- Department of Neurosurgery, Kumamoto City Hospital, Kumamoto, Japan
- Department of Neurosurgery, Kumamoto Red Cross Hospital, Kumamoto, Japan
- Department of Pathology, Kumamoto Red Cross Hospital, Kumamoto, Japan
- Department of Neurosurgery, Kumamoto University, Kumamoto, Japan
Correspondence Address:
Yushin Takemoto
Department of Neurosurgery, Kumamoto University, Kumamoto, Japan
DOI:10.4103/2152-7806.179586
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takemoto Y, Hasegawa S, Nagamine M, Kasamo D, Matsumoto J, Miura M, Kuratsu J. A spontaneous superficial temporal artery pseudoaneurysm possibly related to atherosclerosis: Case report and review of literature. Surg Neurol Int 01-Apr-2016;7:
How to cite this URL: Takemoto Y, Hasegawa S, Nagamine M, Kasamo D, Matsumoto J, Miura M, Kuratsu J. A spontaneous superficial temporal artery pseudoaneurysm possibly related to atherosclerosis: Case report and review of literature. Surg Neurol Int 01-Apr-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-spontaneous-superficial-temporal-artery-pseudoaneurysm-possibly-related-to-atherosclerosis-case-report-and-review-of-literature/
Abstract
Background:Spontaneous superficial temporal artery (STA) pseudoaneurysms are very rare; only four cases, including ours, have been reported to date. Therefore, the cause of them has not been studied.
Case Description:A 57-year-old woman was admitted to our hospital with a pulsatile mass in the left preauricular region. Her medical history included hypertension, dyslipidemia, and angina pectoris. She denied a history of head injury or minor head trauma. Three-dimensional computed tomography angiography showed a well-enhanced saccular aneurysm on the main trunk of the STA. To prevent rupture it was removed surgically. The histological diagnosis was pseudoaneurysm with atherosclerosis. By the 2nd postoperative day, she had completely recovered and was discharged home. There has been no relapse.
Conclusions:As all four documented patients were at high risk for atherosclerosis, we posit that a causal factor was weakening of the arterial wall due to atherosclerosis and chronic pressure on the STA from anatomical structures. Here, we present histological evidence to support this hypothesis.
Keywords: Pseudoaneurysm, spontaneous, superficial temporal artery
INTRODUCTION
The first case report of a superficial temporal artery (STA) aneurysm was published in 1740; subsequently, about 400 additional cases have been reported.[
CASE REPORT
Presentation and clinical evaluation
This 57-year-old woman was referred to our hospital with a growing pulsatile mass in the left preauricular region. She had first noticed the gradually growing mass 5 years earlier. Her medical history included hypertension (HT), dyslipidemia (DL), and angina pectoris. She was treated with oral calcium- and angiotensin II receptor blockers. She had no recollection of head injury or minor head trauma.
Physical examination disclosed no neurological deficits. There was a 13 mm × 10 mm pulsatile mass in the left preauricular region; it was painless but annoying. Three-dimensional computed tomography angiography showed a well-enhancing saccular aneurysm on the main trunk of the STA [
We were instructed her to manually compress the pseudoaneurysm (press a finger on the skin over the pulsatile area) for 30 min 3 times a day. However, it did not thrombosed. To prevent aneurysmal rupture we performed the surgical removal.
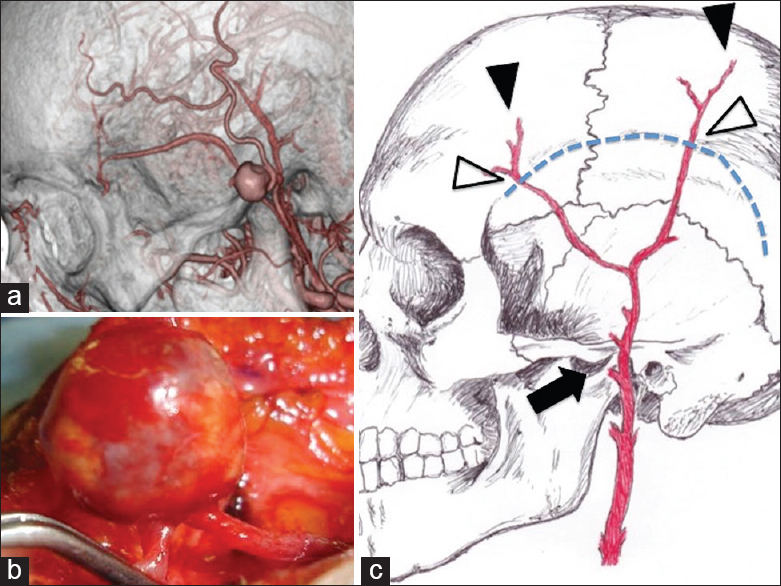
Figure 1
