- Departments of Neurosurgery and Neuro-Oncology, National Cancer Center Hospital, Tsukiji, Chuo-ku, Japan.
- Departments of Gastrointestinal Medical Oncology, National Cancer Center Hospital, Tsukiji, Chuo-ku, Japan.
- Departments of Diagnostic Pathology, National Cancer Center Hospital, Tsukiji, Chuo-ku, Japan.
- Department of Surgery, Denenchofu Central Hospital, Denentyoufu, Ota-ku, Tokyo, Japan.
Correspondence Address:
Yoshitaka Narita
Departments of Neurosurgery and Neuro-Oncology, National Cancer Center Hospital, Tsukiji, Chuo-ku, Japan.
DOI:10.25259/SNI_413_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Erika Yamazawa, Yoshitaka Honma, Kaishi Satomi, Hirokazu Taniguchi, Masamichi Takahashi, Akihiko Yoshida, Koji Tominaga, Yasuji Miyakita, Makoto Ohno, Taku Asanome, Natsuko Satomi, Yoshitaka Narita. A rare case of brain metastasis from poorly differentiated small bowel adenocarcinoma. 27-Dec-2019;10:256
How to cite this URL: Erika Yamazawa, Yoshitaka Honma, Kaishi Satomi, Hirokazu Taniguchi, Masamichi Takahashi, Akihiko Yoshida, Koji Tominaga, Yasuji Miyakita, Makoto Ohno, Taku Asanome, Natsuko Satomi, Yoshitaka Narita. A rare case of brain metastasis from poorly differentiated small bowel adenocarcinoma. 27-Dec-2019;10:256. Available from: https://surgicalneurologyint.com/surgicalint-articles/9822/
Abstract
Background: Small bowel adenocarcinoma (SBA) accounts for et al. reported 1 case of brain metastasis out of 217 SBA cases, but details of the clinical course of the case were unclear. Our case might be the first report covering the full clinical course, pathological findings, and genetic data. Here, we report a very rare case of brain metastasis from poorly differentiated SBA.
Case Description: A 54-year-old man who suffered from abdominal pain and melena visited a nearby hospital. This patient had no risk factors for SBA. He underwent partial resection of the jejunum with regional lymphadenectomy and combined resection of the transverse colon. Pathological diagnosis was poorly differentiated adenocarcinoma, pT4N2M0 Stage IIIB (UICC-TNM: 8th edition). One month after curative surgery, liver metastasis was detected by a computed tomography (CT) scan, and then, palliative chemotherapy was started. During the third-line chemotherapy, a brain tumor on the left cerebellum was detected by the CT scan. Tumor resection was performed, and the histopathological features coincided with the primary jejunum tumor. Based on surgical, radiological, pathological, and genetic findings, this brain tumor was comprehensively diagnosed as a metastasis from poorly differentiated SBA.
Conclusion: Here, we experienced a very rare case of brain metastasis from poorly differentiated SBA.
