- Department of Neurosurgery, Centro Hospitalar Universitario do Algarve, Rua Leao Penedo, Faro, Portugal.
DOI:10.25259/SNI_161_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Pedro Teles, Joaquim Pedro Correia, Lia Pappamikail, Artur Lourenço, Clara Romero, Fátima Lopes, Gonçalo Neto Almeida, Pedro Abreu. A spontaneous cervical epidural hematoma mimicking a stroke – A case report. 20-Jun-2020;11:157
How to cite this URL: Pedro Teles, Joaquim Pedro Correia, Lia Pappamikail, Artur Lourenço, Clara Romero, Fátima Lopes, Gonçalo Neto Almeida, Pedro Abreu. A spontaneous cervical epidural hematoma mimicking a stroke – A case report. 20-Jun-2020;11:157. Available from: https://surgicalneurologyint.com/surgicalint-articles/10093/
Abstract
Background: A spontaneous cervical epidural hematoma (SCEH) is a rare occurrence. It usually presents with quadriparesis, but it may present with hemiparesis or hemiplegia and can easily be misdiagnosed as stroke. We present a case of stroke mimicking SCEH with hemiparesis worsened after tissue plasminogen activator therapy (tPA) followed by emergency cervical decompression laminectomy.
Case Description: A 63-year-old female presented to the emergency department with sudden onset of posterior neck and left shoulder pain with the right side hemiparesis. On neurological examination, the patient had motor power of the right upper and lower limb of 2/5 Medical Research Council, and her whole left extremities were intact. Her medical history was unremarkable for trauma, hemorrhagic diathesis, or anticoagulation therapy. A head computed tomography was ordered ruling out intracranial hemorrhage. Assuming an acute ischemic stroke as the most likely diagnosis, alteplase (tPA) was administered 3 h after symptoms onset, however without any improvement in patient symptoms. A cervical magnetic resonance was performed revealing a right paramedian epidural mass-like lesion between C3-C6. The patient underwent cervical laminectomy C3-C6 with evacuation of epidural hematoma with significant clinical status improvement after surgery.
Conclusion: tPA treatment is frequently used as first-line therapy for acute ischemic stroke. Therefore, physicians should be aware of the potential for the SCEH in patients presenting with hemiparesis, as tPA administration may increase cervical hematoma leading to clinical deterioration. With this case, we intended to warn about SCEH as a rare but possible entity, since its early recognition and prompt clinical intervention may improve neurological outcomes.
Keywords: Cervical epidural hematoma, Stroke, Thrombolysis
INTRODUCTION
A spontaneous cervical epidural hematoma (SCHE) is a rare condition with an estimated incidence of 0.1/100,000.[
The classical clinical presentation is acute neck or interscapular pain, and as a result of the spinal cord compression sensory and motor loss may be seen, such as paraparesis, quadriparesis, or Brown-Sequard syndrome.[
We describe a case of SCHE mimicking a stroke where treatment with alteplase (tPA) was considered as first-line treatment followed by emergency laminectomy.
CASE DESCRIPTION
A 63-year-old female presented to the emergency department with sudden onset of posterior neck and left shoulder pain with right side hemiparesis, mimicking a stroke.
She reported taking hydrochlorothiazide and atenolol for hypertension and her medical history was otherwise unremarkable without known hemorrhagic diathesis, anticoagulation therapy, or recent trauma. Neurological examination revealed right side hemiparesis with 2/5 Medical Research Council (MRC) in the upper limb and 0/5 in the lower limb, sensory function was preserved bilaterally, and all other findings were within normal limits.
A head computed tomography (CT) was ordered which ruled out intracranial hemorrhage. Assuming an acute ischemic stroke as the most likely diagnosis at the time (NIHSS 8), tPA was administered 3 h after symptoms onset, however without any improvement in patient symptoms.
During the first 48 h, her neurological examination remained the same, after which she developed worsening of clinical symptoms with progressive posterior neck and left shoulder pain associated with decreased sensation to pinprick and light touch in the right lower limb.
