- Department of Spine Surgery, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
Correspondence Address:
Rajendra Sakhrekar, Department of Spine Surgery, Sancheti Institute of Orthopedics and Rehabilitation, Pune, Maharashtra, India.
DOI:10.25259/SNI_409_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rajendra Sakhrekar1, Shailesh Hadgaonkar1, Manisha Hadgaonkar1, Parag Sancheti1, Ashok Shyam1. Achondroplasia with seronegative spondyloarthropathy resulting in recurrent spinal stenosis : A case report. 19-Jul-2021;12:354
How to cite this URL: Rajendra Sakhrekar1, Shailesh Hadgaonkar1, Manisha Hadgaonkar1, Parag Sancheti1, Ashok Shyam1. Achondroplasia with seronegative spondyloarthropathy resulting in recurrent spinal stenosis : A case report. 19-Jul-2021;12:354. Available from: https://surgicalneurologyint.com/surgicalint-articles/10984/
Abstract
Background: Achondroplasia is an autosomal dominant condition caused by the G380 mutation of the gene encoding fibroblast growth factor receptor 3 on chromosome 4P. The classical findings include rhizomelic extremities, short stature, and spinal stenosis involving the upper cervical and distal lumbar spine. Rarely, achondroplasia coexisting with seronegative spondyloarthropathy can result in recurrent canal stenosis. Here, we report a 36-year-old male with symptomatic recurrent L3-L4 spinal stenosis 9 years following an original L2-S1 lumbar decompression for stenosis.
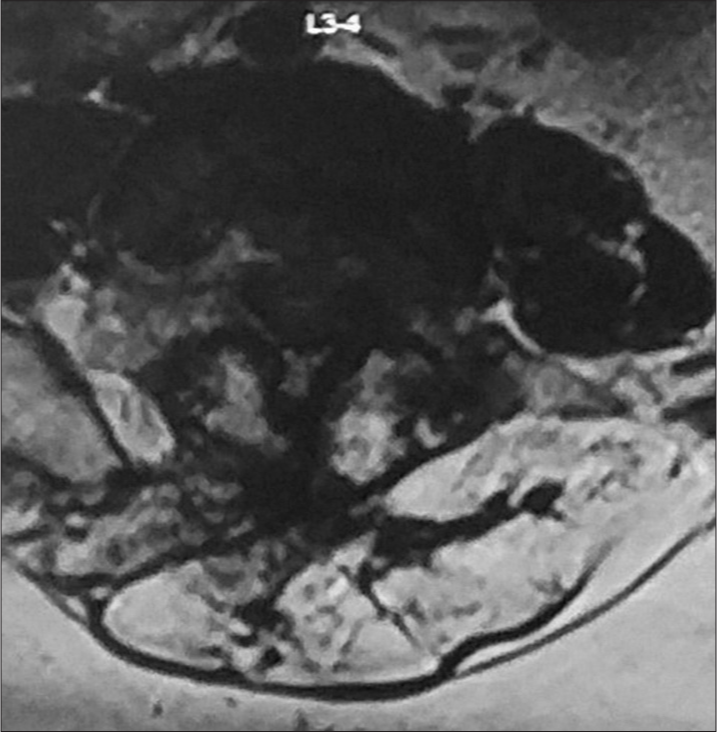
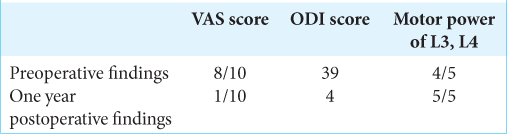
Case Description: A 36-year-old male with achondroplasia (height of 113 cm and weight 43 kg [BMI-33.7]) presented with low back and right lower extremity sciatica (ODI 39). He had achondroplasia with a short stature. Nine years ago, he had an L2-S1 laminectomy for decompression of stenosis. When the new MRI revealed recurrent severe L3-4 stenosis, he underwent a repeated L3-L4 decompression with fusion. One year later, the patient was neurologically intact with radiographic confirmation of adequate L3-L4 arthrodesis.
Conclusion: A 36-year-old male with achondroplasia and a history 9 years ago of an L2-S1 laminectomy for stenosis, presented with symptoms and signs of recurrent L3-L4 stenosis that responded to repeated decompression and fusion.
