- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia,
- School of Public Health, University of Alberta, Edmonton, Alberta, Canada.
- Division of Neurosurgery, Department of Surgery, University of Alberta, Edmonton, Alberta, Canada.
- Department of Critical Care Medicine, University of Alberta, Edmonton, Alberta, Canada.
Correspondence Address:
Yahya H. Khormi
Department of Critical Care Medicine, University of Alberta, Edmonton, Alberta, Canada.
DOI:10.25259/SNI_123_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yahya H. Khormi, Ambikaipakan Senthilselvan, Cian O’kelly, David Zygun. Adherence to brain trauma foundation guidelines for intracranial pressure monitoring in severe traumatic brain injury and the effect on outcome: A population-based study. 23-May-2020;11:118
How to cite this URL: Yahya H. Khormi, Ambikaipakan Senthilselvan, Cian O’kelly, David Zygun. Adherence to brain trauma foundation guidelines for intracranial pressure monitoring in severe traumatic brain injury and the effect on outcome: A population-based study. 23-May-2020;11:118. Available from: https://surgicalneurologyint.com/surgicalint-articles/10036/
Abstract
Background: Severe traumatic brain injury (TBI) is a significant cause of death and disability. The objective of this study was to provide an overview of whether adherence to brain trauma foundation (BTF) guidelines improved outcomes following TBI utilizing intracranial pressure (ICP) monitoring.
Methods: This cohort study between 2000 and 2013 involved 1848 patients who sustained severe blunt TBI. Outcomes were correlated with whether or not ICP monitoring was utilized based on BTF guidelines.
