- Department of Pediatric Neurosurgery, Santa Monica Maternity School - Alagoas State University of Health Sciences, Maceio, Alagoas, Brazil.
- Department of Pediatrics, Neonatal Intensive Care Unit, Santa Monica Maternity School, Maceio, Alagoas, Brazil.
Correspondence Address:
Aldo Jose Ferreira da Silva
Department of Pediatrics, Neonatal Intensive Care Unit, Santa Monica Maternity School, Maceio, Alagoas, Brazil.
DOI:10.25259/SNI_454_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aldo Jose Ferreira da Silva1, Carolina S. Magalhães e Silva2, Sonaly C. R. Mariano2. Amniotic band syndrome with double encephalocele: A case report. 22-Dec-2020;11:448
How to cite this URL: Aldo Jose Ferreira da Silva1, Carolina S. Magalhães e Silva2, Sonaly C. R. Mariano2. Amniotic band syndrome with double encephalocele: A case report. 22-Dec-2020;11:448. Available from: https://surgicalneurologyint.com/surgicalint-articles/10472/
Abstract
Background: Amniotic band syndrome (ABS) is a rare condition of controversial etiology that is associated with varying degrees of anomalies. This study reports a case of a newborn with ABS associated with double encephalocele in the frontal region.
Case Description: A 29-year-old primiparous woman with no history of prenatal infection or consanguineous marriage had a cesarean section at gestational week 38, giving birth to a newborn who was well but had limb anomalies (constriction rings, amputations, and syndactyly) and craniofacial anomalies, mainly double frontal encephalocele. The patient underwent surgical repair and subsequent placement of a ventriculoperitoneal shunt.
Conclusion: Studies clarifying this uncommon association with double encephalocele are limited. ABS associated with double encephalocele is rare and even more complex when associated with other anomalies. Thus, the conditions in such children are severe and require multidisciplinary monitoring.
Keywords: Amniotic band syndrome, Amputations, Encephalocele, Syndactyly
INTRODUCTION