Pre- and intra-operative superficial temporal artery aneurysm imaging and figure. (a) Three-dimensional computed tomography angiogram showing an aneurysm on the main trunk of the superficial temporal artery and the preauricular region on the zygomatic arch. (b) Intraoperative photograph showing the superficial temporal artery aneurysm. There is a small distance between the feeding and the draining artery. (c) Lateral view of the cranial and superficial temporal artery schema showing that the main trunk of the superficial temporal artery crosses the zygomatic arch in the preauricular region, the site where the spontaneous superficial temporal artery pseudoaneurysm developed (arrow). The superficial temporal artery passes over the linea temporalis (white arrowhead) and includes its tip (black arrowhead)
Surgery
With the patient under general anesthesia, we made a skin incision about 4 cm above the main trunk of the left STA. The aneurysm was saccular and located lateral to the zygomatic arch. There was a small distance between the feeding and draining vessels [
Pathology
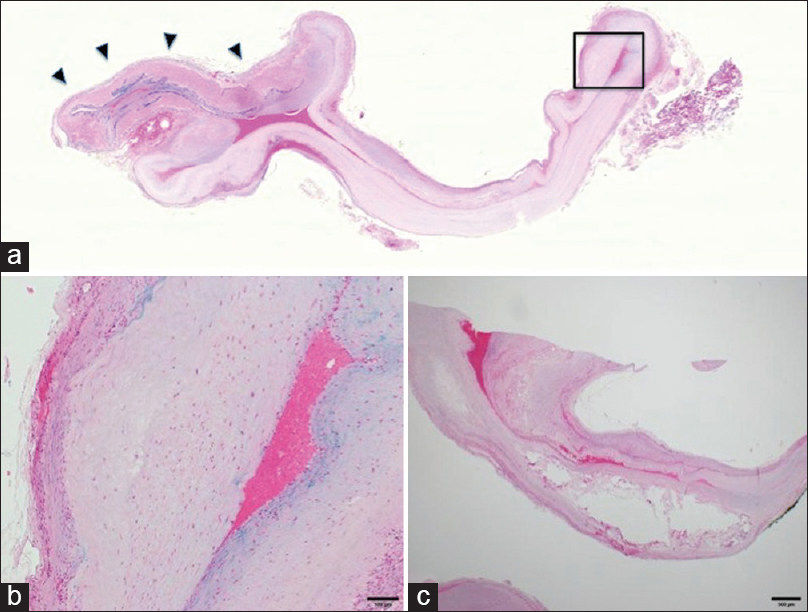
Several histologic sections were prepared from the surgically resected specimen. A cross-section of the aneurysm [
Figure 2
Histological features. (a) Low magnification of the lesion showing saccular dilation of the artery. The remnant of the internal elastic lamina is seen on the left (arrowheads). Victoria blue - H and E staining. (b) High magnification of the aneurysmal wall (encased by a rectangle in
Postoperative course
The patient was discharged home on the 2nd postoperative day. Her condition continues to be good and at the last follow-up 12 months after the operation, there was no evidence of recurrence.
DISCUSSION
Although no universally accepted classification of STA aneurysms based on their etiology has been established, they have been classified as traumatic, iatrogenic, and spontaneous.[
Traumatic aneurysms include those that arise following blunt head trauma, vehicular accidents, stab and gunshot wounds, and sports-related injuries,[
Histologically, most traumatic STA aneurysms exhibit the features of pseudoaneurysms.[
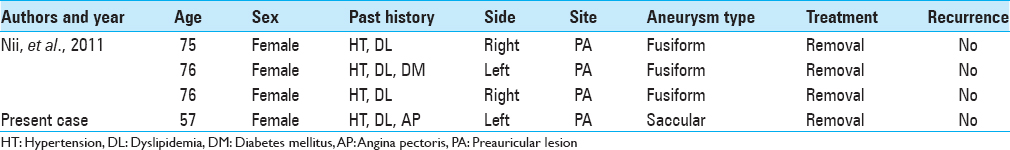
Although Nii et al.[
Most traumatic aneurysms in the head arise on the STA due to its anatomical location.[
They suggested the congenital vulnerability of the arterial wall in this patient population, rather than atherosclerosis, as an important causal factor and the anatomic features of the preauricular region as a contributing factor. From a different perspective, this portion of the STA is not vulnerable to traumatic injury because it runs inside a line from the auricle to the zygomatic arch [
There are two specific sites on the STA that are vulnerable to trauma. One is its peripheral tract; the temporalis muscle is the only protective tissue between the STA and the outer table of the skull. The peripheral portion is particularly vulnerable to injuries due to the lack of protective temporal and frontal muscle tissues [
Other common findings in the four patients with spontaneous STA pseudoaneurysms were their demographics and medical history. All were middle-aged or older women with a history of HT and DL, putting them at high risk for atherosclerosis [
Based on our and previously reported observations in patients with spontaneous STA pseudoaneurysms, we suggest that atherosclerosis, which weakens the arterial wall, and chronic pressure on the STA from anatomical structures, play a role. To support our hypothesis, more case reports and series are needed to identify patient demographics devoid of bias as we cannot rule out the possibility that patients forgot minor trauma to the affected site.
CONCLUSION
To the best of our knowledge, this is the first report of the possible association between atherosclerosis and a spontaneous STA pseudoaneurysm. HT and DL must be treated to prevent cardiovascular events and to prevent spontaneous STA pseudoaneurysms, and physical stress on temporal areas must be avoided, especially in middle-aged and older women with risk factors for atherosclerosis.
