- Freelance Counsel, Karaarslan Freelance Counsel, Malatya, Istanbul, Turkey.
- Department of Radiology, Republic of Turkey, Ministry of Health, State Hospital, Clinics of Radiology, Istanbul, Turkey.
- Department of Neurosurgery, Namik Kemal University School of Medicine, Tekirdag, Istanbul, Turkey.
- Department of Neurosurgery, Koc University Hospital and Spine Center, Clinics of Neurosurgery, Istanbul, Turkey.
Correspondence Address:
Numan Karaarslan
Department of Neurosurgery, Koc University Hospital and Spine Center, Clinics of Neurosurgery, Istanbul, Turkey.
DOI:10.25259/SNI_703_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulkadir Karaarslan1, Fatma Bahar Hacioğlu Kasim2, Numan Karaarslan3, Ozkan Ates4. A study on legal and medical dimensions of radiation exposure in neurosurgery clinics in Turkish practice. 18-Nov-2020;11:397
How to cite this URL: Abdulkadir Karaarslan1, Fatma Bahar Hacioğlu Kasim2, Numan Karaarslan3, Ozkan Ates4. A study on legal and medical dimensions of radiation exposure in neurosurgery clinics in Turkish practice. 18-Nov-2020;11:397. Available from: https://surgicalneurologyint.com/surgicalint-articles/10400/
Abstract
Background: In the present study, the first aim was to address the detrimental effects of the fluoroscopy procedure performed by physicians and other health-care professionals in neurosurgery clinics, then to examine precautions that should be taken to avoid harmful effects of radiation and radioactive substances during this process. The second aim was to handle the rights provided for health-care professionals exposed to the radiation in workplaces.
Methods: A standardized questionnaire was used for a multicenter survey. Volunteer, intellectual, and cooperative participants (n = 41) were randomly chosen. The survey was prepared considering reports drawn up by the International Atomic Energy Agency. The questions concerning safe and effective fluoroscopy procedure were asked to the participants. The answers received were statistically evaluated. The alpha significance value was accepted as 0.05.
Results: Two neurosurgeons only knew the legal rights that they might possess due to the exposure to the radiation or radioactive substances.
Conclusion: The survey conducted among the health-care professionals revealed the insufficiency of knowledge about the protection from the radiation exposure or radioactive substances in workplaces. Furthermore, both health-care professionals working in radiology clinics, and those in neurosurgery and other clinics who are likely to be exposed to the radiation or radioactive substances have the rights afforded by the law.
Keywords: Constitutional rights, Fluoroscopy, Neurosurgery, Radiation exposure, Rights of employees, X-rays
INTRODUCTION
Recent progress in health-care technology has significantly contributed to the neurosurgery practice. Novel radiological diagnostic methods and the use of devices such as fluoroscopy have enabled to make an accurate and timely diagnosis as well as to facilitate surgical operations. Discography, a novel imaging technique, is commonly performed using modified Dallas Classification for the evaluation of annular tears and extravasations in the intervertebral discs.[
As is well known, fluoroscopy is a radiological technique that allows the real-time visualization of the body parts. To ensure safe fluoroscopy procedure, the significant measures should be taken to avoid the adverse effects of X-rays. In all cases, physicians, technicians, or other staffs should use the device quite carefully by sitting behind a protective compartment and using a variety of protective equipment, especially a lead apron. Even though all the protective measures are taken, and the application protocol is completely complied with, the patients, surgeons, as well as staff involved in the procedure may be exposed to some extent to radioactive substances, such as alpha, beta, or gamma rays.[
It is an obvious fact that the use of these kinds of devices emitting radioactive substance can markedly cause biological damages to the living creatures depending on the dose administered, the administration pace, the type/energy of the administered radiation, the distribution of the dose in the tissues, and the sensitivity of the tissues to radioactive materials.[
The mentioned damages occur due to the apoptosis, death, and proliferation of the cells. Thus, deterministic effects such as cataracts, skin burns, infertility, and death,[
Right to work which constitutes the legal basis of the issue is set forth in articles 48–52 of the Turkish Constitution.[
In Turkish practice, health-care professionals who are more likely to be exposed to the radioactive substances in workplaces can work maximum 35 h/week. Moreover, they benefit from an extra-annual paid leave and a length of the service pay increase. They possess the right of 1-month additional paid leave per year, along with their 1-month legal paid leave. In addition, their social insurance contribution is legally increased; therefore, they have the right to early retirement.
