- Department of Neurosurgery, Military Hospital of Instruction of Tunis, Tunis, Tunisia.
- Department of Pathology, Military Hospital of Instruction of Tunis, Tunis, Tunisia.
Correspondence Address:
Kaouther Somrani, Department of Neurosurgery, Military Hospital of Instruction of Tunis, Tunis, Tunisia.
DOI:10.25259/SNI_1115_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kaouther Somrani1, Hichem Ammar1, Faten Gargouri2, Nada Mansouri2, Mohamed Dehmani Yedeas1, Ridha Chkili1. A rare case report of sacral epidural angiolipoma: Diagnosis and treatment. 04-Feb-2022;13:38
How to cite this URL: Kaouther Somrani1, Hichem Ammar1, Faten Gargouri2, Nada Mansouri2, Mohamed Dehmani Yedeas1, Ridha Chkili1. A rare case report of sacral epidural angiolipoma: Diagnosis and treatment. 04-Feb-2022;13:38. Available from: https://surgicalneurologyint.com/surgicalint-articles/11368/
Abstract
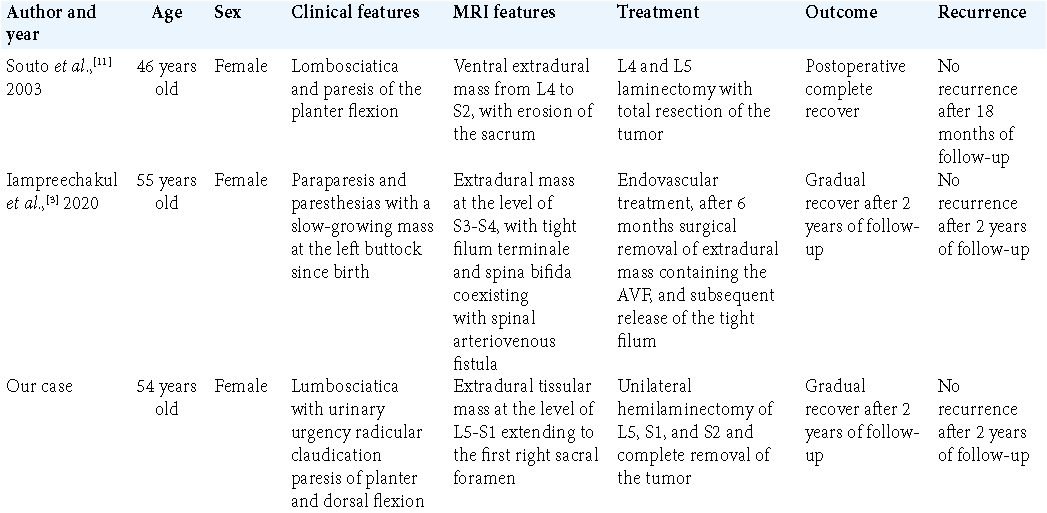
Background: Spinal angiolipomas are rare benign tumors composed of mature adipose tissue and anomalous vascular channels. The sacral localization is extremely rare. To the best of our knowledge, there have been only two cases reported in the literature. Herein, we present an additional case of sacral angiolipoma.
Case Description: We present a case of a 54-year-old woman who presented with the right lumbosciatica and distal crural weakness. Spinal MRI showed an epidural lesion at the level of L5-S1 extending to the first right sacral foramen. The patient had total resection of the tumor and the histological study concluded to an angiolipoma. The patients’ neurologic symptoms improved postoperatively and follow-up revealed no signs of tumor recurrence.
Conclusion: Despite the rarity of sacral localization in angiolipomas, it is a diagnosis to be considered in the case of an epidural tumor with foraminal extension. Magnetic resonance imaging is important for detecting and characterizing spinal angiolipomas despite diagnosis is not always obvious. After surgical removal, the functional prognosis is generally favorable.
Keywords: Benign tumor, Epidural, Sacral, Spinal angiolipoma, Surgery
INTRODUCTION
Spinal angiolipomas are benign neoplasm composed of mature lipocytes and abnormal blood vessels. They account for only 0.04–1.2% of all spinal tumors and are predominantly found in the epidural space, where they represent 2–3% of spinal tumors.[
CASE REPORT
This is a 54-year-old woman with no medical history who was referred to our department by family physician for progressively worsening of the right lumbosciatica associated with urinary urgency for 2 years and radicular claudication for 1 year, reducing the walking perimeter to 500 m.