Keywords: Brain metastases, Jejunum, Metastatic brain tumor, Small bowel, Small intestine
INTRODUCTION
Small bowel adenocarcinoma (SBA) is an extremely rare tumor, accounting for <2% of all gastrointestinal tumors. Its annual incidence rate is 1.2–6.5/1 million people.[
CASE REPORT
A 54-year-old man who suffered from abdominal pain and melena visited a nearby hospital. He had a medical history of hyperlipidemia and diabetes but had no risk factors for SBA. After clinical evaluation, a jejunum tumor was suspected. In July 2017, he underwent partial resection of the jejunum with regional lymphadenectomy and combined resection of the transverse colon. The transverse colon was attached to the jejunum tumor and they could not be separated. The jejunum tumor was approximately 10 cm caudal to Treitz ligament. Pathological diagnosis was poorly differentiated adenocarcinoma, pT4N2M0 Stage IIIB [UICC-TNM: 8th edition;
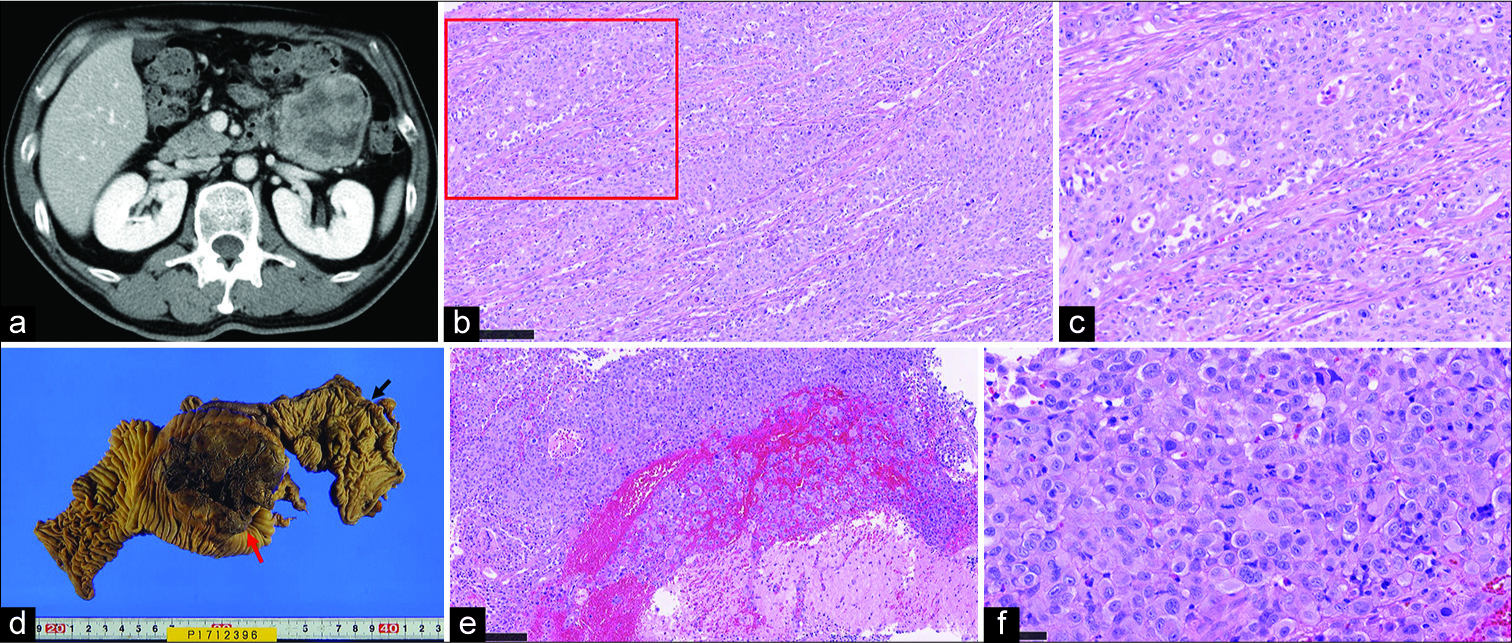
Figure 1:
(a) Contrast computed tomography preoperative imaging of jejunum. (b) Pathology of the primary jejunum lesion, hematoxylin- eosin (HE) staining, low magnification. Poorly differentiated small bowel adenocarcinoma is proliferating solidly. The scale bar is 250 µm. (c) Pathology of the primary jejunum lesion, HE staining, high magnification. There was nuclear atypia, pleomorphism, and prominent nucleoli. The scale bar is 250 µm. (d) Jejunum tumor (red arrow), invading transverse colon (black arrow). (e) Pathology of the cerebellum lesion, HE staining, low magnification. Cerebellum histopathology is seen in the lower right of the screen; there is poorly differentiated adenocarcinoma metastasis. The scale bar is 250 µm. (f) Pathology of the cerebellum lesion, HE staining, high magnification. The histopathological feature of the left cerebellum lesion coincided with that of the primary jejunum lesion. There were nuclear atypia, pleomorphism, and prominent nucleoli. The pathological diagnosis was poorly differentiated small bowel adenocarcinoma metastasis. The scale bar is 50 µm.