The Turkish Atomic Energy Authority is a legal entity authorized by law for carrying out various training activities, auditing, and studies and for drawing up regulations concerning radiation protection, safety, and security of nuclear installations, nuclear materials, and radioactive sources. Where the exposure to the radiation or radioactive substances is the subject of a trial, the experts of Turkish Atomic Energy Authority provide professional assistance to the judges on the issue.
In the present study, the aim was to assess the awareness degree of the physicians and other professionals employing in neurosurgery clinics about the potential exposure to the detrimental rays and radioactive substances due to the use of fluoroscopy. In addition, the legal rights of the health-care professionals employing not only in radiology clinics but also in neurosurgery and other clinics who are likely to be exposed to the radiation were also examined.
MATERIALS AND METHODS
Ethics permission
The aim and benefits were explained to the volunteers, and survey forms were filled out without mentioning names. Physicians and other personnel were informed, and their consents were obtained. The approval of the hospital directors was taken to conduct a survey among physicians and other staff ( February 19, 2019). Ethics committee approval was not required since the present study comprised a retrospective review of records and a survey conducted among health-care professionals.
Type and setup of the research
The data used in the present study were obtained from multicentered neurosurgery clinics. Physicians and other personnel involved in the fluoroscopy procedure were included. The survey was conducted based on the principle of voluntariness. The questions and results were evaluated by an independent researcher who was also blind to study.
The questions related to the fluoroscopy procedure were prepared considering data of the International Atomic Energy Agency.[
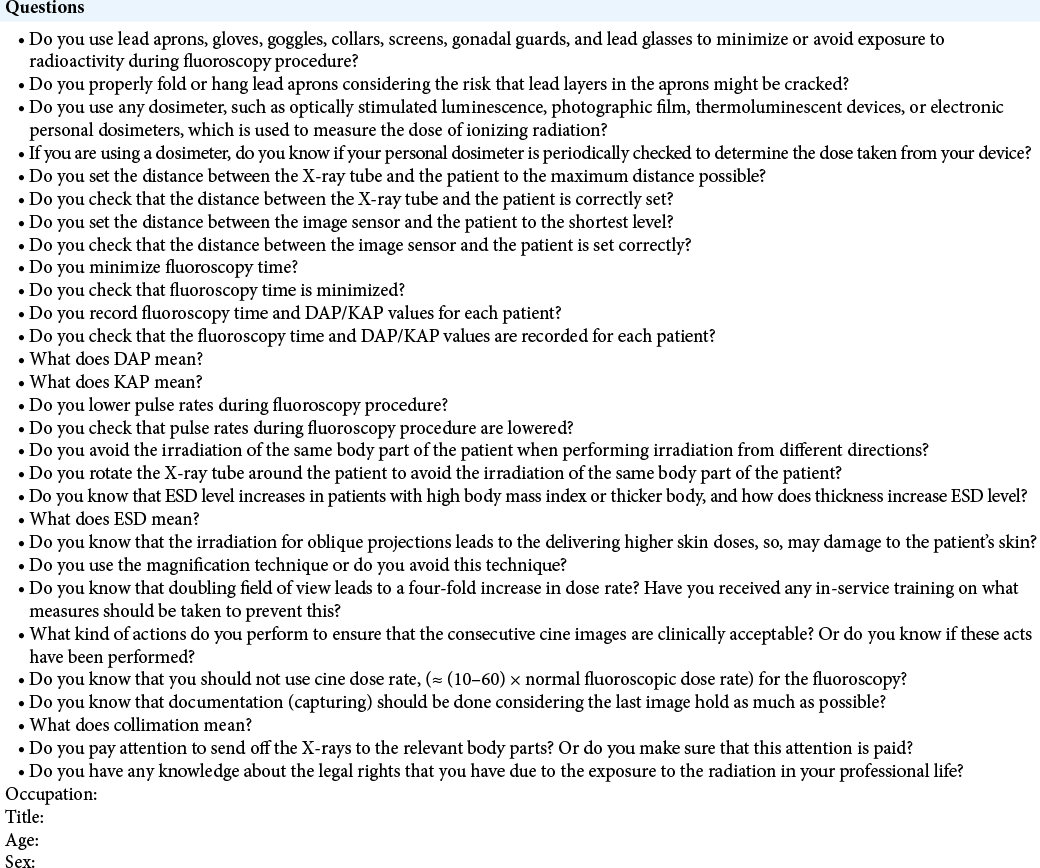
Thirty questions on the matter of research and four questions on the demographic data were included in the questionnaire.
Random sampling was then performed, and questionnaire forms [
Statistical analysis of the survey results
The statistical analyses were performed using Minitab (version 18.0) software, and the alpha significance value was accepted as P < 0.05. Descriptive statistics were presented as the mean ± standard deviation (SD) or frequency (%). Mann–Whitney U-test and Fisher’s exact test were used to compare the differences between independent variables. The Chi-square test was used to compare categorical variables between groups.
RESULTS