A cervical magnetic resonance image (MRI) was performed revealing a right paramedian epidural mass-like lesion between C3-C6 [
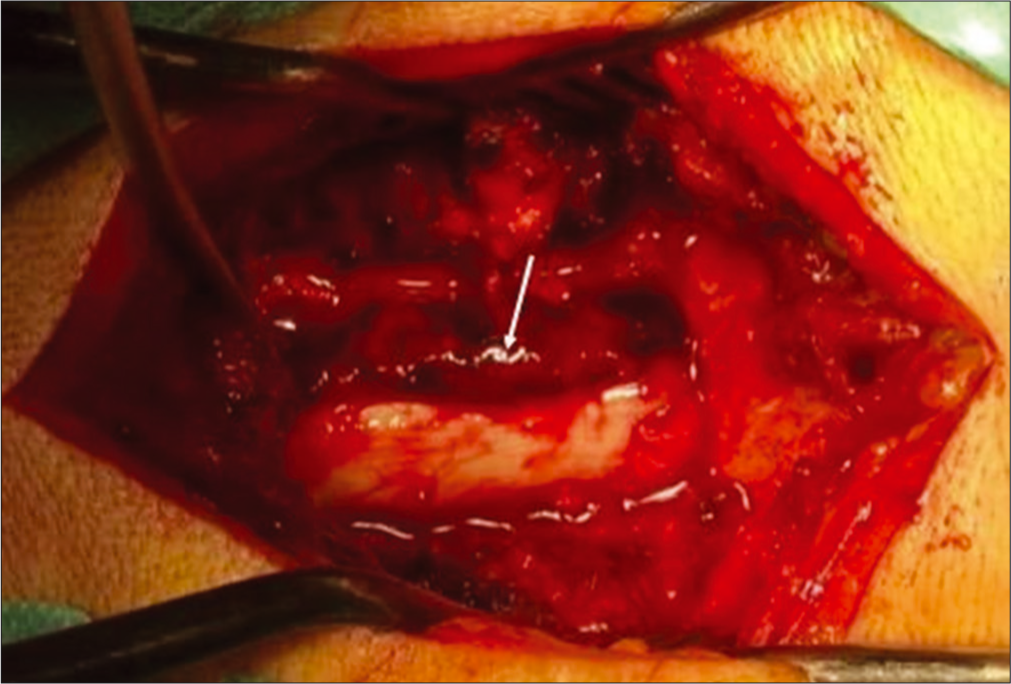
Seventy-two hours after onset the patient underwent cervical laminectomy C3-C6 with evacuation of epidural hematoma [
The patient clinical status suffered no significant improvement immediately after surgery, maintaining right side hemiparesis. During the hospital stay, she enrolled in a strict neurological rehabilitation program and presented motor strength of 3/5 MRC in the right upper limb and 1/5 MRC in the right lower limb at the time she was repatriated back home.
DISCUSSION
SCHE is considered a surgical emergency and was first described by Jackson in 1869.[
Even though there is still some debate if the hematoma mechanism originates in an arterial or venous bleeding point, some risk factors have been established including coagulopathy, vascular malformation, tumors, hypertension, as well as anti-coagulation therapy and Paget’s disease.[
Neurological examination and clinical findings are of paramount importance to avoid misdiagnosis; however, imaging studies are still necessary for a definitive diagnosis. The most common symptoms are sudden neck or back pain followed by motor or sensory deficit caused by compression of the spinal cord and nerve roots.[
CT is the first-line diagnostic tool to exclude cerebral hemorrhage, in patients where ischemic stroke is suspected, and intravenous thrombolytic treatment is considered. Although not necessary to identify ischemic lesions, MRI is more sensitive than CT, showing early signals of cerebral infarction in diffusion-weighted images.[
During the first 24 h, SCHE is shown isointense in T1-weighted images and mildly hyperintense in T2-weighted images, after 72 h due to the hemoglobin oxygenation status and cellular lysis usually appears hyperintense in T1 and hypointense in T2, which correlates with the findings in our case.[
Although tPA is an effective first-line treatment for acute ischemic stroke, it has been established a correlation between its use and spinal hematoma, with potential risk for hematoma progression and worsening of symptoms.