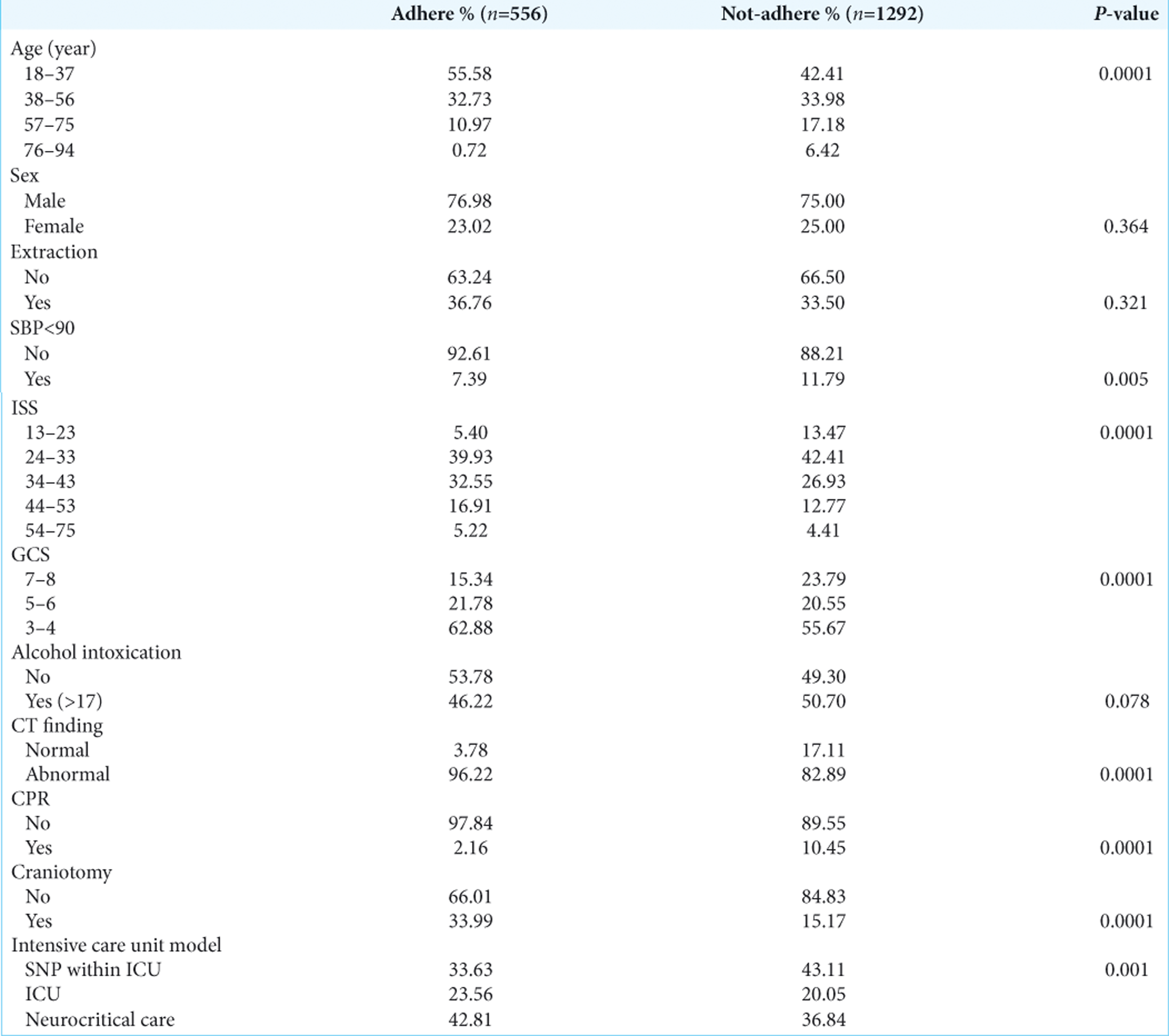
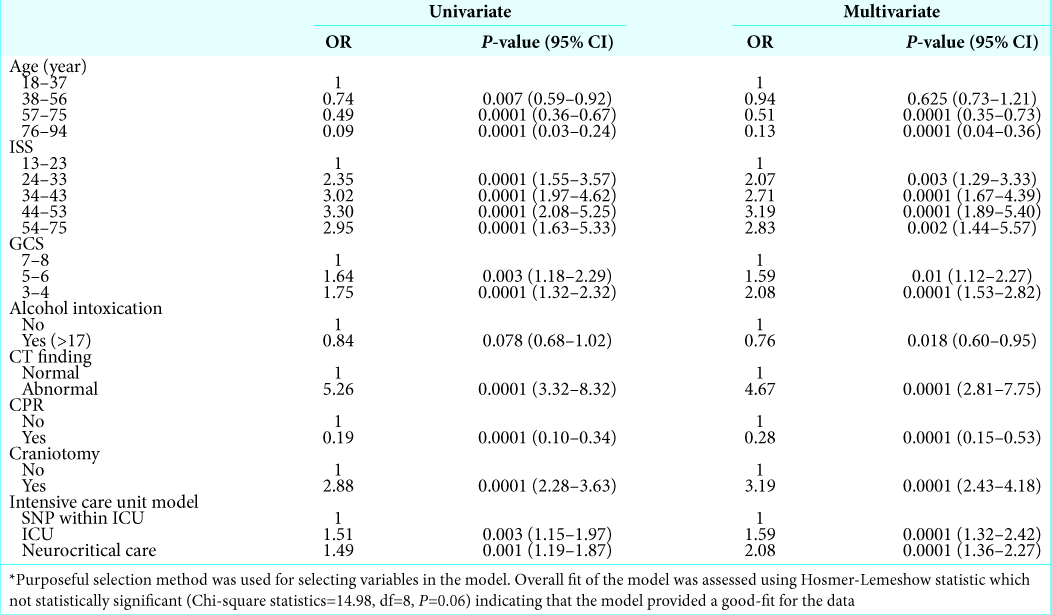
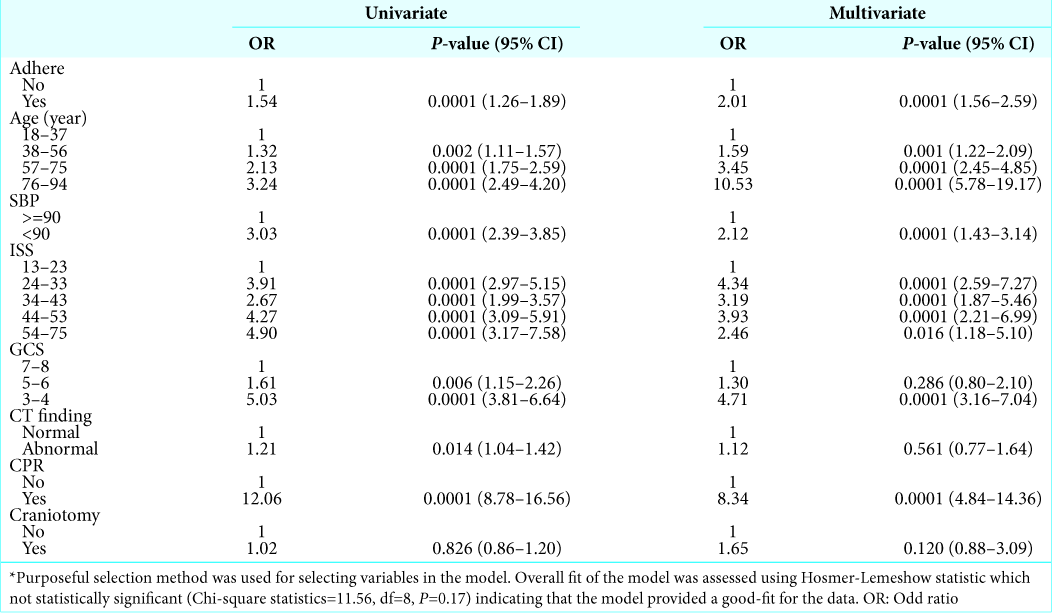
Results: The BTF guideline adherence rate for utilizing ICP monitoring in patients with TBI was 30% in 1848 patients. Adherence rates positively correlated with younger age, high injury severity scores, lower Glasgow Coma Scores, abnormal computed tomography scans of the head, performance of a craniotomy, neurocritical care unit admission, the lack of alcohol intoxication, and the absence of a cardiac arrest. Greater adherence to BTF guidelines was associated with higher mortality rates (OR 2.01, 95% CI: 1.56–2.59, P P
Conclusion: Adherence rates to BTF guidelines for ICP monitoring in patients with severe TBI were low. Further, these rates varied across centers and were correlated with higher mortality and morbidity rates. Although ICP insertion may be an indicator of TBI severity, the current BTF criteria for insertion of ICP monitors may fail to identify patients likely to benefit.
Keywords: Brain injury guideline, Brain trauma foundation guideline, Traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a significant cause of death and disability around the world.[
The brain trauma foundation (BTF) guidelines are supposed to be strictly adhered to for the management of TBI. The BTF recommends continuous ICP monitoring in all salvageable severe TBI patients (Glasgow Coma Score [GCS] ≤8) with a computed tomography (CT) scan revealing intracranial pathology. They are also to be utilized for severe TBI patients with a normal CT scan, but who exhibit two or more of the following risk factors: age over 40 years, unilateral or bilateral motor posturing, or a systolic blood pressure of <90 mm Hg.[