The application duration of the survey was lower than 7 ± 3 min (average time ± SD, min). Thirty-one males and one female neurosurgeon responded to all questions in the questionnaire. Six operating room nurses (one female and five males) and three health-care personnel working in the operating room also participated in the survey. The neurosurgeons participating in the survey composed of three professors, eight assistant professors, specialist physicians, and six research assistants. The mean age of the participants was 38.40 ± 10.14 years.
Operating room personnel were observed not to use neither lead apron nor other protective equipment. Moreover, no health-care personnel wore dosimeter during fluoroscopy procedure even though they were in the operating room. The participants were no knowledge about the safety requirements that should be complied with, except for the necessity of properly hanging of the lead aprons after surgery to prevent damage to these aprons. They did not even receive in-service training on the matter.
Nurses were observed not to use any protective equipment or wear a dosimeter but use lead apron. The nurses were also observed to accurately know the distance between the X-ray tube and the patient, and the sending off the X-rays to the relevant body part. The responses given by them revealed that they did not receive any in-service training on the matter. The extent of surgeons, nurses, and other operating room personnel knowledge on the issue differed from each other, however, this was not statistically significant (P > 0.05).
Of the six research assistants, 9.75% used a lead apron, 2.43% wore a dosimeter, and 33.33% accurately knew the distance between the X-ray tube and the patient. Other than the mentioned points, the research assistants were observed not to correctly answer any questions. Of the neurosurgeons, 46.15% had awareness of using protective equipment to minimize or avoid exposure to radioactivity, 19.23% worn a dosimeter, 26.92% correctly set the distance between the image sensor and the patient, 15.38% recorded fluoroscopy time and DAP/kerma-area product (KAP) values for each patient, and 7.69% avoided the irradiation of the same parts of the patient’s skin when performing irradiation from different directions.
One neurosurgeon was observed to know the requirement of not using cine dose rate for fluoroscopy. Two participants, one professor and one assistant professor, had certain knowledge about their legal rights. Three neurosurgeons knew that documentation should be done considering the last image hold as much as possible. One specialist physician knew the meaning of the term of collimation. No neurosurgeons knew the meaning of the terms of DAP and KAP. None of the participants received in-service training on the issue.