Keywords: Achondroplasia, Lumbar canal stenosis, Resurgery, Seronegative spondyloarthritis, VAS score
INTRODUCTION
Achondroplasia an autosomal dominant caused by a mutation of the G380 gene encoding fibroblast growth factor receptor 3 on chromosome 4P.[
CASE PRESENTATION
A 36-year-old male with achondroplasia (113 cm and weight 43 kg [BMI-33.7] with forehead prominence) presented with low back pain and right lower extremity sciatica of 6 months duration. On examination, the patient was wheelchair bound, had difficulty standing, and could not walk independently (4/5 motor dysfunction diffusely throughout both lower extremities and diffuse hypoesthesia in the L3, L4 distributions). Nine years ago, he had undergone a L2-S1 decompressive laminectomy for stenosis with good resolution of his symptoms. New radiographic studies now showed recurrent L3-L4 lumbar stenosis. Plain lumbar X-rays demonstrated fusion between the L1-L3 and L3-L5 lumbar levels, with osseous fusion of the right sacroiliac joint accompanied by irregularity of the left S1 joint cortex due to advanced seronegative spondyloarthropathy [
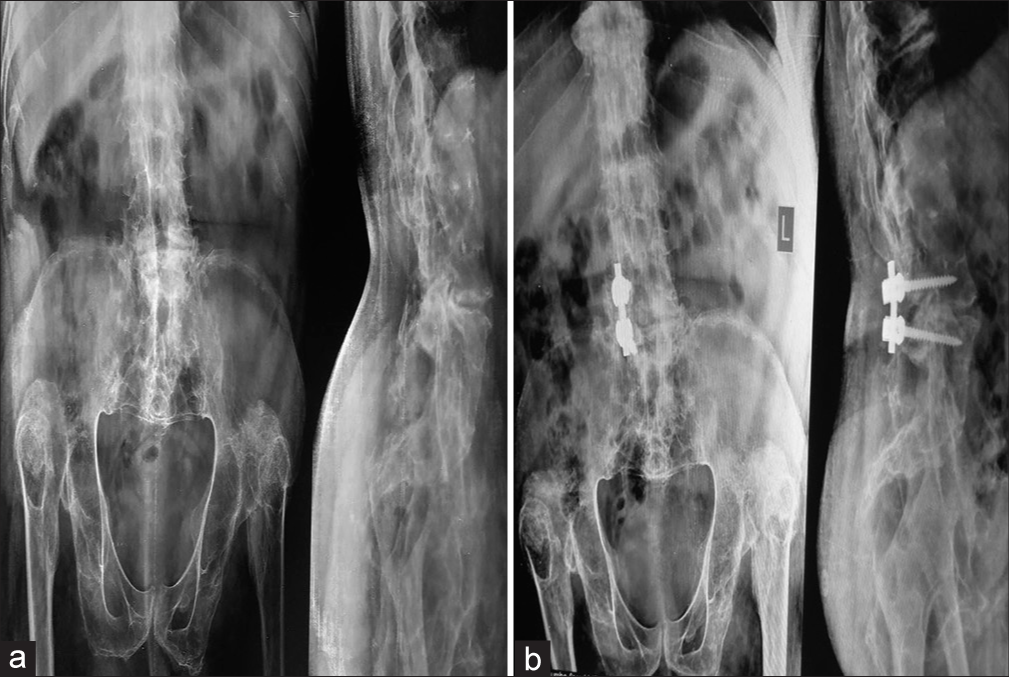
Figure 1:
Preoperative X-ray of lumbosacral spine (anteroposterior and lateral): X-ray suggestive of degenerative changes of lumbar spine and osseous fusion of the right SI joint with irregularity of cortex in the left SI joint. (b) Postoperative X-ray lumbosacral spine (anteroposterior and lateral): posterior decompression at L3-4 and fusion was achieved with the right side unilateral instrumented stabilization and interbody fusion with bone graft.
Surgery
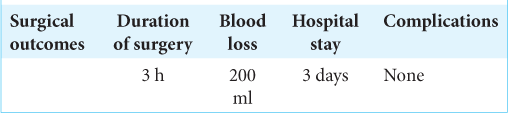
The patient underwent a wide bilateral microscope-assisted decompressive L3-L4 laminectomy for resection of L3-L4 bony spurs, L3-4 discectomy, interbody fusion using local autograft, and L3-L4 right-sided instrumented stabilization [
Postoperative outcomes
Postoperatively, the patient neurologically improved; he walked with a walker on the day of surgery and was able to return to work 6 weeks later. One year postoperatively, his motor deficit fully resolved (i.e. to 5/5) [
DISCUSSION
Patients with achondroplasia and congenitally shortened pedicles are susceptible to developing cervical, thoracic, and/or lumbar stenosis. Patients typically become symptomatic in their 30s though 50s due to accelerated disc degeneration, lumbar kyphosis, hypertrophy of ligamentum flavum, bone spurs, and thickened laminae/facet joints.[
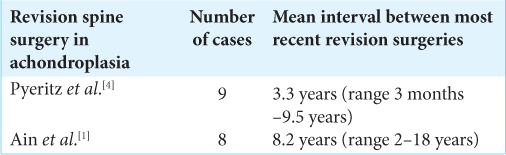
There is often a need for revision spine surgery in these patients attributed to their accelerated facet hypertrophy associated with their genetic defect (i.e., an exaggerated response to normal motion leading to early degeneration)[
CONCLUSION
Patients with achondroplasia who have previously undergone lumbar decompressive surgery may develop recurrent lumbar stenosis that responds well to repeated surgical intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ain MC, Elmaci I, Hurko O, Clatterbuck RE, Lee RR, Rigamonti D. Reoperation for Spinal Restenosis in Achondroplasia. J Spinal Disord. 2000. 13: 168-73
2. Ain MC, Abdullah MA, Ting BL, Skolasky RL, Carlisle ES, Schkrohowsky JG. Progression of low back and lower extremity pain in a cohort of patients with achondroplasia. J Neurosurg. 2010. 13: 335-40
3. Bailey JA. Orthopaedic aspects of achondroplasia. J Bone Joint Surg Am. 1970. 52: 1285-301
4. Pyeritz RE, Sack GH, Udvarhelyi GB. Thoracolumbosacral laminectomy in achondroplasia: Long-term results in 22 patients. Am J Med Genet. 1987. 28: 433-44
5. Saito K, Miyakoshi N, Hongo M, Kasukawa Y, Ishikawa Y, Shimada Y. Congenital lumbar spinal stenosis with ossification of the ligamentum flavum in achondroplasia: A case report. J Med Case Rep. 2014. 8: 88
6. Thomeer RT, van Dijk JM. Surgical treatment of lumbar stenosis in achondroplasia. J Neurosurg. 2002. 96: 3