It has been suggested that implementation and adherence to BTF guidelines correlate with improvement in neurological outcome and reduction in mortality following severe TBI. However, there is significant variability in the use of ICP monitors and inconsistency in adherence to BTF guidelines across neurosurgical centers.[
Here, we evaluated the extent to which BTF guidelines for continuous ICP monitoring in severe TBI patients were being performed, and how it impacted outcomes.
MATERIALS AND METHODS
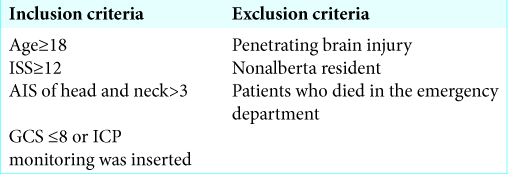
We obtained IRB approval for this population-based retrospective cohort study of TBI patients. From 2000 to 2013, 5449 patients with TBI from three trauma centers were evaluated [
The study population was stratified into two-study arms based on the adherence to BTF guidelines for insertion of ICP monitoring; (1) patients with severe TBI (GCS ≤8) and an abnormal CT scan, (2) patients with severe TBI without CT abnormalities, but with at least two of the following: age >40 years old, unilateral or bilateral motor posturing (GCS motor score ≤3), and/or a systolic blood pressure <90 mm Hg.
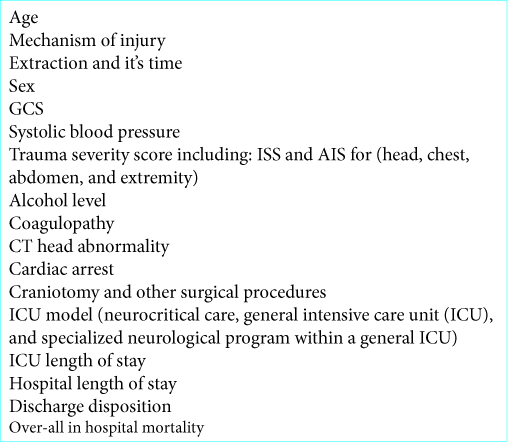
Evaluation of outcomes
Primary outcomes included assessment of adherence to BTF guidelines, and in-hospital mortality. Secondary outcomes assessed morbidity including ICU and hospital length of stay (LOS), discharge disposition, and others.