In August 2017, he was referred to our hospital for the purpose of adjuvant treatment. However, due to a liver metastasis detected by a computed tomography (CT) scan at the time of admittance, palliative chemotherapy using capecitabine and oxaliplatin (CAPOX) was selected. However, the efficacy of CAPOX and second-line FOLFIRI (5-fluoropyrimidine/ leucovorin/irinotecan) chemotherapy was limited.
In April 2018, during the course of the third-line chemotherapy using nab-paclitaxel, he presented with dizziness, followed by headache, nausea, and ataxia symptoms which were remarkable. Magnetic resonance imaging (MRI) revealed a cystic lesion with a major axis of 38 mm attached to the tent in the left cerebellum. The lesion had weak contrast effect and was accompanied by edema. Tumor resection was performed for symptom control. The contents of the cyst were old brownish hematoma-like liquid with nodular lesions.
The pathological diagnosis revealed brain metastasis of poorly differentiated SBA [
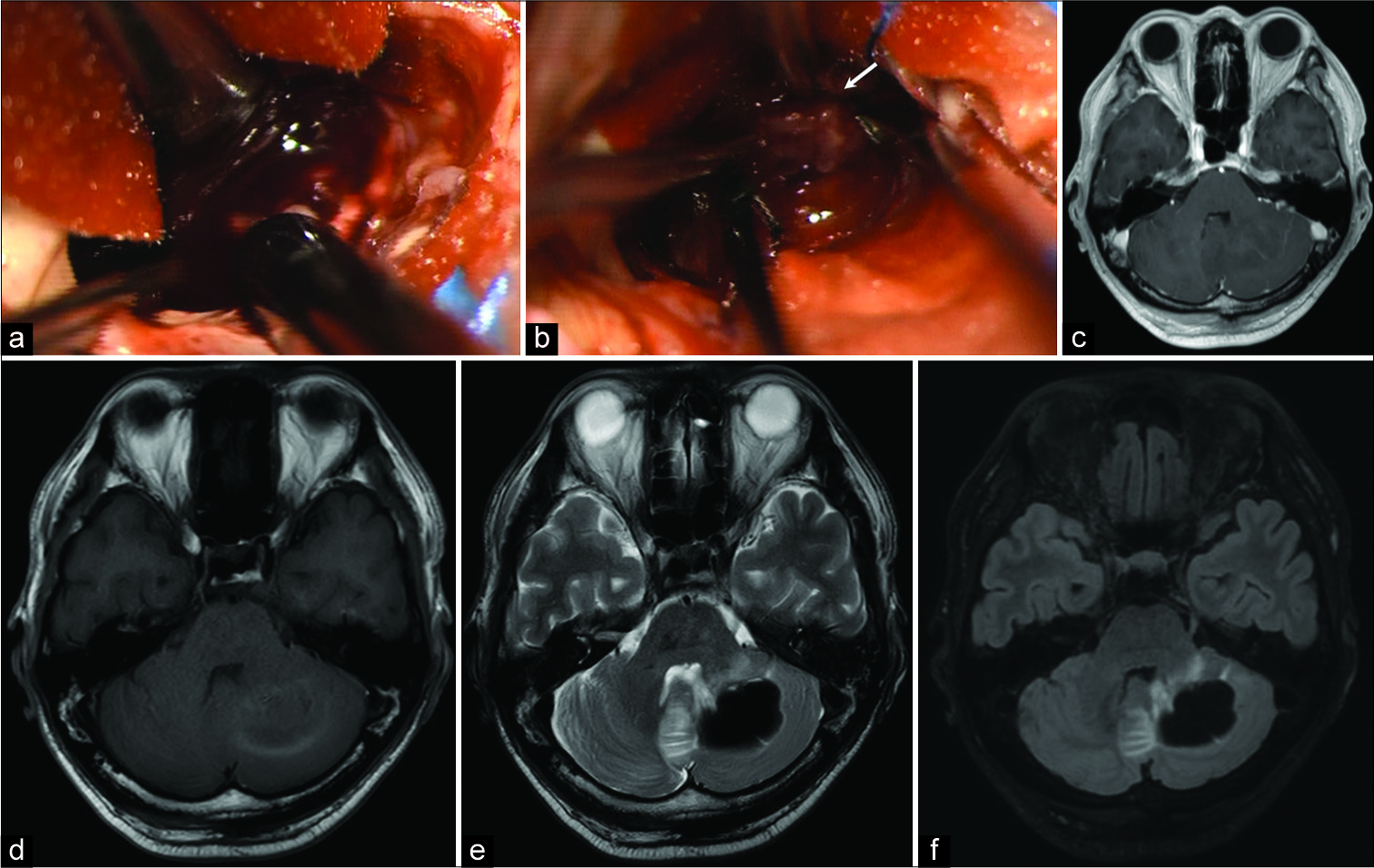
Figure 2:
The contents of the cerebellum cyst were old brownish hematoma-like liquid (a), and partially nodular lesions were inside the cyst (b; arrow). Preoperative magnetic resonance imaging (MRI) of cerebellar metastasis lesion (c: T1WI MRI with contrast, d: T1WI, e: T2WI, f: Fluid-attenuated inversion recovery).
