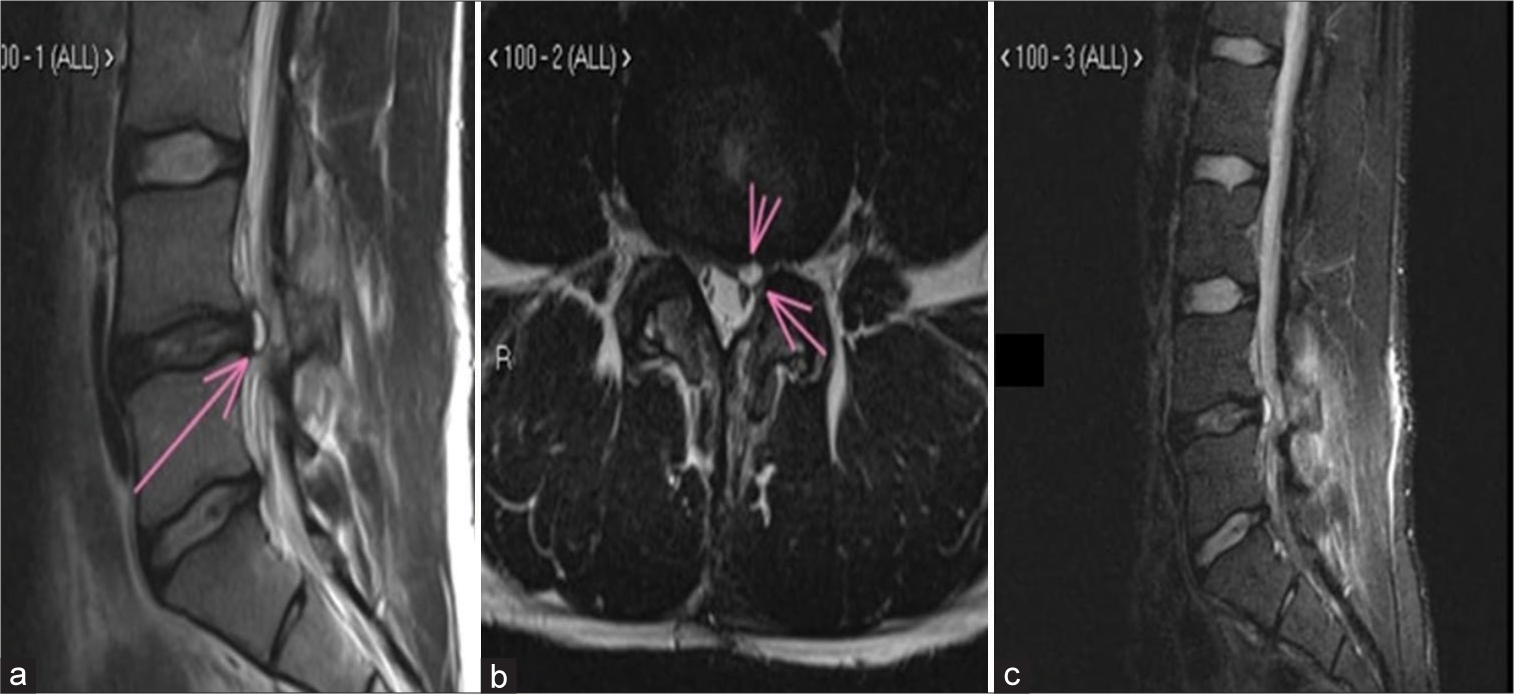
Case Description: A 21-year-old rugby player developed leg pain after an uncomplicated lumbar microdiscectomy. The repeat lumbar magnetic resonance imaging confirmed a postoperative lumbar annular/ discal cyst, for which he underwent repeat surgery. The diagnosis was further confirmed histopathologically at surgery.
Conclusion: Although rare, postoperative discal/annular cysts may be potential causes of recurrent postoperative pain and lumbar radiculopathy mimicking recurrent disc herniations.
Keywords: Annular cyst, Back pain, Disc herniation, Discal cyst, Radiculopathy
INTRODUCTION
Postoperative annular cysts may reproduce symptoms and signs (i.e., low back pain and radiculopathy) similar to recurrent disc herniations.[
CASE PRESENTATION
A 21-year-old rugby player underwent an uncomplicated discectomy at the L4/5 level [
Literature review
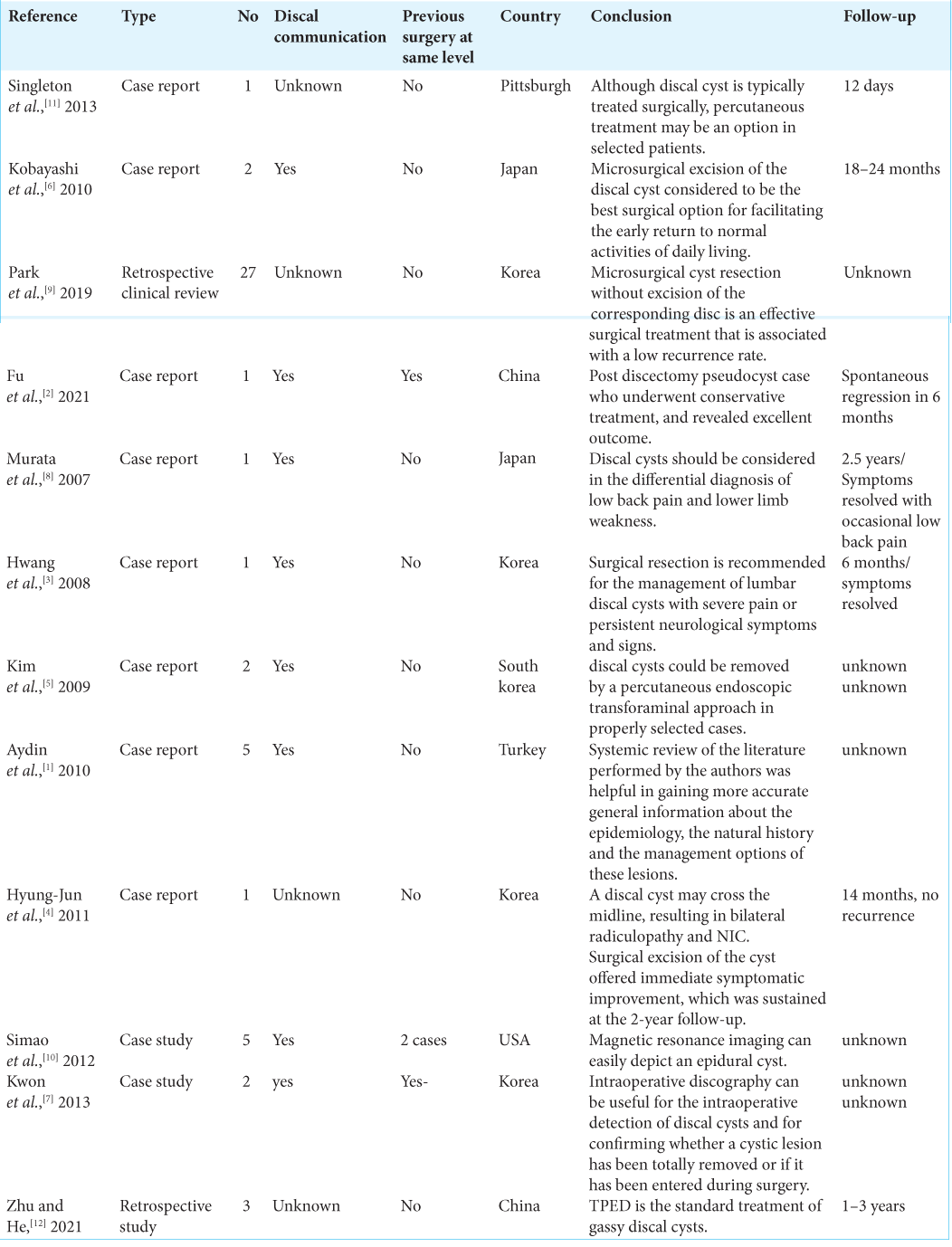
From 2007 to 2021, we found 20 reports involving 37 patients with similar postoperative discal cysts [
DISCUSSION
Discal cysts, known as a pre-membranous hematomas, are extremely rare lesions. Notably, they are directly related to synovial cysts, ganglion cysts, and Tarlov perineural cysts.[
Treatment of discal/annular cysts
Multiple modalities have been utilized to treat the symptoms/signs of discal/annular cysts.[
CONCLUSION
Postoperative discal cysts can present with the classical signs and symptoms of recurrent lumbar disc herniation. Optimal management typically includes direct surgical resection rather than often reported failed attempts at cyst aspiration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aydin S, Abuzayed B, Yildirim H, Bozkus H, Vural M. Discal cysts of the lumbar spine: Report of five cases and review of the literature. Eur Spine J. 2010. 19: 1621-6