Physicians and other health-care professionals participating in the survey were observed not to have any knowledge on the matter, and they did not even receive in-service training. Few neurosurgeons were observed to have knowledge about whether such records were kept in the operating rooms.
DISCUSSION
C-arm digital fluoroscopy is used in a wide variety of surgical interventions such as spine surgeries, some cranial surgeries, transforaminal and caudal epidural steroid injections, as well as for the evaluation of annular tears and extravasations in the intervertebral discs.[
Adverse effects such as radiation dosage a health-care professional can be exposed to, the amount of radioactive substance that can be emitted to the environment in the operating rooms, the precautions that must be taken to avoid the mentioned adverse effects in health-care units are regulated by the domestic and international law. However, the measures that must be taken to avoid the negative effects of radiation during radiological imaging performed with portable or mobile devices in neurology and neurosurgery clinics may not be as adequate and effective as those in radiology clinics.
As is well known, fluoroscopy is an imaging technique that employs X-rays to get real-time moving images of the body. Health-care unit professionals such as physicians and technicians are exposed to the detrimental effects of the X-rays when using fluoroscopy. In an opinion letter of the Turkish Atomic Energy Authority, dated April 12, 2011, and numbered 5010, related to the Radiological Devices License, the radioactive sources used in health-care units are defined as follows: “the main sources of ionizing radiation used in health-care units are devices such as c-arm scopy, u-arm scopy, o-arm scopy, Cyberknife, Gamma Knife, simulator, CT simulator, as well as other similar devices used in the operating rooms.”
Article 4/I of the Regulation on the Working Principles with Ionizing Radiation in Healthcare Units, issued in the Official Gazette in July 5, 2012, defines personnel who are exposed to the ionizing radiation in workplaces as follows: individuals who are more likely to be exposed to the ionizing radiation above the dose limits, specified in the Radiation Safety Regulation, issued in the Official Gazette in March 24, 2000, to which ordinary people are likely to be exposed in daily life.
The Radiation Safety Regulation also includes a similar provision. Article 4/H defines radiation officer as follows: a person who is more likely to be exposed to radiation above the dose limits specified in the article 10 of this regulation due to the use of a source of radiation in the workplace. However, the Radiation Safety Code, issued in the Official Gazette in September 7, 1985, defines the term of the radiation officer in a slightly different manner. According to article 2/K: a person constantly works in controlled areas or in a workplace where radiation sources are constantly used. Given the above-mentioned provisions, health-care professionals who temporarily use devices emitting radioactive substance or who work in a unit where radiation sources are temporarily used are not considered as a radiation officer in Turkish practice.
An annual dose of radioactive substance a person can be exposed to is determined in the article 10 of the radiation safety regulation as follows: for radiation officers, the effective dose cannot exceed 20 mSv for an average of 5 consecutive years and 50 mSv for 1 year. The annual equivalent dose limit for hand, foot, or skin is 500 mSv and 150 mSv for the eye lens. The equivalent dose of 1 cm2 area exposed to the highest radiation dose for the skin is the average skin equivalent dose regardless of the dose to which other parts of the body are exposed.