Financial support and sponsorship
Nil.
Conflicts of interest
All authors who are members of the Japan Neurosurgical Society (JNS) have registered online self-reported conflict of interest disclosure statement forms through the website for JNS members.
Acknowledgments
I would like to express my sincere gratitude to my supervisor, Prof. Junichi Kuratsu for providing me this precious study opportunity. I especially would like to express my deepest appreciation to my supervisor, Dr. Shu Hasegawa for his elaborated guidance, considerable encouragement, and invaluable discussion that make my research of great achievement and my study life unforgettable.
References
1. Angevine PD, Connolly ES. Pseudoaneurysms of the superficial temporal artery secondary to placement of external ventricular drainage catheters. Surg Neurol. 2002. 58: 258-60
2. Conner WC, Rohrich RJ, Pollock RA. Traumatic aneurysms of the face and temple: A patient report and literature review, 1644 to 1998. Ann Plast Surg. 1998. 41: 321-6
3. Evans CC, Larson MJ, Eichhorn PJ, Taylor RS. Traumatic pseudoaneurysm of the superficial temporal artery: Two cases and review of the literature. J Am Acad Dermatol. 2003. 49: S286-8
4. Fernández-Portales I, Cabezudo JM, Lorenzana L, Gómez L, Porras L, Rodríguez JA. Traumatic aneurysm of the superficial temporal artery as a complication of pin-type head-holder device. Case report. Surg Neurol. 1999. 52: 400-3
5. Fujii S, Kajikawa H, Yamamura K, Wada M, Shimamoto F. Spontaneous dissecting aneurysm of the superficial temporal artery: A case report. No Shinkei Geka. 1995. 23: 797-800
6. Han K, Borah GL. Pseudoaneurysm of the anterior superficial temporal artery. Ann Plast Surg. 1996. 37: 650-3
7. Hong JT, Lee SW, Ihn YK, Son BC, Sung JH, Kim IS. Traumatic pseudoaneurysm of the superficial temporal artery treated by endovascular coil embolization. Surg Neurol. 2006. 66: 86-8
8. Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, Stanley JC. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg. 1991. 13: 452-8
9. Kawabori M, Kuroda S, Nakayama N, Kenmotsu Y, Shimizu H, Tanino M. Spontaneous giant aneurysm of the superficial temporal artery: Case report. Neurol Med Chir (Tokyo). 2009. 49: 198-201
10. Leal FS, Miranda CC, Guimarães AC. Traumatic pseudoaneurysm of the superficial temporal artery: Case report. Arq Neuropsiquiatr. 2005. 63: 859-61
11. Lee HS, Jo KW, Lee SH, Eoh W. Traumatic pseudoaneurysm of the superficial temporal artery due to gardner traction. J Korean Neurosurg Soc. 2010. 48: 291-3
12. Levisianos I, Sood V. Traumatic aneurysm (pseudoaneurysm) of the superficial temporal artery. Emerg Med J. 2008. 25: 239-40
13. Murakami M, Kakita K, Hosokawa Y. Ruptured traumatic aneurysm after trivial injury mimicking acute spontaneous subdural hematoma – Case report. Neurol Med Chir (Tokyo). 2003. 43: 130-3
14. Nii K, Tsutsumi M, Aikawa H, Onizuka M, Sakamoto K, Inoue R. Spontaneous superficial temporal artery pseudoaneurysm in elderly women – Three case reports. Neurol Med Chir (Tokyo). 2011. 51: 713-5
15. Peick AL, Nichols WK, Curtis JJ, Silver D. Aneurysms and pseudoaneurysms of the superficial temporal artery caused by trauma. J Vasc Surg. 1988. 8: 606-10
16. Quereshy FA, Choi S, Buma B. Traumatic pseudoaneurysm of the superficial temporal artery in a pediatric patient: A case report. J Oral Maxillofac Surg. 2008. 66: 133-5
17. Rich NM, Hobson RW, Collins GJ. Traumatic arteriovenous fistulas and false aneurysms: A review of 558 lesions. Surgery. 1975. 78: 817-28
18. Schechter MM, Gutstein RA. Aneurysms and arteriovenous fistulas of the superficial temporal vessels. Radiology. 1970. 97: 549-57
19. Sirin G, Bolcal C, Akay T, Iyem H, Tatar H. Traumatic aneurysm of the superficial temporal artery: A case report. Ulus Travma Acil Cerrahi Derg. 2007. 13: 60-2
20. Skaf GS, Domloj NT, Salameh JA, Atiyeh B. Pseudoaneurysm of the superficial temporal artery: A complication of botulinum toxin injection. Aesthetic Plast Surg. 2012. 36: 982-5
21. Uchida N, Sakuma M. Atherosclerotic superficial temporal artery aneurysm: Report of a case. Surg Today. 1999. 29: 575-8
22. Walker MT, Liu BP, Salehi SA, Badve S, Batjer HH. Superficial temporal artery pseudoaneurysm: Diagnosis and preoperative planning with CT angiography. AJNR Am J Neuroradiol. 2003. 24: 147-50