- Division of Neurosurgery, University of Calgary, Calgary, Alberta, Canada
- Department of Diagnostic Imaging, University of Calgary, Calgary, Alberta, Canada
Correspondence Address:
Albert M. Isaacs
Division of Neurosurgery, University of Calgary, Calgary, Alberta, Canada
DOI:10.4103/sni.sni_218_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ben-Israel D, Isaacs AM, Morrish W, Gallagher NC. Acute vertex epidural hematoma. Surg Neurol Int 07-Sep-2017;8:219
How to cite this URL: Ben-Israel D, Isaacs AM, Morrish W, Gallagher NC. Acute vertex epidural hematoma. Surg Neurol Int 07-Sep-2017;8:219. Available from: http://surgicalneurologyint.com/surgicalint-articles/acute-vertex-epidural-hematoma/
Epidural hematomas (EDH) are often located at the cerebral hemisphere convexities or the posterior fossa often following trauma. The offending source of bleeding in a majority of EDHs is secondary to arterial, venous, or bony vascular channel compromise.[
We present a previously healthy 26-year-old male seen at our tertiary center 6-hours after sustaining blunt force trauma to the head. He was found to be Glasgow Coma Scale (GCS) 14, disoriented, intermittently bradycardic, but had no focal neurologic deficits. A computer tomography (CT) scan [
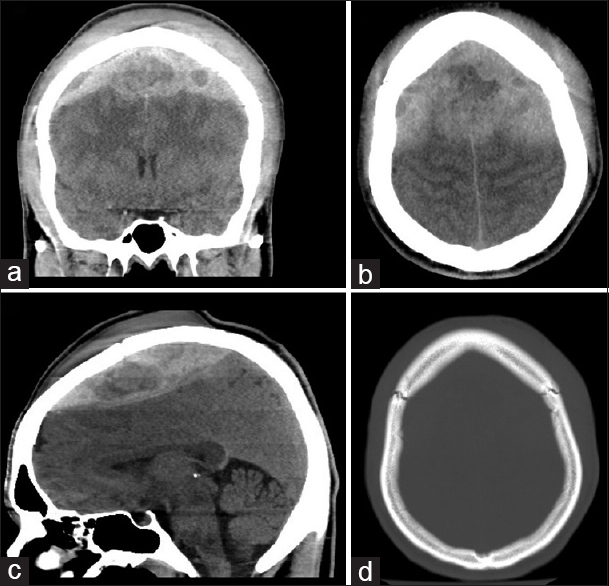
Figure 1
Preoperative noncontrast CT head – (a) coronal cut at the level of the sphenoid sinus, (b) vertex axial cut, (c) mid-sagittal cut, showing a large vertex epidural hematoma with mixed density suggestive of hyperacute hemorrhage, active extravasation and downward herniation. (d) vertex axial cut, bone window, showing coronal suture diastasis
Given the prolonged lucid interval, it was felt the hemorrhage was likely venous in etiology. A CT venogram (CTV) [