Article 103 of the Civil Servants Law No.657 is as follows: officers who are exposed to the radioactive rays in their workplaces are granted a monthly extra-annual leave along with their paid annual leave. Furthermore, article 23 of the Regulation on Radiology, Radium and Electrical Treatment and Other Physiotherapy Institutions provides that the personnel who are exposed to radiation in workplaces are granted a month of extra-annual leave along with a paid annual leave. Considering all the above-mentioned provisions on the issue, it is obvious that health-care professionals working in either public or private hospitals are granted 1 month of extra-annual leave on healthy purpose if they are exposed to radioactive substance above the dose limits specified in the radiation safety regulation, that is, without the requirement of performing a constant work in a health-care unit where radiation sources are used. In conclusion, the sole legal condition that must be fulfilled to have the right to 1 month of extra-annual paid leave is to be exposed to the radiation dose beyond limits determined in the radiation safety regulation. Accordingly, not only personnel working in radiology clinics but also those working in clinics where radiation sources such as fluoroscopy are used may request 1 month of extra-annual leave. The dosage of radiation to which the health-care professionals are exposed in a year should be gauged by an expert on this issue, then if the dosage exposed to exceed the level indicated in the radiation safety regulation, 1 month of extra-annual leave must be granted without considering the clinics where the personnel are working. Therefore, health-care professionals working either in a public or private hospital should submit an official petition including their request of 1 month of extra-annual leave due to the exposure to the radiation. In the case of the nonacceptance of the request, they are entitled to bring the case before the administrative or labor courts. During the trial, the dosage of the radiation exposure in a year is gauged by the experts designated by the judges; subsequently, the court accedes to the request of the complainant if the dosage exposed to exceed the limits enshrined in the regulation. Therefore, health-care professionals may also have 1 month of extra-annual leave due to the exposure to the radiation on the judgment of the court.
In addition, the article 40 of the Social Security Law No. 5510 defines the health-care personnel who have a right to length of the service pay increase as follows: health-care personnel such as physicians, dentists, technicians, other staffs, radiation physicists, and technicians, working in health-care units where ionizing radiations such as X-rays, radium, and similar substances are used. The personnel who are legally entitled to the length of the service pay increase should be designated using the same procedure explained above for the entitlement of 1 month of extra-annual leave.
There are two studies on radiation exposure originating in the use of fluoroscopy.[
As is well known, the guidelines include the following notice: the physicians or personnel performing the procedure should use lead aprons, gloves, goggles, collars, screens, gonadal guards, and lead glasses to minimize or avoid exposure to radioactivity.[
The data obtained through survey revealed that neurosurgeons, nurses, and other operating room personnel did not pay attention to the safety requirements that should be complied with to minimize or avoid exposure to radiation and radioactive substances. More interestingly, two neurosurgeons only knew the legal rights they might possess due to the exposure to the radiation or radioactive substances. Other health-care professionals had no knowledge about their legal rights.
CONCLUSION
It should be remembered that not only the personnel or physicians in the radiology departments but also those in the neurosurgery departments are working continuously with devices emitting radiation. Therefore, they are exposed to some extent to the radioactive substances or radiation in workplaces. In all cases, the dosage of radiation to which the health-care professionals are exposed in a year should be gauged by an expert on this matter, then if the dosage exposed to exceed the level indicated in the Radiation Safety Regulation, the relevant personnel should enjoy the above-mentioned rights laid down in the law. Health-care professionals should effectively receive in-service training on this issue to have more knowledge about their legal rights, and they should also receive effective and adequate in service training concerning the protection from radiation exposure in their workplaces.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We, the authors, would like to thank Ibrahim YILMAZ, Ph.D. in the University of Istanbul Medipol, Department of Medical Pharmacology, for his statistical assessment of the data. Before applying the questionnaire to the health-care professionals participating in the study, we have conducted a preliminary study to evaluate the reliability of the questionnaire and have applied this questionnaire to an independent person from the study. We would like to thank Assoc. Prof. M.D., Necati KAPLAN, a neurosurgeon in Istanbul Rumeli University, Corlu Reyap Hospital, Clinics of Neurosurgery, for his precious support in this preliminary testing process.
References
1. Autsavapromporn N, Plante I, Liu C, Konishi T, Usami N, Funayama T. Genetic changes in progeny of bystander human fibroblasts after microbeam irradiation with X-rays, protons or carbon ions: The relevance to cancer risk. Int J Radiat Biol. 2015. 91: 62-70
2. Chavan MS, Chavan PM, Sable D, Pande S, Inamdar H, Kunjir G. Are gingival cells more sensitive to genotoxic effects caused by dental radiography?. Oral Oncol. 2018. 87: 201-2
3. Constitution of the Republic of Turkey. Available from: https://www.anayasa.gov.tr/en/legislation/turkish-constiution [Last accessed on 2020 Jun 20].
