- Departments of Neurosurgery Centro Hospitalar e Universitário de Lisboa Central, Rua José António Serrano, Lisboa, Lisbon, Portugal.
- Departments of Pathological Anatomy, Centro Hospitalar e Universitário de Lisboa Central, Rua José António Serrano, Lisboa, Lisbon, Portugal.
Correspondence Address:
Ricardo Malcata Nogueira
Departments of Pathological Anatomy, Centro Hospitalar e Universitário de Lisboa Central, Rua José António Serrano, Lisboa, Lisbon, Portugal.
DOI:10.25259/SNI_352_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ricardo Malcata Nogueira, Luis Santos Cardoso, Lino Fonseca, Pedro Branco, Miguel Correia, Pedro Roque, Catarina Araújo. An uncommon intramedullary tumor: Primary medullary cone melanoma. 18-Jul-2020;11:200
How to cite this URL: Ricardo Malcata Nogueira, Luis Santos Cardoso, Lino Fonseca, Pedro Branco, Miguel Correia, Pedro Roque, Catarina Araújo. An uncommon intramedullary tumor: Primary medullary cone melanoma. 18-Jul-2020;11:200. Available from: https://surgicalneurologyint.com/surgicalint-articles/10144/
Abstract
Background: Melanoma is the third most common primary tumor to metastasize to the central nervous system (CNS). However, primary CNS melanoma is very rare, and primary intramedullary melanoma is even less frequently encountered, with only 27 cases published in the literature. There are no pathognomonic imaging characteristics, therefore, the diagnosis must be confirmed immunohistologically and the preferred treatment is the gross total resection.
Case Description: A 68-year-old male presented with low back pain of 2 months duration, and 1 week of urinary retention/anal sphincter incontinence. The neurologic examination revealed bilateral paraparesis (3/5 level) with bilateral Babinski signs, and a T10–T11 pin level. The lumbar CT-Scan showed a hyperdense intramedullary tumor arising from the conus medullaris. The patient underwent a D12–L2 laminectomy with myelotomy for gross-total tumor resection. Postoperatively, he regained motor function but the urinary incontinence remained unchanged. The diagnosis of a primary malignant melanoma was confirmed both histopathologically and immunohistochemically (e.g., staining revealed positive immunoreactivity for S100 protein and Melan A).
Conclusions: Primary intramedullary spinal melanoma is very rare, and the diagnosis must be biopsy/operatively confirmed. Whether gross total resection is feasible depends on the extent of tumor infiltration of the cord/ adherence as well as the potential for clinical deterioration with overly aggressive removal.
Keywords: Intramedullary tumor, Medullary cone, Melanoma
INTRODUCTION
Primary CNS melanoma is rare and accounts for only 1% of all melanomas according to the World Health Organization classification.[
Patients present with symptoms reflecting the level of the intramedullary lesion. Complaints typically include somatic pain, myelopathy/motor deficits, sensory changes/pin levels, and sphincter dysfunction.[
Here, we present a case of an intramedullary primary melanoma in a 68-year-old male who presented with paraparesis and a T10/T11 sensory level who did well following gross total tumor excision.
CASE REPORT
A 68-year-old man presented with lumbar pain of 2 months duration that progressed to paraparesis with sphincter incontinence over the last week.
The neurologic examination confirmed the lower extremity motor strength of 3/5, bilateral Babinski signs, and a relative pin level at T10.
