- Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
Correspondence Address:
Shigeomi Yokoya, Department of Neurosurgery, Saiseikai Shiga Hospital, Imperial Gift Foundation Inc., Ritto, Shiga, Japan.
DOI:10.25259/SNI_574_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeomi Yokoya, Hideki Oka, Akihiko Hino. Adhesion between an extruded coil and the oculomotor nerve: Unexpected interference due to coil extrusion. 26-Aug-2022;13:390
How to cite this URL: Shigeomi Yokoya, Hideki Oka, Akihiko Hino. Adhesion between an extruded coil and the oculomotor nerve: Unexpected interference due to coil extrusion. 26-Aug-2022;13:390. Available from: https://surgicalneurologyint.com/surgicalint-articles/11822/
Abstract
Background: When direct clipping is performed for a recurrent aneurysm after coil embolization, there are sometimes findings of the coil adhering to the surrounding tissue, after it has been extruded from inside the aneurysm into the subarachnoid space and brain parenchyma. However, there have only been few previous reports on extruded coils adhering to the cranial nerves, preventing aneurysm dissection and clip application.
Case Description: We performed the coil embolization of a ruptured aneurysm originating from the bifurcation of basilar artery and superior cerebellar artery in a 36-year-old male patient. Recurrence was confirmed 5 years after embolization and direct clipping was performed. The intraoperative finding was that part of the coil was strongly adhering to or encircling the oculomotor nerve, making it difficult to achieve sufficient mobility of the cerebral aneurysm.
Conclusion: When direct clipping is performed after coil embolization of an intracranial aneurysm, part of the coil may be extruded from the aneurysm and then adhere strongly to the cranial nerve.
Keywords: Coil embolization, Direct clipping, Extruded coils, Oculomotor nerve, Recurrent aneurysm
INTRODUCTION
There have been numerous reports that additional coil embolization is safe and efficient treatment for recurrent aneurysms after coil embolization, and according to most of these reports, endovascular treatment should be the first-line method for retreatment.[
However, for we can ascertain, there have only been few reports on extruded coils adhering to the cranial nerves,[
The present report describes a case of a coil extruded from the aneurysm into the subarachnoid space, which subsequently strongly adhered to or encircled the oculomotor nerve, and thus prevented aneurysm dissection.
CASE DESCRIPTION
A 36-year-old male patient with a history of cerebral contusion and hypertension was brought to an emergency room after waking up with a sudden severe headache. On arrival, the patient was lucid and had no neurological deficit. Head computed tomography showed a subarachnoid hemorrhage. Cerebral angiography (CAG) showed a 9 mm diameter cerebral aneurysm originating from the bifurcation of the left basilar artery and superior cerebellar artery. Coil embolization was performed on the same day. After embolization, although CAG showed a neck remnant in the aneurysm [
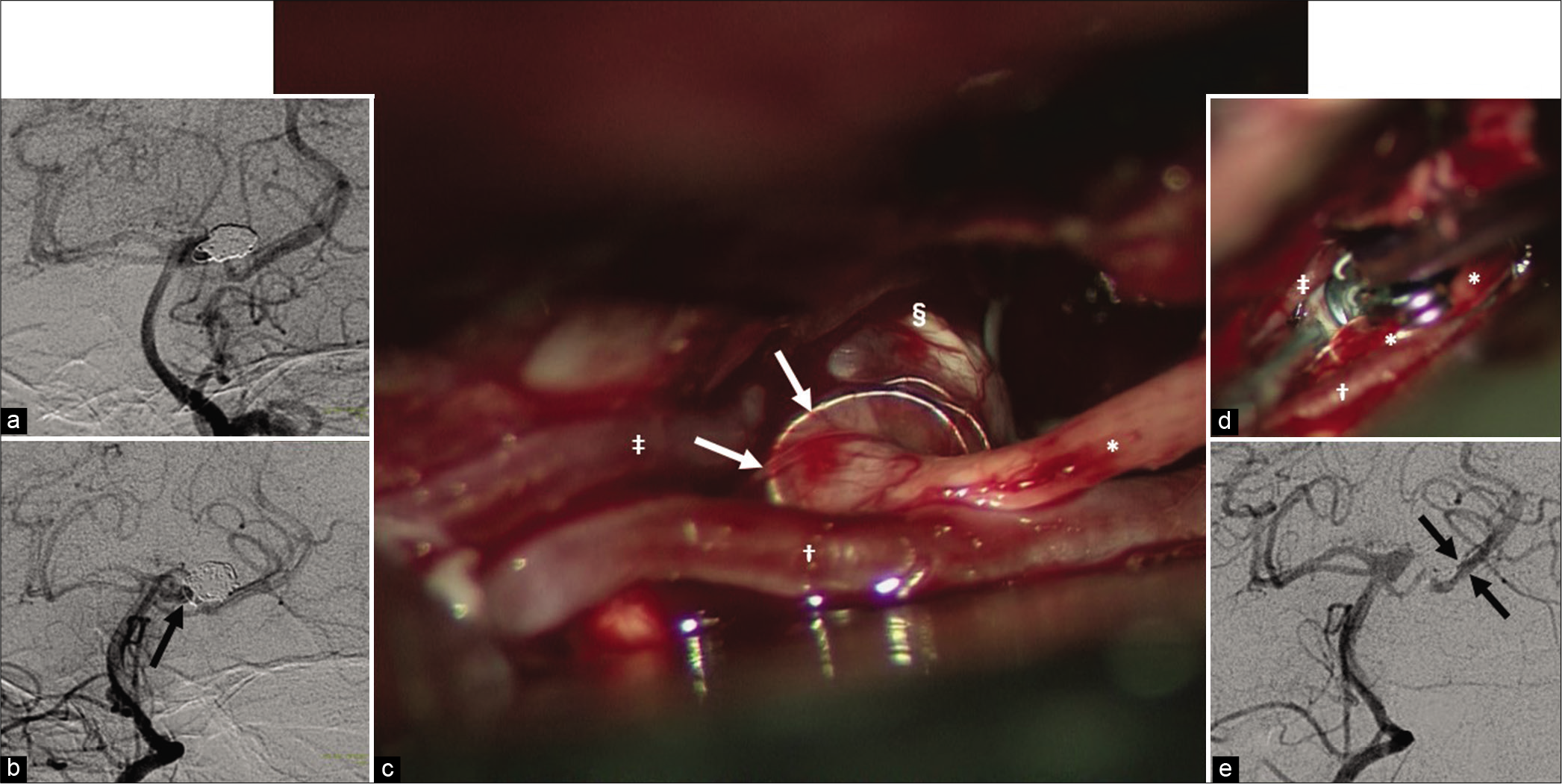
Figure 1:
(a) Cerebral angiography soon after coil embolization (anteroposterior view). A neck remnant is present, although the rupture point is occluded by the coil. (b) Cerebral angiography before direct clipping (anteroposterior view). Expansion of the neck remnant in connection with coil compaction is confirmed. In particular, the part of the coil that formed the loop (black arrow) has undergone major morphological change. (c) Intraoperative photograph of direct clipping. The coil extruded from the aneurysm (white arrow) encircles or strongly adheres to the oculomotor nerve. (d) Intraoperative photograph of the pervious clip readjustment. The previous clip occluding the posterior cerebral artery was moved. Moreover, a mini-clip was added to the suspected remnant portion. (e) Cerebral angiography after the clip readjustment (anteroposterior view). The posterior cerebral artery (paired arrows), which has disappeared before the clip readjustment, is visualized. *Oculomotor nerve, †Posterior cerebral artery, ‡Superior cerebellar artery, §Aneurysm.
DISCUSSION
This case showed that a coil extruded from inside the aneurysm into the subarachnoid space after coil embolization of a cerebral aneurysm has the potential to adhere strongly to, or encircle around, the oculomotor nerve, preventing aneurysm dissection and restricting mobility, and thus markedly interfere with the clipping procedure. Four principal mechanisms have been put forward for coil extrusion: (i) aneurysm perforation with iatrogenic extrusion of the coil; (ii) initial coiling of a pseudoaneurysm; (iii) forcible coil compaction leading to extrusion; and (iv) degradation of the distal aneurysm wall.[
To the best of our knowledge, there is only one previous report on an extruded coil adhering to the cranial nerve strongly sufficient to prevent direct clipping.[
Considering the past literature, including our case, coil extrusion may not be an unusual phenomenon in postcoiling recurrent cases. Moreover, adhesions with the cranial nerves also may not be an unusual phenomenon. The aneurysm occurring near cranial nerves, originating from the basilar and superior cerebral arteries bifurcation or from the vertebral artery and PICA bifurcation, may less likely to be retreated by direct clipping; therefore, this condition may be the reason for the limited number of reports.
More importantly, it is impossible to determine the presence or absence of adhesion to the oculomotor nerve by imaging before direct clipping. Neurosurgeons should recognize the potential for strong adhesion between the cranial nerve and extruded coil when performing direct clipping after coil embolization.
CONCLUSION
When performing direct clipping after coil embolization of an intracranial aneurysm near the cranial nerve, consideration should be given to the potential for part of the coil to be extruded from the aneurysm and to interfere markedly with the cranial nerve.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Deshaies EM. Extruded platinum coils from recurrent previously coiled intracranial aneurysms discovered at the time of microsurgical clip ligation. A report of three cases. Interv Neuroradiol. 2011. 17: 59-63
2. Dorfer C, Gruber A, Standhardt H, Bavinzski G, Knosp E. Management of residual and recurrent aneurysms after initial endovascular treatment. Neurosurgery. 2012. 70: 537-53
3. Izumo T, Matsuo T, Morofuji Y, Hiu T, Horie N, Hayashi K. Microsurgical clipping for recurrent aneurysms after initial endovascular coil embolization. World Neurosurg. 2015. 83: 211-8
4. Toyota S, Kumagai T, Goto T, Mori K, Taki T. Clipping of recurrent cerebral aneurysms after coil embolization. Acta Neurochir Suppl. 2018. 129: 53-9
5. Waldron JS, Halbach VV, Lawton MT. Microsurgical management of incompletely coiled and recurrent aneurysms: Trends, techniques, and observations on coil extrusion. Neurosurgery. 2009. 64: 301-15