- Department of Neurosurgery, Sri Sathya Sai Institute of Higher Medical Sciences, Whitefield, Bengaluru, Karnataka, India
- Department of Finance and Accounts, Sri Sathya Sai Institute of Higher Medical Sciences, Whitefield, Bengaluru, Karnataka, India
- Department of Neurosurgery, Loma Linda University, Loma Linda, California, USA
Correspondence Address:
Sumit Thakar
Department of Neurosurgery, Sri Sathya Sai Institute of Higher Medical Sciences, Whitefield, Bengaluru, Karnataka, India
DOI:10.4103/2152-7806.162484
Copyright: © 2015 Thakar S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Thakar S, Dadlani R, Sivaraju L, Aryan S, Mohan D, Sai Kiran NA, Rajarathnam R, Shyam M, Sadanand V, Hegde AS. A value-based, no-cost-to-patient health model in the developing world: Critical appraisal of a unique patient-centric neurosurgery unit. Surg Neurol Int 07-Aug-2015;6:131
How to cite this URL: Thakar S, Dadlani R, Sivaraju L, Aryan S, Mohan D, Sai Kiran NA, Rajarathnam R, Shyam M, Sadanand V, Hegde AS. A value-based, no-cost-to-patient health model in the developing world: Critical appraisal of a unique patient-centric neurosurgery unit. Surg Neurol Int 07-Aug-2015;6:131. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-value%e2%80%91based-no%e2%80%91cost%e2%80%91to%e2%80%91patient-health-model-in-the-developing-world-critical-appraisal-of-a-unique-patient%e2%80%91centric-neurosurgery-unit/
Abstract
Background:It is well-accepted that the current healthcare scenario worldwide is due for a radical change, given that it is fraught with mounting costs and varying quality. Various modifications in health policies have been instituted toward this end. An alternative model, the low-cost, value-based health model, focuses on maximizing value for patients by moving away from a physician-centered, supply-driven system to a patient-centered system.
Methods:The authors discuss the successful inception, functioning, sustainability, and replicability of a novel health model in neurosurgery built and sustained by inspired humanitarianism and that provides all treatment at no cost to the patients irrespective of their socioeconomic strata, color or creed.
Results:The Sri Sathya Sai Institute of Higher Medical Sciences (SSSIHMS) at Whitefield, Bengaluru, India, a private charitable hospital established in 2001, functions on the ideals of providing free state-of-the-art healthcare to all in a compassionate and holistic manner. With modern equipment and respectable outcome benchmarks, its neurosurgery unit has operated on around 18,000 patients since its inception, and as such, has contributed INR 5310 million (USD 88.5 million) to society from an economic standpoint.
Conclusions:The inception and sustainability of the SSSIHMS model are based on self-perpetuating philanthropy, a cost-conscious culture and the dissemination of human values. Replicated worldwide, at least in the developing nations, this unique healthcare model may well change the face of healthcare economics.
Keywords: Neurosurgery, no-cost-to-patient health model, patient-centric, value-based
INTRODUCTION
Health models worldwide have been long riddled with escalating costs, varying the quality of care and ethical concerns related to commercialization of healthcare.[
THE SRI SATHYA SAI INSTITUTE OF HIGHER MEDICAL SCIENCES MODEL
The SSSIHMS is a zero revenue (and therefore nonprofit by definition) charitable hospital that functions on the principles (as laid down by its founder, Sri Sathya Sai Baba) that ideal healthcare should be universal (accessible to all irrespective of economic or insurance status, creed, color, religion or nationality), free-of-charge, compassionate (based on human values), comprehensive (directed toward the body, mind, and spirit), and preventative. This billing-free, 333-bed tertiary-care hospital (providing services in neurology, neurosurgery, cardiology, and cardiothoracic surgery) was established in 2001 in Whitefield, Bengaluru, India along the lines of its predecessor, the SSSIHMS at Puttaparthi, India, that has been running successfully for more than two decades now. All services in the hospital (surgery, consultations, laboratory and radiological investigations, ward stay, and Intensive Care Unit (ICU) stay, drugs, etc.) are provided at no cost to the patients. The running cost of the hospital is met by the income generated from a corpus fund that was instituted at the hospital's inception by totally unsolicited donations from thousands of individuals and several corporations, both national and international. Although several privately owned hospitals in India and elsewhere do provide free or subsidized care to some patients, SSSIHMS is arguably the only tertiary-care hospital without a billing department and as such, is a unique experience that has attracted patients and visitors from other countries, as well. Factors that have sustained and promoted the growth of the hospital include self-perpetuating humanitarianism, a set of caregivers inspired by the ethos of such a healthcare system, and an intensely cost-conscious culture.