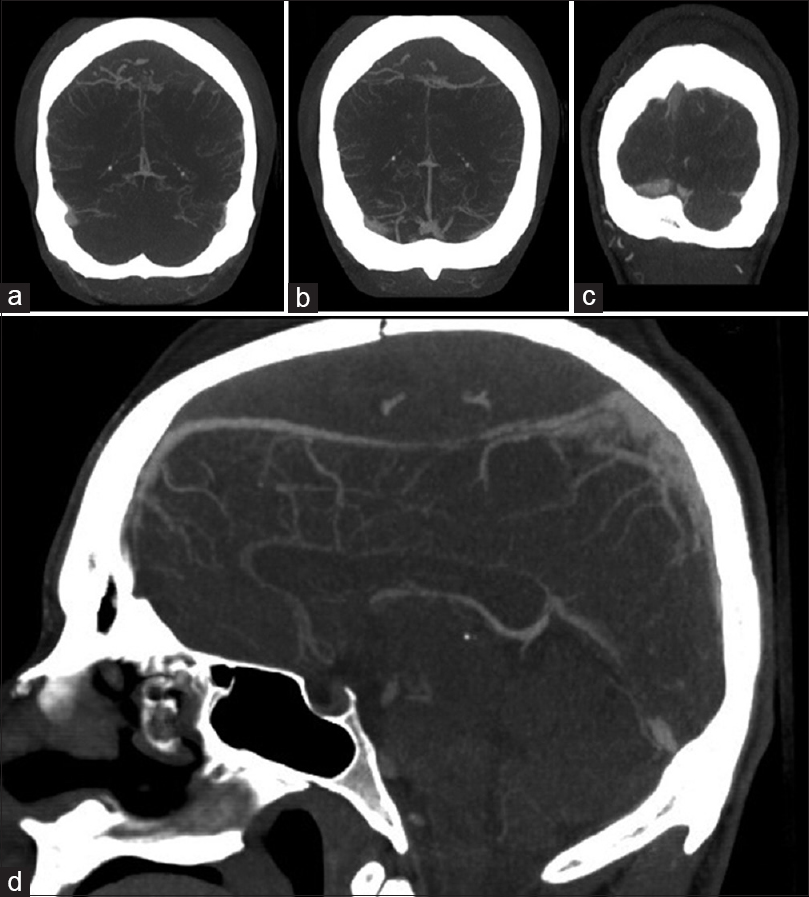
Figure 2
Preoperative CT angiogram head – (a-c) coronal cuts, progressively more posterior, showing downward displacement of the superior sagittal sinus (SSS) with spot signs within the epidural hematoma suggestive of active extravasation. (d) mid-sagittal cut, showing attenuation of the SSS in the posterior frontal region suggesting possible sinus injury or compression
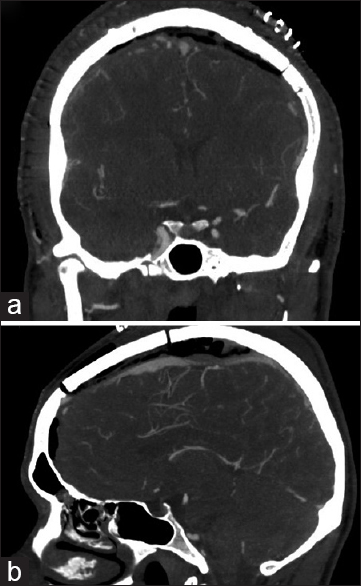
The patient underwent an emergency bifrontal craniotomy for vEDH evacuation. No SSS injury was identified, though several arachnoid granulations were seen actively bleeding. This was controlled with Gelfoam, active pressure, and Tisseel fibrin glue. The bone flap was then replaced and the subgaleal hematoma evacuated. Postoperative imaging [
DISCUSSION
In the pre-magnetic resonance imaging era, acute vEDH were thought to comprise only around 1–8% of all EDHs.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Behera SK, Senapati SB, Mishra SS, Das S. Management of superior sagittal sinus injury encountered in traumatic head injury patients: Analysis of 15 cases. Asian J Neurosurg. 2015. 10: 17-20
2. Bimpis A, Marcus HJ, Wilson MH. Traumatic bifrontal extradural haematoma resulting from superior sagittal sinus injury: Case report. JRSM Open. 2015. 6: 2054270415579137-
3. Datta SGS. Bilateral vertex extradural hematomas: A case report. Indian J Neurotrauma. 2008. 5: 109-11
4. Harbury OL, Provenzale JM, Barboriak DP. Vertex epidural hematomas: Imaging findings and diagnostic pitfalls. Eur J Radiol. 2000. 36: 150-7
5. Miller DJ, Steinmetz M, McCutcheon IE. Vertex epidural hematoma: Surgical versus conservative management: Two case reports and review of the literature. Neurosurgery. 1999. 45: 621-