The absence of clinical improvement after tPA administration should prompt further investigation as lack of improvement at 24 h is an independent predictor of poor outcome. Early MRI, when available, should be obtained to exclude extension of the original infraction, lacunar infarction, brain edema, or hydrocephalus and to rule out complications such as intracranial hemorrhage. In this case, an MRI scan was obtained at 48 h after worsening of clinical symptoms. This may have caused a delay in the diagnosis, leading to late surgery and therefor limiting potentially recovery.
Emergency decompression laminectomy with hematoma evacuation represents the most effective treatment for SCHE, however conservative treatment may be an option in patients without neurological involvement or with strong surgical contraindication.[
In this case, surgery was performed 72 h after symptom onset, which is beyond optimal time, fact that could explain the lack of significant neurological improvement. This emphasizes the need for early diagnosis to reduce the time elapsed between symptom onset and surgical decompression and maximize potential neurological recovery.
CONCLUSION
tPA treatment is frequently used as first-line therapy for acute ischemic stroke. Therefore, physicians should be aware of the potential for the SCEH in patients presenting with hemiparesis, as tPA administration may increase cervical hematoma leading to clinical deterioration. With this case, the authors intended to warn about SCEH as a rare but possible entity, since its early recognition and prompt clinical intervention may improve neurological outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adamson D, Bulsara K, Bronec P. Spontaneous cervical epidural hematoma: Case report and literature review. Surg Neurol. 2004. 62: 156-9
2. Beatty M, Winston R. Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg. 1984. 61: 143-8
3. Cai HX, Liu C, Zhang JF, Wan S, Uchida K, Fan S. Spontaneous epidural hematoma of thoracic spine presenting as brown-sequard syndrome: Report of a case with review of the literature. J Spinal Cord Med. 2011. 34: 432-6
4. Chalela J, Kidwell C, Nentwich L, Luby M, Butman J, Demchuk A. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: A prospective comparison. Lancet. 2007. 369: 293-8
5. Groen R, Ponssen H. The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci. 1990. 98: 121-38
6. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008. 359: 1317-29
7. Holtas S, Heiling M, Lonntoft M. Spontaneous spinal epidural hematoma: Findings at MR imaging and clinical correlation. Radiology. 1996. 199: 409-13
8. Horcajadas A, Katati M, Arráez MA, Ros B, Abdullah O, Castañeda M. Spontaneous epidural spinal hematoma: Report of 2 cases and review of the literature. Neurologia. 1998. 13: 401-4
9. Hsieh CF, Lin HJ, Chen KT, Foo NP, Te A. Acute spontaneous cervical spinal epidural hematoma with hemiparesis as the initial presentation. Eur J Emerg Med. 2006. 13: 36-8
10. Jackson R. Case of spinal apoplexy. Lancet. 1869. 2: 5-6
11. Lo CC, Chen JY, Lo YK, Lai PH, Lin YT. Spontaneous spinal epidural hematoma: A case report and review of the literatures. Acta Neurol Taiwan. 2012. 21: 31-4
12. Serizawa Y, Ohshiro K, Tanaka K, Tamaki S, Matsuura K, Uchihara T. Spontaneous resolution of an acute spontaneous spinal epidural hematoma without neurological deficits. Intern Med. 1995. 34: 992-4
13. Shin JJ, Kuh SU, Cho YE. Surgical management of spontaneous spinal epidural hematoma. Eur Spine J. 2006. 15: 998-1004
14. Tiryaki M, Basaran R, Aydin SO, Efendioglu M, Balkuv E, Balak N. Spontaneous cervical epidural hematoma with hemiparesis mimicking cerebral stroke. Case Rep Emerg Med. 2014. 2014: 210146-
15. Wang CC, Chang CH, Lin HJ, Lin KC, Kuo JR. Misdiagnosis of spontaneous cervical epidural haemorrhage. Eur Spine J. 2009. 18: 210-2