Amniotic band syndrome (ABS) is a rare congenital condition. Its incidence varies from 1:1200 to 1:15,000 live births, and it has an equal distribution between sexes. The occurrence of ABS is sporadic, and the prognosis of ABS depends on the severity of the anomalies and degree of involvement of the affected organs. The etiology of ABS is controversial, and several synonyms have been reported in the literature, including ADAM (Amniotic Deformity, Adhesions, and Mutilations) complex, amnion rupture sequence, amniotic band sequence, amniotic band disruption complex, congenital ring constriction, constriction ring syndrome, transverse limb defects, annular constriction bands, aberrant tissue bands, Streeter’s dysplasia or syndrome, and early amnion rupture spectrum.[
Portal was the first to report this malformation in 1685.[
The present study reports a case of a newborn with ABS associated with double frontal encephalocele, which is a rare malformation.
CASE DESCRIPTION
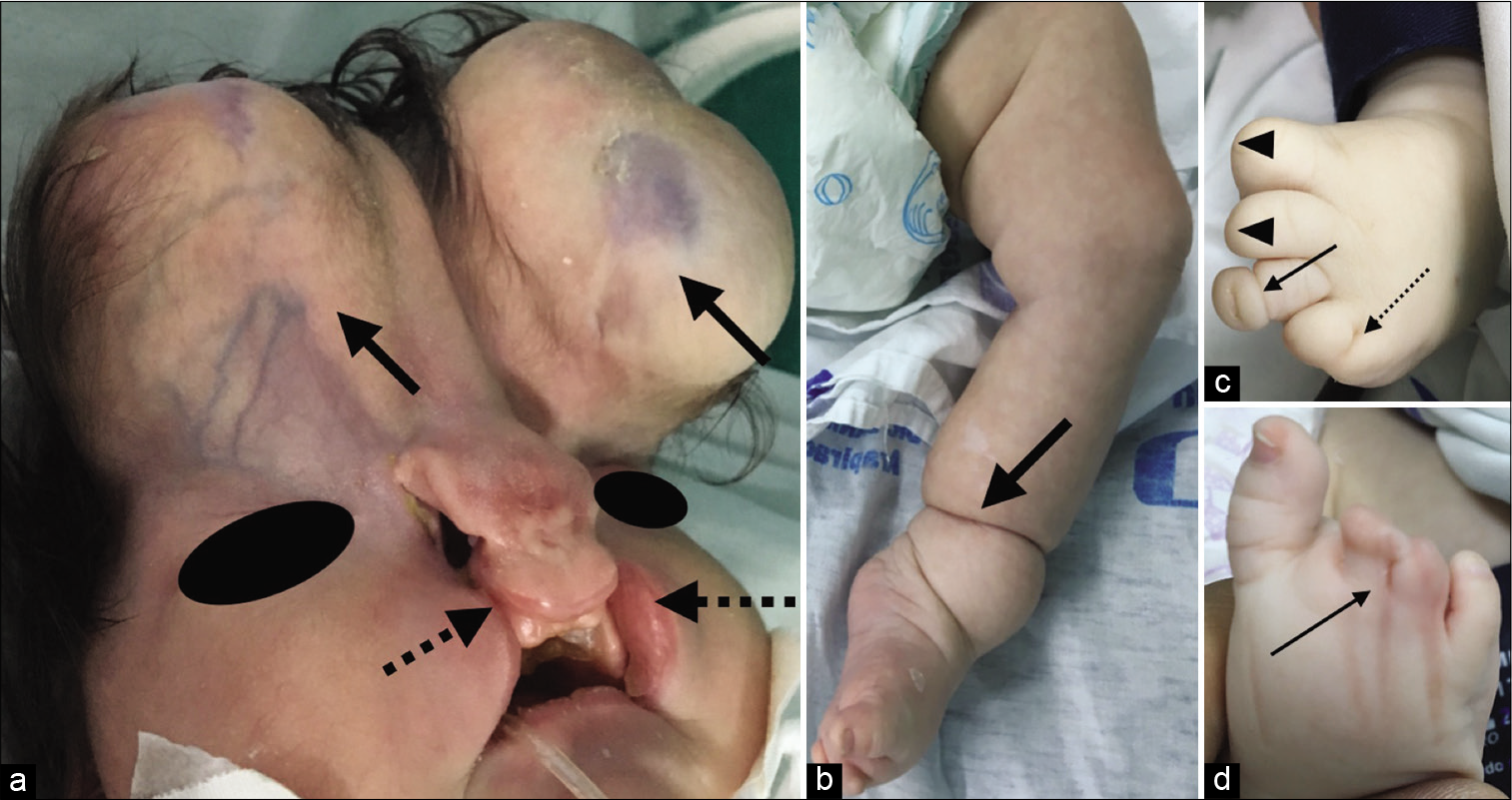
The mother was a 29-year-old primiparous woman with no history of infections during pregnancy, a consanguineous marriage, or exposure to teratogens. She was admitted to Santa Mônica Maternity School at gestation week 38; she underwent a cesarean section and delivered a female newborn who was well, with an APGAR scores were 8 and 9 at 1–5 min, respectively. Weight 3550 g, height 51 cm, non-measurable head circumference, and chest circumference 35 cm. The newborn had the following abnormalities: multiple craniofacial malformations such as bilateral cleft lip, hypertelorism, and bilateral frontal encephalocele [
Figure 1:
(a) Double frontal encephalocele (black arrow), bilateral complete cleft lip (dotted black arrow) and hypertelorism; (b) Left leg: constriction ring above ankle joints (black arrow); (c) Left foot: partial amputation of the 1st and 2nd fingers (black arrowheads), constriction ring of the 3rd finger (black arrow) and fenestrated syndactyly of the 4th and 5th fingers (dotted black arrow); (d) Right foot: fenestrated syndactyly of the 2nd, 3rd, and 4th fingers (black arrow).