THE NEUROSURGERY UNIT AND ITS VALUE TO THE COMMUNITY
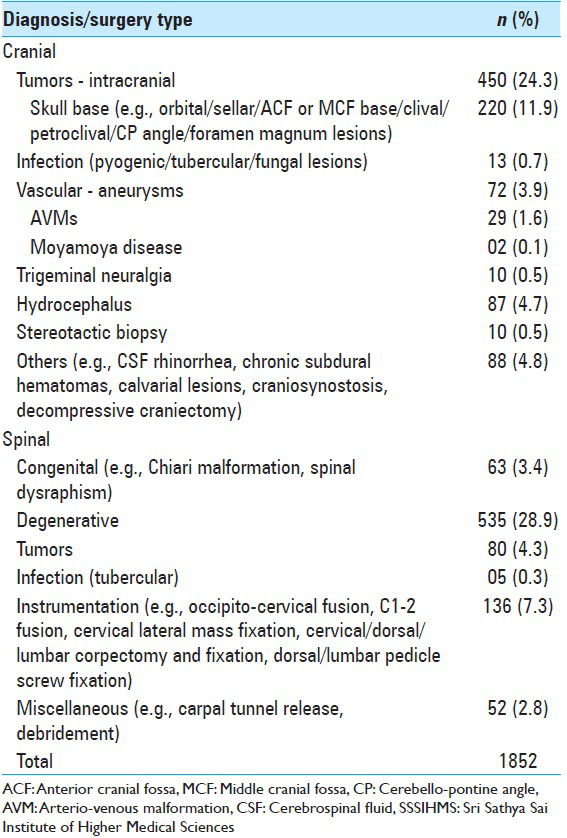
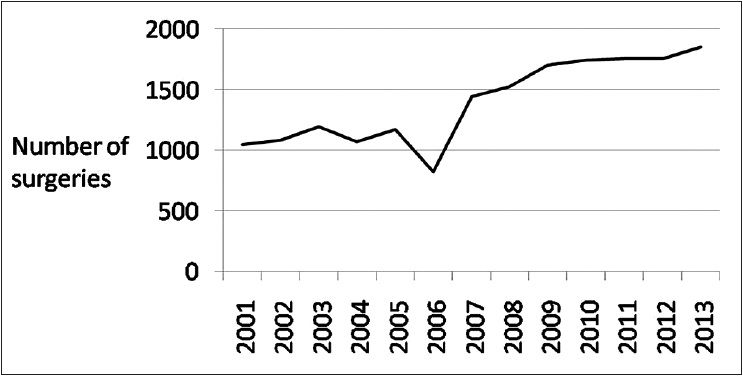
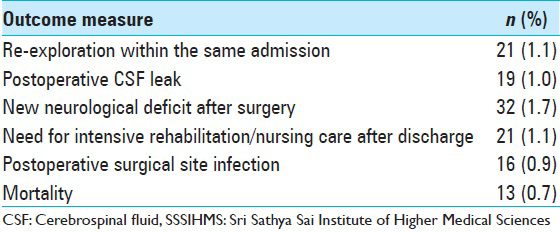
The SSSIHMS neurosurgery unit has performed 196,696 out-patient consultations (including those for patients making their first visit, and for subsequent re-visits, including postdischarge visits for operated patients), 4586 teleconsultations and 18,179 nontrauma related surgeries of varying complexity in the period, January 2001 to December 2013. In the same period, 26,221 diagnostic or follow-up computed tomography (CT) scans, 79,766 magnetic resonance imaging (MRI) scans, and 2096 angiographies were done for patients in the unit. The unit is equipped with state-of-the-art equipment that includes a Leica OH5 operating microscope with fluorescence imaging, a Medtronic S7 neuronavigation system, an intraoperative monitor (Nihon-Kohden), and a Karl Storz endoscopy set. The surgical team (consisting of five consultants and five residents) has performed 1852 surgeries in the period, January 2013 to December 2013 [
STANDARDS OF CARE
At SSSIHMS, the decision on the type of intervention and the degree of care including the length of postoperative stay for a given patient is ascertained on the basis of evidence-based standards of care and is not biased by factors like cost or insurance status. Patients also benefit from a host of free-of-charge facilities that ensure multi-modality treatment, augment patient comfort and provide ease of access for follow-up. Nonsurgical utilities include a 128-slice, 750 HD CT scanner (GE Medical Systems), a Magnetom Aera 1.5 T MRI (Siemens), an Artis Zee biplane neuro-vascular lab (Siemens), automated laboratory services and blood bank (backed by voluntary blood donors), dietary counseling and physiotherapy. Nonneurosurgical specialty services in the disciplines of cardiology and cardiothoracic surgery are provided by the SSSIHMS, while services in the general specialties are offered by an affiliated general hospital that also follows the five principles of ideal healthcare listed earlier. In addition, a panel of doctors from various specialties, and across different hospitals provide consultations for in-patient referrals free of cost, moved by the altruistic nature of the hospital. As a step beyond treating just the physical aspect of disease in an attempt to deliver “whole-person care,”[
COST-CONSCIOUS CULTURE
Assessing cost implications of every decision is inviolable as SSSIHMS has a fiduciary responsibility to the donors of the Sri Sathya Sai Central Trust's (SSSCT) corpus and further, as the free medical care provided by SSSIHMS is not reimbursed by any third-party payers. Cost consciousness without quality compromise pervades across the hospital, and prudent expenditure is a shared goal. This culture, in fact, forms the basis for SSSIHMS's ability to meet rising costs. Being a zero income model, there is no price list for the rendered services. The cost structure consequently is the key economic driver and enables budgetary allocation of resources to support the periodic activity objectives, evaluation of capital expenditure options, assessment of asset performance and utilization reviews, and identification of cost control opportunities.