On examination, she had paresis of plantar and dorsal flexion (muscle strength 2/5) associated with a poorly systematized hypoesthesia of the right lower limb. She did not have saddle anesthesia. Spinal magnetic resonance imaging (MRI) showed an epidural tissular mass at the level of L5-S1 extending to the first right sacral foramen, which was enlarged without bone lysis with extension to the presacral soft tissues, hypointense on T1-weighted image, slightly hyperintense on T2-weighted image with intense and homogeneous contrast. This lesion was suggestive of an S1 schwannoma [
Figure 1:
Magnetic resonance imaging of the lumbosacral spine: sagittal gadolinium T1-weighted with fat suppression (a), T2-weighted (b), axial T2-weighted (c), and coronal T2-weighted (d) demonstrated intracanal tissular process regarding L5-S1 extending to the level of the first right sacral foramen, which was enlarged without bone lysis with extension to the presacral soft tissues, in T1 hyposignal, moderate T2 hypersignal with intense and homogeneous contrast.
The patient was operated in the genupectoral position. A median incision from L4 to S3 was performed followed by a right unilateral approach and hemilaminectomy of L5, S1, and S2 until exposure of the S3 foramen. A reddish hemorrhagic epidural lesion was found, pushing back the dural sac and the right S2 nerve. A careful dissection of the tumor was performed following a cleavage plane with the nerve. The resection was macroscopically complete.
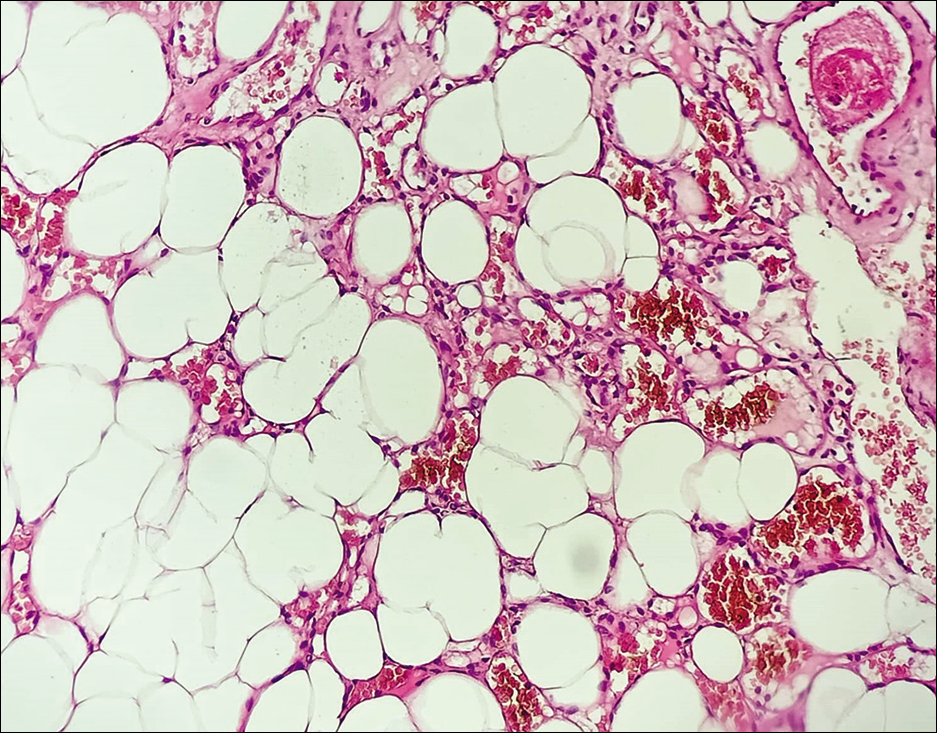
The histological study concluded to an angiolipoma [
Postoperatively, the patient showed an improvement of her motor deficit, which was rated at 3+/5, and she underwent motor rehabilitation, which allowed her to walk normally again.
A 2-year follow-up revealed no signs of tumor recurrence.