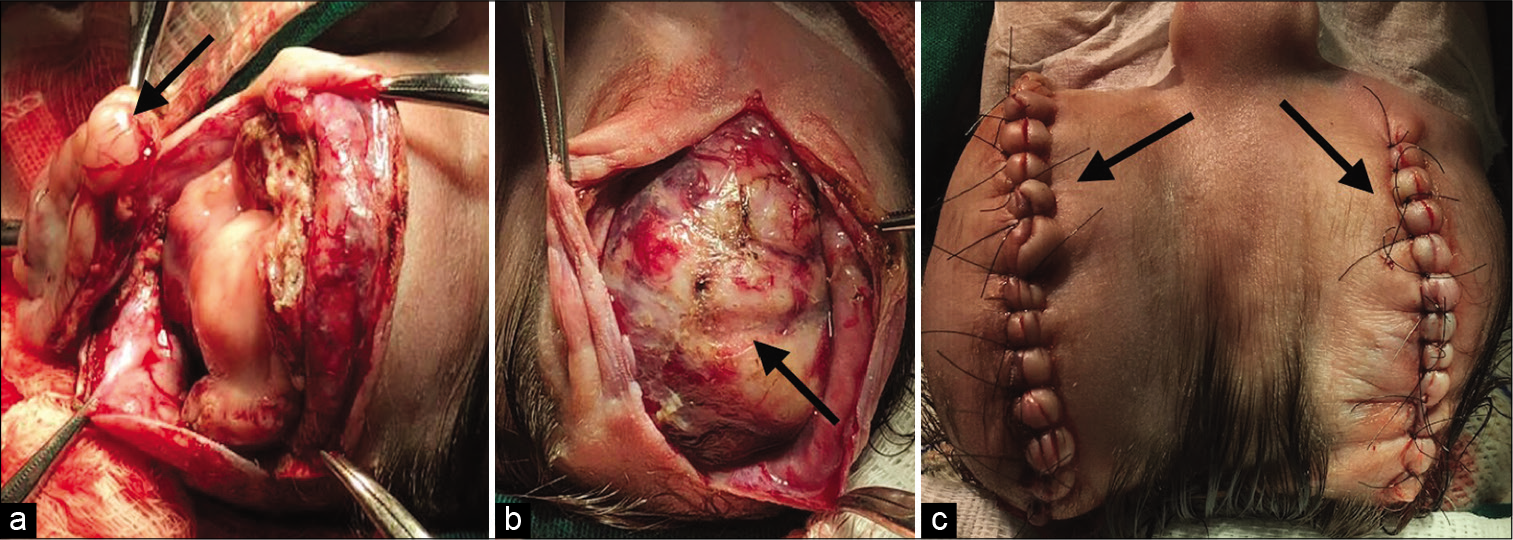
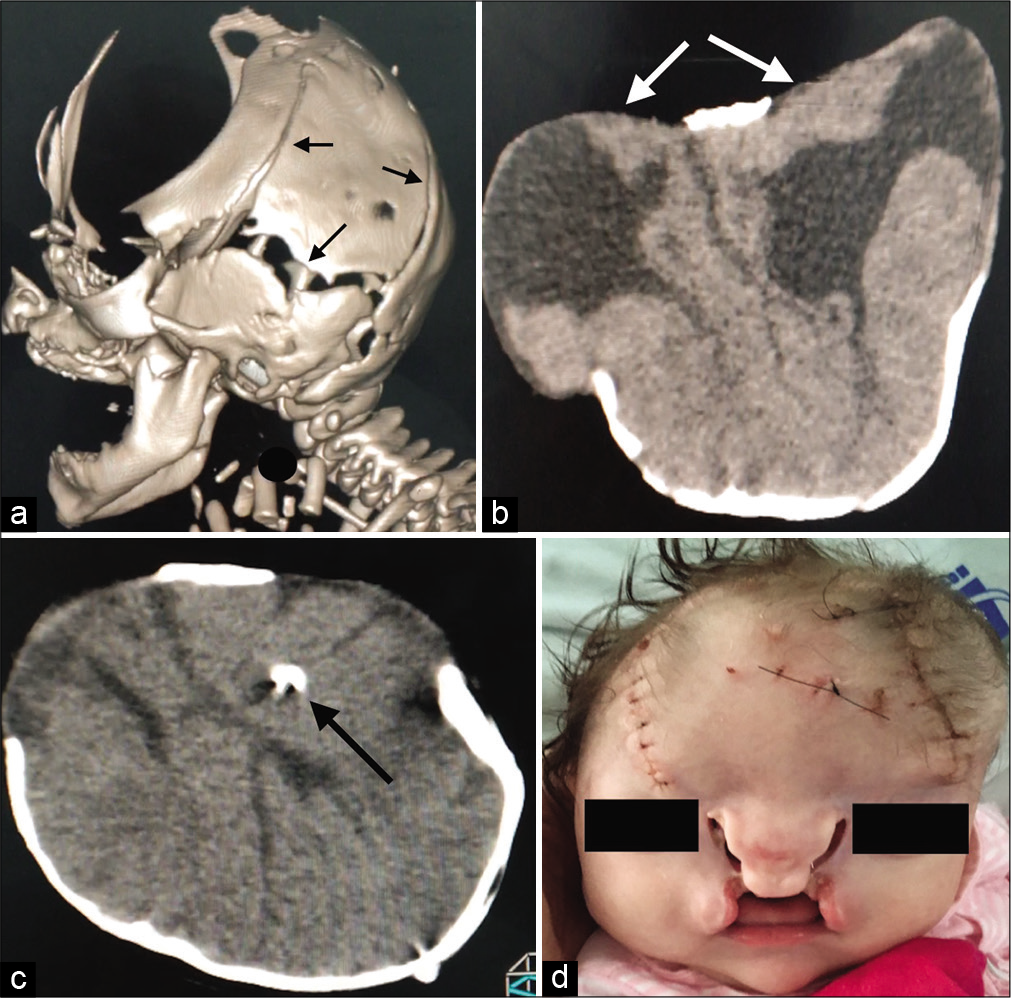
The patient underwent surgical repair of the double frontal encephaloceles (6 × 4 cm on the right and 6 × 5.5 cm on the left), with no complications [
Figure 3:
(a) and (b) Frontal cranial defect with open sutures (black arrows), without craniosynostosis showing two separate sacs with malformed neural tissue (white arrows): dysmorphic ventricle, open lip schizencephaly, lissencephaly spectrum, agenesis of the corpus callosum; (c) ventriculoperitoneal shunt placement (black arrow). (d) After shunt placement.
DISCUSSION
In an attempt to explain the etiopathogenesis of ABS, two theories have been proposed. The first is the intrinsic theory, proposed by George Streeter in 1930; this theory states that a dysfunction in embryogenesis would lead to imperfect histogenesis of the fetal tissue, resulting in the fibrous bands. However, it fails to explain most of the anomalies observed.[
Some risk factors associated with amniotic rupture include maternal abdominal injuries, surgical interventions before or during pregnancy, use of intrauterine devices, uterine malformation, collagen diseases (osteogenesis imperfecta and Ehlers-Danlos syndrome), drugs (clomiphene and contraceptives), and amniocentesis (chorionic villus biopsy).[
Other theories also try to explain the anomalies caused by ABS, such as the vascular disruption theory, proposed in 1987, according to which vascular damage during embryogenesis would lead to destruction of existing structures, thereby causing internal and external defects.[
A genetic basis has also been considered to explain these anomalies of ABS, theorizing that the cause could be a mutant gene, such as a human homolog of the Ds gene (“disorganization gene”) of mutant mice, which would cause a wide variety of anomalies.[
Some genetic syndromes involving cleft lip and palate can also present oral or facial fibrous bands. These include Van der Woude syndrome and popliteal pterygium syndrome, which involve IRF6 mutations, and Hay-Wells syndrome, with p63 mutations.[
According to Guzmán-Huerta et al.,[