2. Fu CF, Tian ZS, Yao LY, Yao JH, Jin YZ, Liu Y. Postoperative discal pseudocyst and its similarities to discal cyst: A case report. World J Clin Cases. 2021. 9: 1439-45
3. Hwang JH, Park IS, Kang DH, Jung JM. Discal cyst of the lumbar spine. J Korean Neurosurg Soc. 2008. 44: 262-4
4. Hyung-Jun K, Dae-Yong K, Tae-Ho K, Ho-Sang P, Jae-Sung K, Jae-Won J. Lumbar discal cyst causing bilateral radiculopathy. Surg Neurol Int. 2011. 2: 21
5. Kim JS, Choi G, Lee CD, Lee SH. Removal of discal cyst using percutaneous working channel endoscope via transforaminal route. Eur Spine J. 2009. 18: 201-5
6. Kobayashi S, Takeno K, Uchida K, Yayama T, Nakajima H, Miyazaki T. Pathogenesis of the discal cysts communicating with an adjacent herniated disc. Histological and ultrastructural studies of two cases. Joint Bone Spine. 2010. 77: 184-6
7. Kwon YK, Choi KC, Lee CD, Lee SH. Intraoperative discography for detecting concealed lumbar discal cysts. J Korean Neurosurg Soc. 2013. 53: 255-7
8. Murata K, Ikenaga M, Tanaka C, Kanoe H, Okudaira S. Discal cysts of the lumbar spine: A case report. J Orthop Surg (Hong Kong). 2007. 15: 376-9
9. Park JW, Lee BJ, Jeon SR, Rhim SC, Park JH, Roh SW. Surgical treatment of lumbar spinal discal cyst: Is it enough to remove the cyst only without following discectomy?. Neurol Med Chir (Tokyo). 2019. 59: 204-12
10. Simao MN, Helms CA, Richardson WJ. Magnetic resonance imaging findings of disc-related epidural cysts in nonsurgical and postoperative microdiscectomy patients. Radiol Brasil. 2012. 45: 205-9
11. Singleton A, Agarwal V, Casagranda B, Hughes MA, Rothfus WE. Lumbar discal cyst in an elite athlete. Radiol Case Rep. 2015. 8: 764
12. Zhu K, He D. Transforaminal percutaneous endoscopic discectomy for symptomatic gas-filled discal cysts-report of three cases and literature review. J Orthop Surg Res. 2021. 16: 251