Cost evaluation is supported by a robust costing methodology that includes all operating and capital, fixed and variable cost elements. Using a mix of top-down and bottom-up costing methods based on the principles of relevance, accuracy, transparency, and materiality, costs are computed at three main cost object levels. First, they are aggregated at points-of-service delivery- at the OR, ICU, ward, and outpatient clinic. Second, average per episode cost (intervention and stay) are computed for “surgery types” for similar combinations of “surgery site” (cranial/spinal)-“procedure”-“implant use” features. Third, cost per consultation at the outpatient clinic is measured. The principles of time-driven activity based costing[
Policies and processes are designed to highlight the cost-effectiveness of alternative options and cost implications of decisions - both for acquisition and for utilization of all resources. Some of the general policies related to cost-containment in acquisition of equipment and consumables at SSSIHMS include selecting equipment for absolute patient-care value rather than their flair quotient, centralization of purchases for all hospitals managed by the SSSCT, inclination toward long-term contracts to fix reasonable and stable rates, direct imports rather than third party purchases, establishing forward contracts (for imports) to hedge against exchange rate fluctuations, following a “just in time” ordering method where feasible and minimizing wastage/pilferage. Cost-containment initiatives in utilization include in-house innovations like the “stores module” - an inventory management system developed by the Information Systems Department; rigorous efforts to ensure optimal utilization of resources wherever possible such as avoidance of unnecessary investigations, minimizing surgical unit time, rigid infection control, and application of economies of scale; and decreasing equipment-related “cost per unit” by maximal utilization of their capacity. Such stringent financial budgeting and also independent goal-setting by clinical departments help balance available resources against the demand.
Human resource cost, which is a major contributor to total healthcare costs, is controlled by offering fixed remuneration to all medical and nonmedical staff. Without volume-based incentives, there are no unnecessary orders for investigation or consultations that tend to occur in the fee-for-service system. Performance incentives arise from commitment to the five founding principles and evidence of definitive individual impact on patient well-being. In managing people cost, as well as in other aspects, the financial system of the SSSIHMS health model merits substantially from the dissemination of human values in its structure, as detailed in the section below.