Statistical methods and bias
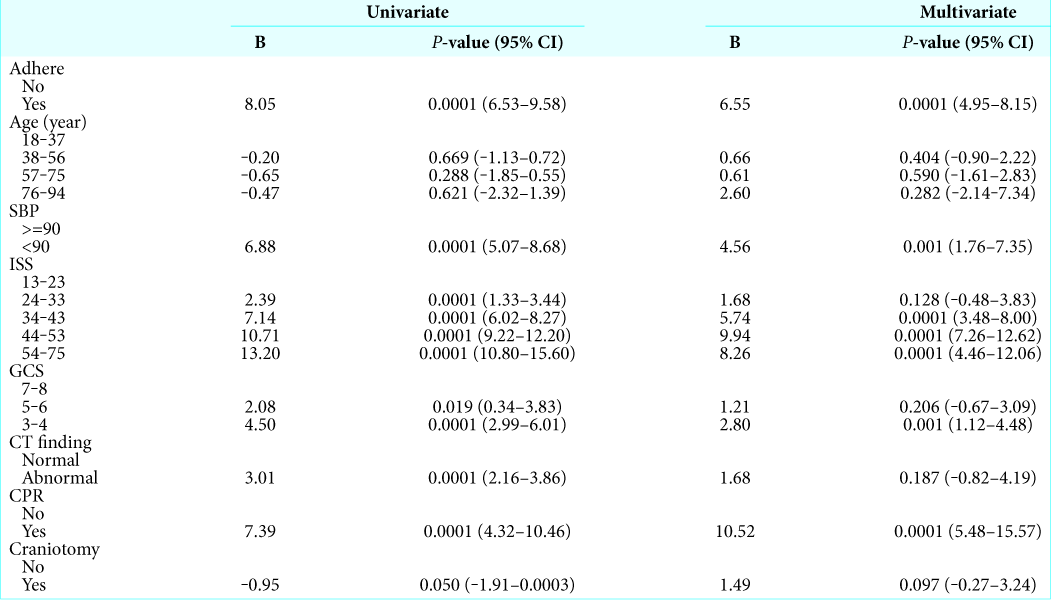
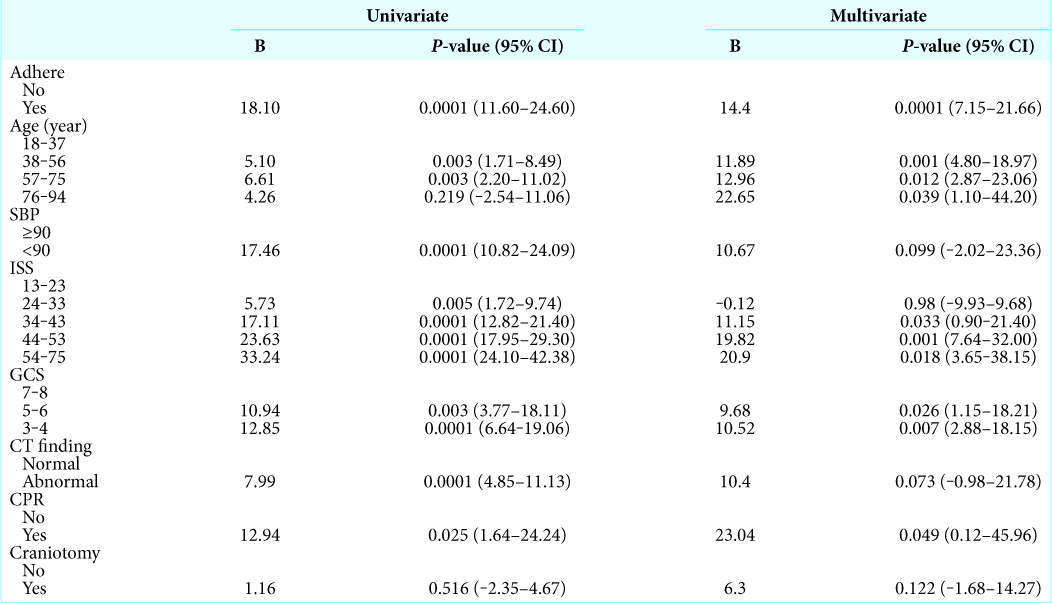
Univariate and multivariate logistic and linear regression were used to assess outcome. A purposeful selection method was deployed using variables after univariate analysis to identify the predictors of adherence and confounders effect on outcome.