Pathological findings of the primary jejunum tumor were reviewed. The jejunum tumor was poorly differentiated adenocarcinoma resembling cerebellum tumor. Squamous differentiation was limited, observed in part of the tumor. Immunohistochemically, the jejunum tumor cells were positive for cytokeratin (CK) 7, CK8, hepatocyte nuclear factor 4α (HNF4α), vimentin, and p40 (partially positive on cancer cells with squamous differentiation). They were negative for CK20, thyroid transcription factor 1, and caudal- type homeobox protein 2 (CDX2). Next-generation DNA sequencing (NGS) of primary lesions showed a KRAS codon 12 mutation, which is the most frequent genetic alteration of SBA. Based on surgical, radiological, pathological, and genetic findings, this brain tumor was comprehensively diagnosed as a metastasis from poorly differentiated SBA.
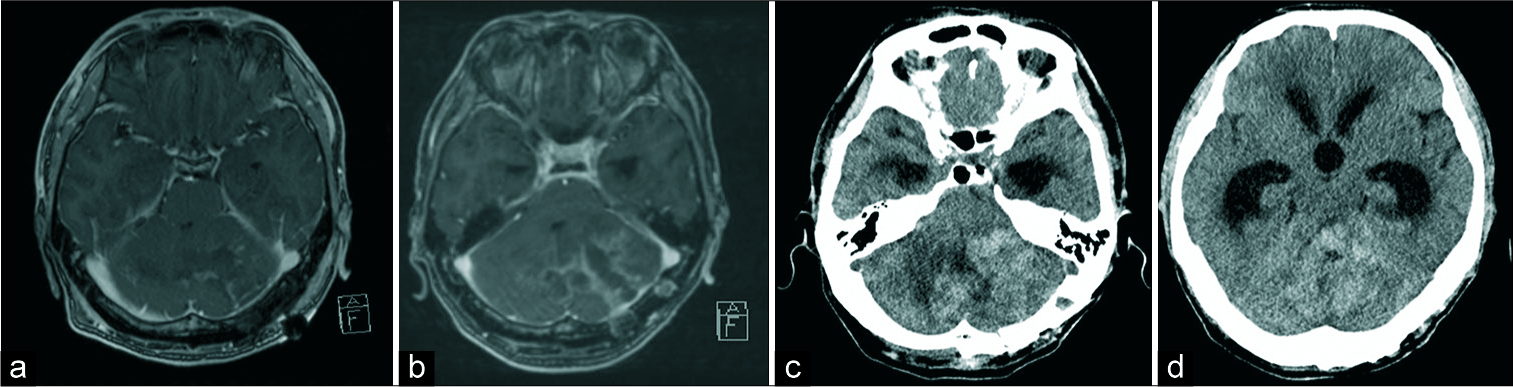
Postoperative MRI revealed total removal of the tumor; thus, according to the results of the JCOG 0504 trial, we chose close observation without additional radiotherapy [
The next day, he was urgently admitted due to bowel obstruction and melena. A CT scan showed the progression of multiple peritoneal metastases. A month later, periodical MRI revealed obstructive hydrocephalus accompanying the recurrence of brain tumor [
DISCUSSION
The breakdown of small bowel malignancies in the United States is 37.4% neuroendocrine tumor, 36.9% adenocarcinomas, 8.4% stromal tumors, and 17.3% lymphomas.[
Immunohistochemically, the jejunum tumor was HNF4α positive and CDX2 negative. HNF4α is consistent with poorly differentiated adenocarcinoma of the gastrointestinal tract. CDX2 is usually positive in differentiated SBA, but in undifferentiated types, the positive rate drops to 58%. Thus, this finding might not be contradictory to the standard immunohistochemistry of poorly differentiated SBA.[
In NGS of the primary lesion, a KRAS codon 12 mutation was detected. It was reported that the mutation of the KRAS gene was frequently observed in SBA, occurring in 43–53% of cases.[
This patient died of intratumoral bleeding from a recurrent tumor, which grew rapidly 1 month after surgery. Considering the initial brain metastasis had intratumoral bleeding, postoperative adjuvant radiotherapy might have avoided it.