4. de González AB, Darby S. Risk of cancer from diagnostic X-rays: Estimates for the UK and 14 other countries. Lancet. 2004. 363: 345-51
5. Denko NC, Green SL, Edwards D, Giaccia AJ. p53 checkpoint-defective cells are sensitive to X rays, but not hypoxia. Exp Cell Res. 2000. 258: 82-91
6. Hak DJ. Radiation exposure during intramedullary nailing. Injury. 2017. 48: 26-9
7. Hwang YM, Lee MH, Kim SJ, Lee SW, Chung HW, Lee SH. Comparison of radiation exposure during fluoroscopy-guided transforaminal epidural steroid injections at different vertebral levels. Korean J Radiol. 2015. 16: 357-62
8. Karaarslan N, Yilmaz I, Ozbek H, Sirin DY, Kaplan N, Caliskan T. Are radio-contrast agents commonly used in discography toxic to the intact intervertebral disc tissue cells?. Basic Clin Pharmacol Toxicol. 2019. 124: 181-9
9. Kim SJ, Lee MH, Lee SW, Chung HW, Lee SH, Shin MJ. Radiation exposure for fluoroscopy-guided lumbosacral epidural steroid injections: Comparison of the transforaminal and caudal approaches. J Spinal Disord Tech. 2014. 27: 37-40
10. Mori R, Matsuya Y, Yoshii Y, Date H. Estimation of the radiation-induced DNA double-strand breaks number by considering cell cycle and absorbed dose per cell nucleus. J Radiat Res. 2018. 59: 253-60
11. Navarro-Ramirez R, Lang G, Lian X, Berlin C, Janssen I, Jada A. Total navigation in spine surgery; a concise guide to eliminate fluoroscopy using a portable intraoperative computed tomography 3-dimensional navigation system. World Neurosurg. 2017. 100: 325-35
12. Noguchi M, Kanari Y, Yokoya A, Narita A, Fujii K. Live-cell imaging study of mitochondrial morphology in mammalian cells exposed to X-rays. Radiat Prot Dosimetry. 2015. 166: 101-3
13. Qing Y, Yang XQ, Zhong ZY, Lei X, Xie JY, Li MX. Microarray analysis of DNA damage repair gene expression profiles in cervical cancer cells radioresistant to 252Cf neutron and X-rays. BMC Cancer. 2010. 10: 71
14. Radiation Protection of Patients. Available from: https://www.iaea.org/resources/rpop [Last accessed on 2020 Jul 17].
15. Scherer K, Yaroshenko A, Bölükbas DA, Gromann LB, Hellbach K, Meinel FG. X-ray dark-field radiography in vivo diagnosis of lung cancer in mice. Sci Rep. 2017. 7: 402
16. Shi Y, Zhang X, Tang X, Wang P, Wang H, Wang Y. MiR-21 is continually elevated long-term in the brain after exposure to ionizing radiation. Radiat Res. 2012. 177: 124-8
17. Tandon V, Raheja A, Suri A, Chandra PS, Kale SS, Kumar R. Randomized trial for superiority of high field strength intra-operative magnetic resonance imaging guided resection in pituitary surgery. J Clin Neurosci. 2017. 37: 96-103
18. Urboniene A, Sadzeviciene E, Ziliukas J. Assessment of eye lens doses for workers during interventional radiology procedures. Radiat Prot Dosimetry. 2015. 165: 299-303
19. Vanaclocha-Vanaclocha V, Verdú-López F, Sáiz-Sapena N, Herrera JM, Rivera-Paz M. Biplanar X-ray fluoroscopy for sacroiliac joint fusion. Neurosurg Focus. 2016. 41: 1