All statistical analyses were performed using Stata 13.1. P < 0.05 was considered statistically significant.
RESULTS
Adherence rates to BTF criteria
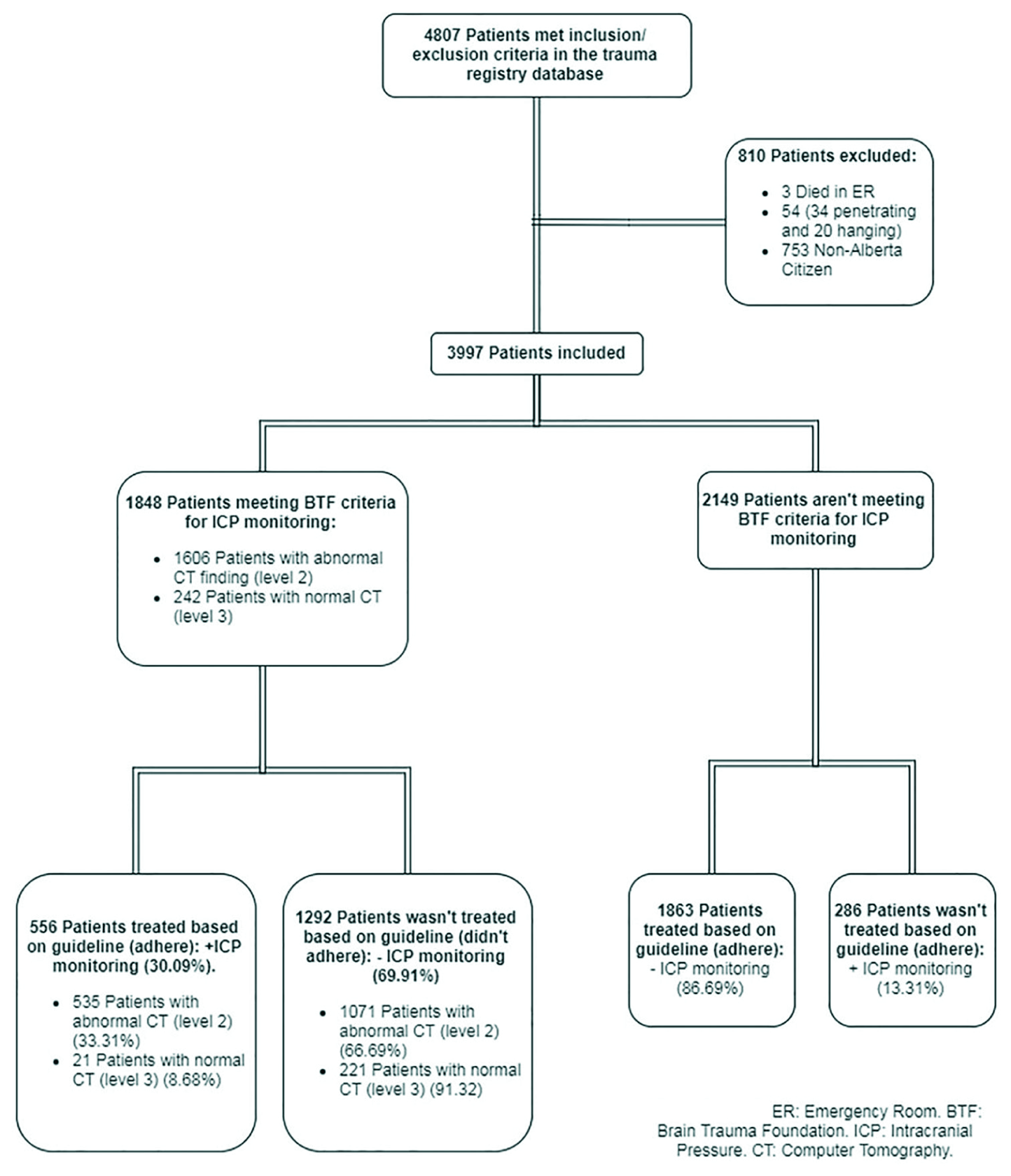
There were 1848 patients who met the BTF guidelines for ICP monitoring; of these, 1606 had abnormal CT scans.