Based on present billing rates at Indian corporate hospitals, the market value of surgeries performed at SSSIHMS in 2013, is estimated to be INR 556 million (USD 9.3 million). As an illustration of how the cost per surgery at SSSIHMS compares with that elsewhere, spinal fusion with instrumentation costing approximately INR 80,000 (USD 1333) in SSSIHMS would have cost around USD 5500 in a corporate hospital in India, and around USD 43,000 in the United States.[
ROLE OF HUMAN VALUES
Sri Sathya Sai Baba's emphasis on universal values (truth, love, right conduct, peace, and nonviolence) and holistic patient-centric care (“Love all, Serve all,” “Patient First, Institution Next, Staff Last”) set the basis for the SSSIHMS ethos. Hippocrates has remarked that it is more important to know and care for the patient than it is to know and care for the disease. Indeed, it is even better to know and care for both, and this remains the cornerstone of the commitment made by the SSSIHMS. Given the importance of the value-based attitude and ethics that have helped to build and sustain this high-volume unit, the staff here is selected on a “hire for attitude and train for skills” principle. Recognizing the long-term, nonfinancial rewards of working in such a system, even the medical professionals willingly accept a moderate, need-based pay, and some voluntarily assume multiple responsibilities or even prefer to render honorary services. Such an inspiring ethos precludes any tendency to get influenced by commercial inducements that may otherwise result in the use of drugs or equipment that are more expensive than necessary. A sense of ownership amongst committed caregivers leads to a higher productivity and cost-effective delivery of care, an overall low staff attrition rate (9.72% for the 2013–2014 financial year compared to a national average attrition rate of 14% in the healthcare sector) that helps in containing induction- and training-related costs, and an improved quality of care that results in better outcomes. The existence of a common, noble shared purpose engaging the physicians, as seen here, has indeed been cited as a crucial starting point in the healthcare revolution.[
REPLICABILITY OF THE SRI SATHYA SAI INSTITUTE OF HIGHER MEDICAL SCIENCES MODEL
The need for a synthesis of professionalism and the practice of human values in optimal neurosurgical practice has been acknowledged.[
CONCLUSIONS
The neurosurgery unit at the SSSIHMS, a private charitable hospital, has been providing high-value, holistic treatment at no cost to its patients for more than a decade. The inception and sustainability of the model are based on self-perpetuating philanthropy, a cost-conscious culture and the dissemination of human values. Replicated worldwide, at least in the developing nations, this unique healthcare model may well change the face of healthcare economics.
ACKNOWLEDGMENTS
The authors acknowledge the assistance provided by Mr. Krishna Kumar Parthasarathy, Controller, Finance and Accounts, SSSIHMS, Bengaluru during the preparation of the manuscript.
References
1. Berger D. Corruption ruins the doctor-patient relationship in India. BMJ. 2014. 348: g3169-
2. Dadlani R, Mani S, Jai Ganesh AU, Mohan D, Rajgopalan N, Thakar S. The impact of telemedicine in the postoperative care of the neurosurgery patient in an outpatient clinic: A unique perspective of this valuable resource in the developing world - An experience of more than 3000 teleconsultations. World Neurosurg. 2014. 82: 270-83
3. Daly R. Putting physicians in the lead for cost containment. Healthc Financ Manage. 2013. 67: 52-9
4. Last accessed on 2014 Sep 05. Available from: http://www.oecd.org/els/health-systems/48723982.pdf .
5. El-Sayed AM, Ziewacz JE, Davis MC, Lau D, Siddiqi HK, Zamora-Berridi GJ. Insurance status and inequalities in outcomes after neurosurgery. World Neurosurg. 2011. 76: 459-66
6. Kanat A, Epstein CR. Challenges to neurosurgical professionalism. Clin Neurol Neurosurg. 2010. 112: 839-43
7. Kaplan RS, Anderson SR. Time-driven activity-based costing. Harv Bus Rev. 2004. 82: 131-8, 150
8. Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011. 89: 46-52, 54, 56
9. Koenig H, King D, Carson VB.editors. Handbook of Religion and Health. New York: Oxford University Press; 2012. p.
10. Krause JH. Regulating, guiding, and enforcing health care fraud. N Y Univ Annu Surv Am Law. 2004. 60: 241-
11. Lee TH, Cosgrove T. Engaging doctors in the health care revolution. Harv Bus Rev. 2014. 92: 104-11
12. Mackintosh M, Koivusalo M.editors. Commercialization of Health Care: Global and Local Dynamics and Policy Responses. New York: Palgrave Macmillan; 2005. p.