CONCLUSION
Here, we experienced a very rare case of brain metastasis from poorly differentiated SBA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bilimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, Talamonti MS. Small bowel cancer in the United States: Changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg. 2009. 249: 63-71
2. Dabaja BS, Suki D, Pro B, Bonnen M, Ajani J. Adenocarcinoma of the small bowel: Presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004. 101: 518-26
3. Halfdanarson TR, McWilliams RR, Donohue JH, Quevedo JF. A single-institution experience with 491 cases of small bowel adenocarcinoma. Am J Surg. 2010. 199: 797-803
4. Kayama T, Sato S, Sakurada K, Mizusawa J, Nishikawa R, Narita Y. Effects of surgery with salvage stereotactic radiosurgery versus surgery with whole-brain radiation therapy in patients with one to four brain metastases (JCOG0504): A phase III, noninferiority, randomized controlled trial. J Clin Oncol. 2018. 36: JCO2018786186-
5. Khrolenko DE, Belaia KA. On metastases to the brain by cancer originating in the small intestine. Zh Nevropatol Psikhiatr Im S S Korsakova. 1967. 67: 655-8
6. Laforest A, Aparicio T, Zaanan A, Silva FP, Didelot A, Desbeaux A. ERBB2 gene as a potential therapeutic target in small bowel adenocarcinoma. Eur J Cancer. 2014. 50: 1740-6
7. Masselli G, Colaiacomo MC, Marcelli G, Bertini L, Casciani E, Laghi F. MRI of the small-bowel: How to differentiate primary neoplasms and mimickers. Br J Radiol. 2012. 85: 824-37
8. Overman MJ, Pozadzides J, Kopetz S, Wen S, Abbruzzese JL, Wolff RA. Immunophenotype and molecular characterisation of adenocarcinoma of the small intestine. Br J Cancer. 2010. 102: 144-50
9. Salvati M, Cervoni L, Paolini S, Delfini R. Solitary cerebral metastases from intestinal carcinoma. Acta Neurochir (Wien). 1995. 133: 181-3
10. Schottenfeld D, Beebe-Dimmer JL, Vigneau FD. The epidemiology and pathogenesis of neoplasia in the small intestine. Ann Epidemiol. 2009. 19: 58-69
11. Schrock AB, Devoe CE, McWilliams R, Sun J, Aparicio T, Stephens PJ. Genomic profiling of small-bowel adenocarcinoma. JAMA Oncol. 2017. 3: 1546-53






youssef
Posted January 31, 2020, 11:28 am
Good morning.
I read your article with interest, my wife had the exactly the same case, with SBA in the jujenum, and synchrouns liver metastasis.
she takes complete surgery of small bowel, and after, liver surgery, and after, brain metastasis which we treat by sterotaxic radiotherapy Gamma Knife. she lived 15 months after the detection of this brain metastasis. that happens between february 2015 and april 2017. and she was treated at the French Hospital Salpetriere.
I you want, I can discuss with you our strategy, and communicate you any information , in order to help other, and take benefice from our experience.
Best regards
my name is youssef,