DISCUSSION
In the review of Preul et al.,[
The majority of spinal angiolipomas arise in women throughout their peri- or postmenopausal period. According to a literature review of 108 spinal angiolipomas in 2009, the majority of the tumors (86%) were located in the thoracic spine, followed by 12 (11%) in the lumbar spine, 2 (1.85%) in the cervical spine, and one in the sacrum.[
Spinal angiolipoma usually presents as a slow-growing mass causing compression of the spinal cord. Clinically, early symptoms are typically numbness in the lower extremities, back discomfort, and leg weakness,[
Angiolipomas are mesenchymal neoplasms made up of mature adipose tissue and aberrant blood arteries. These lesions are considered a subgroup of lipomas.[
In some aspects, spinal angiolipomas differ from spinal lipomas. The former is more common in adults, almost always seen in the epidural space, and is unrelated to congenital myelovertebral abnormalities. The latter mainly appears in childhood and is found in the epi- and intra-dural regions; majority are associated to congenital myelovertebral abnormalities.[
Noninfiltrating and infiltrating angiolipomas are the two forms of spinal angiolipomas. The majority of these tumors, including our case, are noninfiltrating.[
Extradural components of angiolipomas are isointense or hyperintense in T1-weighted images, most likely due to the fat component, and usually hyperintense in T2-weighted images in MRI studies. These areas show an early enhancement following gadolinium administration and are thought to be the vascular component.[
Surgical resection of the lesion through anterior approach or posterior laminectomy is the gold standard treatment modality.[
The first-choice treatment is total surgical removal of the tumor. However, it may be more difficult in the infiltrating type than in the noninfiltrating type. Nevertheless, even with partial removal, most patients have a good prognosis because tumors are usually slow growing and do not progress to malignancy.[
CONCLUSION
Spinal angiolipomas are rare benign tumors of angiomatous and lipomatous tissue. Sacral location is exceptional. The diagnosis can be challenging radiologically since they may mimic the other spinal lesions. Total resection may not be achievable in some cases. We attained total resection in our case without any further neurological complication.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Gelabert-González M, García-Allut A. Spinal extradural angiolipoma: Report of two cases and review of the literature. Eur Spine J. 2009. 18: 324-35
2. Guzey FK, Bas NS, Ozkan N, Karabulut C, Bas SC, Turgut H. Lumbar extradural infiltrating angiolipoma: A case report and review of 17 previously reported cases with infiltrating spinal angiolipomas. Spine J. 2007. 7: 739-44
3. Iampreechakul P, Tangviriyapaiboon T, Liengudom A, Lertbutsayanukul P, Thammachantha S, Siriwimonmas S. Sacral extradural angiolipoma associated with tight filum terminale and spina bifida coexisting with spinal arteriovenous fistula. World Neurosurg. 2020. 140: 37-45
4. Labram EK, El-Shunnar K, Hilton DA, Robertson NJ. Revisited: Spinal angiolipoma-three additional cases. Br J Neurosurg. 1999. 13: 25-9
5. Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974. 34: 720-7
6. Oge HK, Söylemezoglu F, Rousan N, Ozcan OE. Spinal angiolipoma: Case report and review of literature. J Spinal Disord. 1999. 12: 353-6
7. Pearson J, Stellar S, Feigin I. Angiomyolipoma: Long-term cure following radical approach to malignant-appearing benign intraspinal tumor: Report of three cases. J Neurosurg. 1970. 33: 466-70
8. Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas: Report of three cases. J Neurosurg. 1993. 78: 280-6
9. Rocchi G, Caroli E, Frati A, Cimatti M, Savlati M. Lumbar spinal angiolipomas: Report of two cases and review of the literature. Spinal Cord. 2004. 42: 313-6
10. Sakaida H, Waga S, Kojima T, Kubo Y, Matsubara T, Yamamoto J. Thoracic spinal angiomyolipoma with extracanal extension to the thoracic cavity: A case report. Spine (Phila Pa 1976). 1998. 23: 391-4
11. do Souto AA, Domingues FS, Chimelli L, Lemos AM. Lumbosacral angiolipoma: Case report. Arq Neuropsiquiatr. 2003. 61: 269-73
12. Trabulo A, Cerqueira L, Monteiro J, Roque P, Reis FC, Coelho MR. Spinal angiolipomas revisited: Two case reports. Acta Neurochir (Wien). 1996. 138: 1311-9
13. Yang X, Richard SA, Lei C, Liu J, Huang S. Spinal extradural angiolipoma: A report of two cases and review of literature. J Spine Surg. 2018. 4: 490-5