13. Porter ME, Lee TH. The strategy that will fix health care. Harv Bus Rev. 2013. 91: 50-70
14. Puchalski CM. Integrating spirituality into patient care: An essential element of person-Centered care. Pol Arch Med Wewn. 2013. 123: 491-7
15. Sanghavi DM. What makes for a compassionate patient-caregiver relationship?. Jt Comm J Qual Patient Saf. 2006. 32: 283-92
16. Last accessed on 2015 Jun 20. (Online article) http://www.nashp.org/wp-content/uploads/sites/default/files/cost_containment_approaches.pdf .
17. Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evid Rep Technol Assess (Full Rep). 2006. 132: 1-71
18. Spath PL.editors. Error Reduction in Health Care: A Systems Approach to Improving Patient Safety. San Francisco, CA: John Wiley and Sons; 2011. p.







Dr. Miguel Faria
Posted August 11, 2015, 9:16 pm
This is an interesting paper that deserves serious consideration for health care strategies in underdeveloped nations and even in some developed nations — particularly funding uninsured patients or charity cases in cases of free-market, private medical/surgical care.
The operating cost of $88.5 million (USD) and the surgery costs of 9.3 million at SSSIHMS in 2013 in India are very low by Western standards, but very efficiently provided medical/surgical care. If these services were provided in developed nations, it would have translated into hundreds of millions, if not billions of U.S. dollars. The authors provide a vivid example of efficient cost-effectiveness: “ a spinal fusion with instrumentation costing approximately INR 80,000 (USD 1333) in SSSIHMS would have cost around USD 5500 in a corporate hospital in India, and around USD 43,000 in the United States.”
The efforts of this institution and its physicians and nurses are highly commendable. The authors should be congratulated.
Aruni mahapatra
Posted August 13, 2015, 5:31 am
Brilliant article indeed. Happy note that importance of the role of human values above doctor patient billing relationship . On the replicability of such model I am happy to inform you that such a hospital has already started in Naya Raipur , Sri Sathya Sai Sanjeevani Hospital . You have pointed out requirements of Corpus fund as a pre requisite to start such hospital, but this hospital has done more than 1000 heart surgeries on pediatric patient totally free of cost without any access to corpus fund. It has been made successful by men of High ideals and Values and total commitment to practicing those ideals.
viswanath
Posted August 16, 2015, 7:16 am
It was going to be inaugarated by APJ Kalam I read. But i dont see any mention of this in the Trust’s website. Is it not run by Swami’s trust or Is it not yet fully functional?
Sri Ramulu Elluru
Posted August 14, 2015, 1:39 pm
I am happy to see that this Temple of Healing is doing so well. I remember being a student at Sri Sathya Sai Institute of Higher Learning when it was inaugurated in 2000. It is an ideal role model for low cost health care systems around the world.
Dr Kiron Bala Arora
Posted August 15, 2015, 4:02 am
Bhagavan is called a miracle man by many, as He gifted tokens of His Divine Love to one and all beyond any man made human divisions or considerations. But above those ‘visiting cards’ as He called them, He performed the ‘Miracle of love’ by touching the hearts of millions across the globe, by establishing ‘Temples of Healing’, Temples of Learning’ and ‘Temples of transformation’ through the pure drinking water He provided and is providing to millions even today. These are His real miracles, to be emulated by men and women who believe in goodness and greatness, which lies in giving.
Michael
Posted August 17, 2015, 5:13 pm
This is the most amazing description of a free healthcare model I have ever come across.
Hats off to the founder, Sathya Sai Baba, and to the motivated team that have helped sustain the model. This, indeed, may pave the way for better healthcare the world over.
Satya Jnana Dutt
Posted August 23, 2015, 4:29 am
I am a happy beneficiary and an operated patient at Sri Sathya Sai Institute of Higher Medical Sciences. The environment and the staff will ensure and builds patients confidence, then the treatment starts.
Suresh Rao Savkur
Posted July 30, 2016, 5:58 am
Very thought provoking and informative article by Sumit T and his co research workers. Need wide publicity. Thank you for the article.