The adherence rate to BTF guidelines for the insertion of an ICP monitor in TBI patients was highest among those with abnormal CT studies (1606 patients; 33.31%) versus normal CT’s (8.68% of 242 patients). Notably, just 556 (30.09%) patients received ICP monitors [
Predicting ICP monitoring adherence
Baseline demographics, injury characteristics, and the model of care systems for ICP adherence and nonadherence groups were analyzed [
Strict adherence to BTF criteria for ICP monitoring in TBI patients was lowest in the specialized neurological program within a general ICU model (center). Further, the general ICU model (center) had a lower adherence rate versus the neurocritical model (center) [
Summary of morbidity and mortality rates
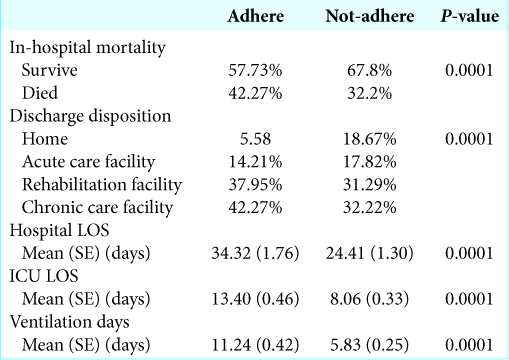
In-hospital, the mortality was 42% in the adherent group and 32% in nonadherent group [
Adherence to ICP monitoring following BTF guidelines was associated with an average higher LOS in the ICU (>7 days), and hospital (>14 days). Other variables were associated with longer ventilation times, ICU and length of hospital stays are listed in [
In the sensitivity analysis from excluding patients who died within 48 h of admission, the association between adherence to BTF of ICP monitoring and mortality was greater (OR: 4.59 P = 0.0001).
DISCUSSION
Our study showed that ICP monitoring was performed in a minority of patients with severe traumatic brain injuries who meet the current BTF criteria (30.1%). Adherence rates were significantly different across different critical care units; this rate is even lower than those reported in UK (43% and 46%), Austria (56%),[
Adherence was lower in patients with a normal CT scan and two or more risk factors; age, BP, and motor GCS (9%) versus patients with abnormal intracranial finding (33%). This suggests that clinicians are likely not convinced that ICP monitoring in this subgroup of severe TBI patients is necessary.
In this study, ICP monitoring was associated with the higher mortality and morbidity despite controlling multiple confounders.
CONCLUSION
In a large sample of Canadian TBI patients, adherence to BTF guidelines for ICP monitoring was low and varied across centers, especially if CT studies were normal. Further, ICP monitoring was associated with the higher mortality rates and ICU/hospital lengths of stay.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Biersteker HA, Andriessen TM, Horn J, Franschman G, Van der Naalt J, Hoedemaekers CW. Factors influencing intracranial pressure monitoring guideline compliance and outcome after severe traumatic brain injury. Crit Care Med. 2012. 40: 1914-22
2. Bratton SL. Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma. 2007. 24: S37-44
3. . Available from: http://www.cihi.ca [Last accessed on 2018 Aug 10].
4. Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017. 80: 6-15
5. Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012. 367: 2471-81
6. Mauritz W, Steltzer H, Bauer P, Dolanski-Aghamanoukjan L, Metnitz P. Monitoring of intracranial pressure in patients with severe traumatic brain injury: An Austrian prospective multicenter study. Intensive Care Med. 2008. 34: 1208-15
7. Sahjpaul R, Girotti M. Intracranial pressure monitoring in severe traumatic brain injury--results of a Canadian survey. Can J Neurol Sci. 2000. 27: 143-7
8. Saul TG, Ducker TB. Effect of intracranial pressure monitoring and aggressive treatment on mortality in severe head injury. J Neurosurg. 1982. 56: 498-503
9. Shafi S, Diaz-Arrastia R, Madden C, Gentilello L. Intracranial pressure monitoring in brain-injured patients is associated with worsening of survival. J Trauma. 2008. 64: 335-40
10. Stocchetti N, Picetti E, Berardino M, Buki A, Chesnut RM, Fountas KN. Clinical applications of intracranial pressure monitoring in traumatic brain injury: Report of the Milan consensus conference. Acta Neurochir (Wien). 2014. 156: 1615-22
11. Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H. Intracranial pressure monitoring in severe head injury: Compliance with brain trauma foundation guidelines and effect on outcomes: A prospective study. J Neurosurg. 2013. 119: 1248-54
12. Zygun DA, Laupland KB, Hader WJ, Kortbeek JB, Findlay C, Doig CJ. Severe traumatic brain injury in a large Canadian health region. Can J Neurol Sci. 2005. 32: 87-92