In the present study, the rare craniofacial defect associated with ABS was double encephalocele, which is characterized by multiple neural tube defects of rare occurrence.[
The diagnosis of ABS is most often made on the basis of the clinical findings of anatomical abnormalities. Chromosomal analysis is usually normal.[
CONCLUSION
ABS may be associated with several anomalies ranging from the less severe defects such as constriction rings of the fingers to the most complex craniofacial malformations, as that reported in the present study. Double encephalocele in the presence of ABS is a rare condition, and in our case, it was accompanied by other existing anomalies (cleft lip, limb constriction rings, and amputations). Such conditions are severe, with high morbidity and mortality rates. Patients who survive such conditions require multidisciplinary monitoring to improve their quality of life.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
1. Askins G, Ger E. Congenital constriction band syndrome. J Pediatr Orthop. 1988. 8: 461-6
2. Burgess RC. Brachydactyly in acrosyndactyly. J Hand Surg Am. 1991. 16: 125-6
3. Chen H, Gonzalez E, Opitz JM, Reynolds JF. Amniotic band sequence and its neurocutaneous manifestations. Am J Med Genet. 1987. 28: 661-73
4. Cignini P, Giorlandino C, Padula F, Dugo N, Cafà EV, Spata A. Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenat Med. 2012. 6: 59-63
5. da Silva G, Cammarata SF, González-Coira M, Lacruz MA, Rendon B. Amniotic band syndrome: 3 case reports. Rev Chil Pediatr. 2008. 79: 172-80
6. Donnai D, Winter RM. Disorganisation: A model for early amnion rupture?. J Med Genet. 1989. 26: 421-5
7. Foulkes GD, Reinker K. Congenital constriction band syndrome: A seventy-year experience. J Pediatr Orthop. 1994. 14: 242-8
8. Goldfarb CA, Sathienkijkanchai A, Robin NH. Amniotic constriction band: A multidisciplinary assessment of etiology and clinical presentation. J Bone Joint Surg Am. 2009. 91: 68-75
9. González ZI, Padilla F. Complex of amniotic deformities, adhesions, mutilations: Endless debate. Bol Med Hosp Infant Mex. 2015. 72: 159-68
