- Department of Neurosurgery, American University of Beirut Medical Center, Beirut,
- School of Medicine, University of Balamand, El-Koura, Lebanon.
Correspondence Address:
Marwan Najjar, Department of Neurosurgery, American University of Beirut Medical Center, Beirut, Lebanon.
DOI:10.25259/SNI_698_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sarah Kawtharani1, Charbel Moussalem1, Mohamad El Houshiemy1, Elias Horanieh2, Marwan Najjar1. A rare case of metastatic colon cancer to the pineal region: A case report. 30-Sep-2022;13:453
How to cite this URL: Sarah Kawtharani1, Charbel Moussalem1, Mohamad El Houshiemy1, Elias Horanieh2, Marwan Najjar1. A rare case of metastatic colon cancer to the pineal region: A case report. 30-Sep-2022;13:453. Available from: https://surgicalneurologyint.com/surgicalint-articles/11896/
Abstract
Background: Colorectal cancer is the third most common cancer and the third most leading cause of death in the United States with brain being a rare site for metastasis and the pineal region being a rarer site to manifest.
Case Description: We present a rare case of a 72-year-old male patient with pineal region tumor and obstructive hydrocephalus for which an endoscopic third ventriculostomy was done with biopsy of the tumor showing primary colorectal origin in a patient known to be previously healthy.
Conclusion: Intracranial metastasis to the pineal region is considered rare especially in cases without widely spread systematic cancer or without presence of other metastatic lesions in the brain. The case we presented suggests that we should consider pineal region metastasis as part of our differential whenever we encounter patients with an isolated pineal lesion. Endoscopic third ventriculostomy can be a better treatment option to treat obstructive hydrocephalus caused by the lesion potentially avoiding peritoneal dissemination.
Keywords: Colon cancer, Endoscopic third ventriculostomy, Pineal lesion, Pineal region metastasis
INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer and the third most leading cause of death in the United State.[
CASE PRESENTATION
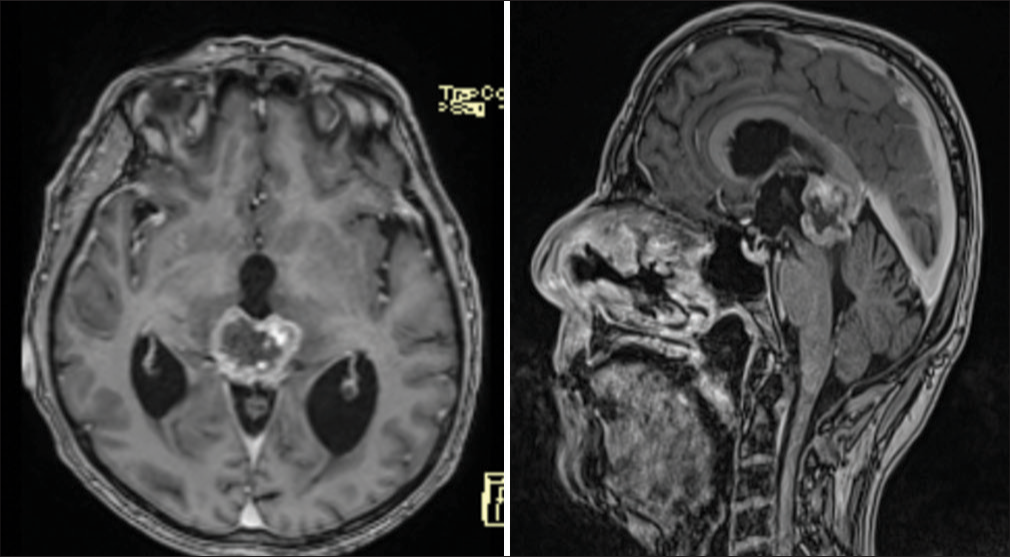
We present the case of a 72-year-old male patient who is known to have coronary artery disease on aspirin and who presented to our institution with 2-month history of horizontal, binocular diplopia, with the left-sided numbness of his face, gait instability, tinnitus, and vertigo. He denied previous history of headaches, seizure activity, memory deficits, or urinary incontinence. His physical examination was intact with no neurological deficits. MRI brain done as part of the work up showed a 2.8 cm tumor with its epicenter in the pineal gland region which invades the medial aspects of the thalami bilaterally, the tectum inferiorly, and the anteroinferior aspect of the splenium of the corpus callosum superiorly [
The patient underwent a right burr hole for endoscopic third ventriculostomy with endoscopic biopsy of the pineal region tumor.
The pathology result was consistent with a colorectal primary cancer. The tumor cells were positive for CK20 and CDX-2 and negative for CK7 and TTF-1.
DISCUSSION
Colon cancer is known to metastasize to several sites including lymph nodes, liver, lung, peritoneum, and rarely to the brain holding a poor prognosis with best median survival shown to be in patients who receive multimodality treatment.[
CONCLUSION
Intracranial metastasis to the pineal region is considered rare especially in cases without widely spread systematic cancer or without presence of other metastatic lesions in the brain. The case we presented suggests that we should consider pineal metastasis as part of our differential whenever we encounter patients with isolated pineal lesion. Endoscopic third ventriculostomy can be a better treatment option to treat obstructive hydrocephalus caused by the lesion without causing any peritoneal dissemination, especially that a biopsy may be done in the same procedure should that be required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Lassman AB, Bruce JN, Fetell MR. Metastases to the pineal gland. Neurology. 2006. 67: 1303-4
2. Majd N, Simon M, Wagman R, Gesner L. A rare case of colon cancer metastasis to the brain anda brief review of its treatment and prognosis. Radiol Case Rep. 2022. 17: 696-9
3. Mege D, Ouaissi M, Fuks D, Metellus P, Peltier J, Dufour H. Patients with brain metastases from colorectal cancer are not condemned. Anticancer Res. 2013. 33: 5645-8
4. Mongan JP, Fadul CE, Cole BF, Zaki BI, Suriawinata AA, Ripple GH. Brain metastases from colorectal cancer: Risk factors, incidence, and the possible role of chemokines. Clin Colorectal Cancer. 2009. 8: 100-5
5. Nemoto K, Aoshiba K, Itoh M, Semba S, Tsuji T, Adachi H. Isolated pineal region metastasis from lung adenocarcinoma with obstructive hydrocephalus: A case report. J Med Case Rep. 2013. 7: 71
6. Struja T, Capraro J. Synchronous pituitary and pineal gland lesions presenting with panhypopituitarism in a patient with widespread colorectal cancer: A case report. Oxf Med Case Rep. 2021. 2021: omab030