10. Guzmán-Huerta ME, Muro-Barragán SA, Acevedo-Gallegos S, Velázquez-Torres B, Gallardo-Gaona JM, Ramírez-Calvo JA. Amniotic band sequence: Prenatal diagnosis, phenotype descriptions, and a proposal of a new classification based on morphologic findings. Rev Invest Clin. 2013. 65: 300-6
11. Hunter AG, Seaver LH, Stevenson RE. Limb-body wall defect. Is there a defensible hypothesis and can it explain all the associated anomalies? Am J Med Genet A 2011. ;. 155: 2045-59
12. Kulkarni ML, Gopal PV. Amniotic band syndrome. Indian Pediatr. 1990. 27: 471-6
13. Lobato G. Amniotic band: Sonographic findings and correlations etiopathogenic. Femina. 2008. 36: 159-63
14. Montgomery WF. Observation on the spontaneous amputation of the limbs of the fetus in utero, with an attempt to explain the occasional cause of its production. Dublin Med Chem Sci J. 1832. 1: 140-4
15. Nakatsu T, Uwabe C, Shiota K. Neural tube closure in humans initiates at multiple sites: Evidence from human embryos and implications for the pathogenesis of neural tube defects. Anat Embryol (Berl). 2000. 201: 455-66
16. Pardini AG, Santos MA, Freitas AD. Congenital constriction bands. Acta Ortop Bras. 2001. 9: 3-10
17. Portal P.editors. La Pratique des Accouchements Soutenue d’un Grand Nombre D’observations. Paris: Gabriel Martin; 1685. p.
18. Rebello CM, Leone CR, Zugaib M, Ramos JL, Gonzáles CH. Amniotic band syndrome. Pediatria (Säo Paulo). 1990. 11: 26-9
19. Streeter GL. Focal deficiencies in fetal tissues and their relation to intrauterine amputation. Contrib Embryol Carnegie Inst. 1930. 22: 1-44
20. Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands: Associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965. 91: 65-75
21. van Allen MI, Kalousek DK, Chernoff GF, Juriloff D, Harris M, McGillivray BC. Evidence for multi-site closure of the neural tube in humans. Am J Med Genet. 1993. 47: 723-43
22. Walter JH, Goss LR, Lazzara AT. Amniotic band syndrome. J Foot Ankle Surg. 1998. 37: 325-33
23. Yhoshu E, Dash V, Bawa M. Double encephalocele: An unusual presentation. J Pediatr Neurosci. 2018. 13: 264-6