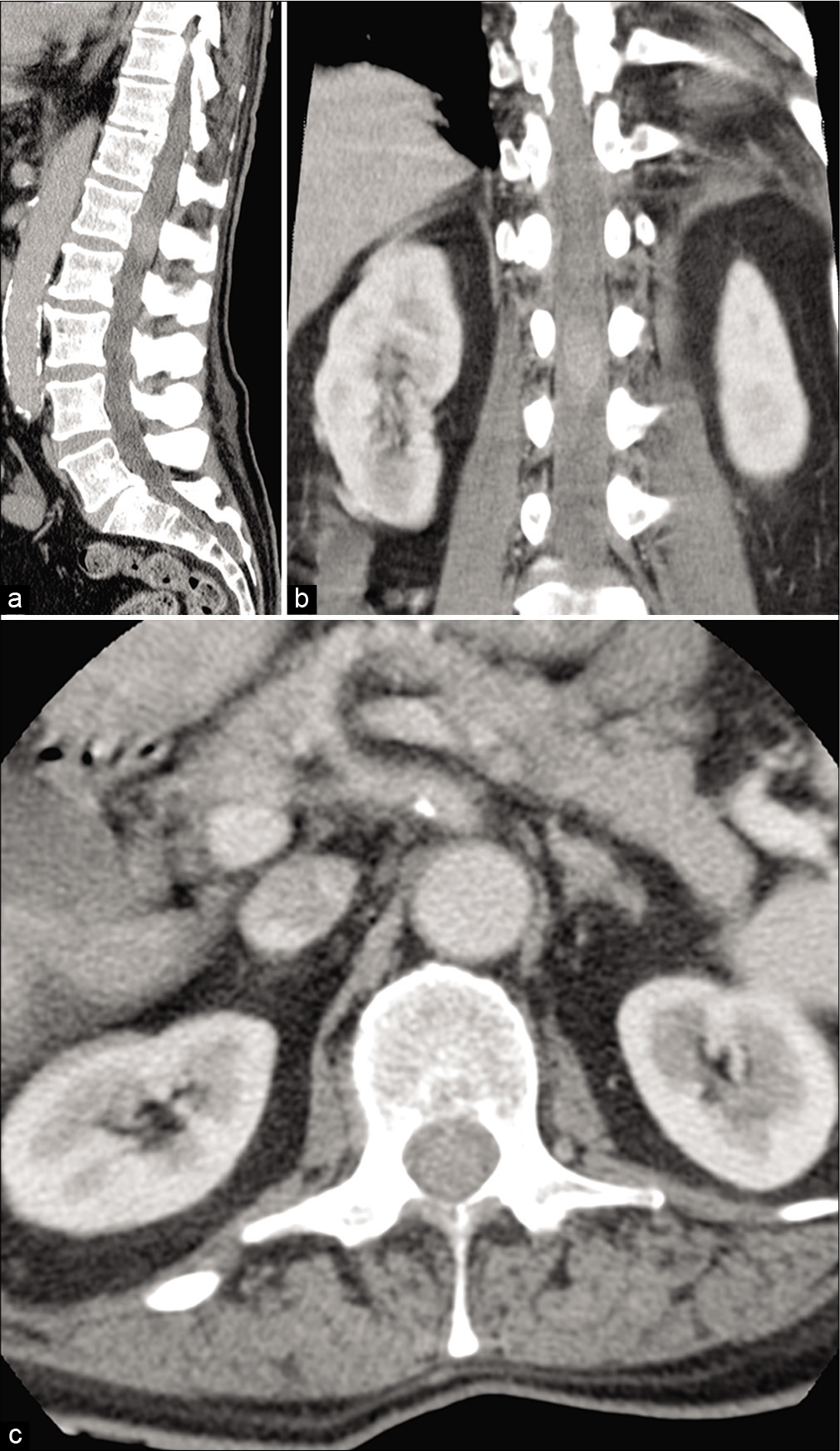
The lumbar CT-scan [
Figure 1:
(a) Lumbosacral computed tomography showing a central hyperdense image at L1 level suggestive of a intradural lesion occupying almost all the canal with no extension to the foramen and with no bone lesion associated; sagittal plane, (b) pre-operative, coronal plane (c) pre-operative, axial plane.
Through a D12–L2 laminectomy and midline myelotomy, tumor was excised at the conus medullaris level; it was readily dissected and full resected exhibiting an excellent cleavage plane. It was soft, black, and had an intratumoral hematoma. Intraoperatively, there were no changes in the in the motor evoked potentials or somatosensory evoked potential. Watertight dural closure was achieved, and a laminoplasty was performed.
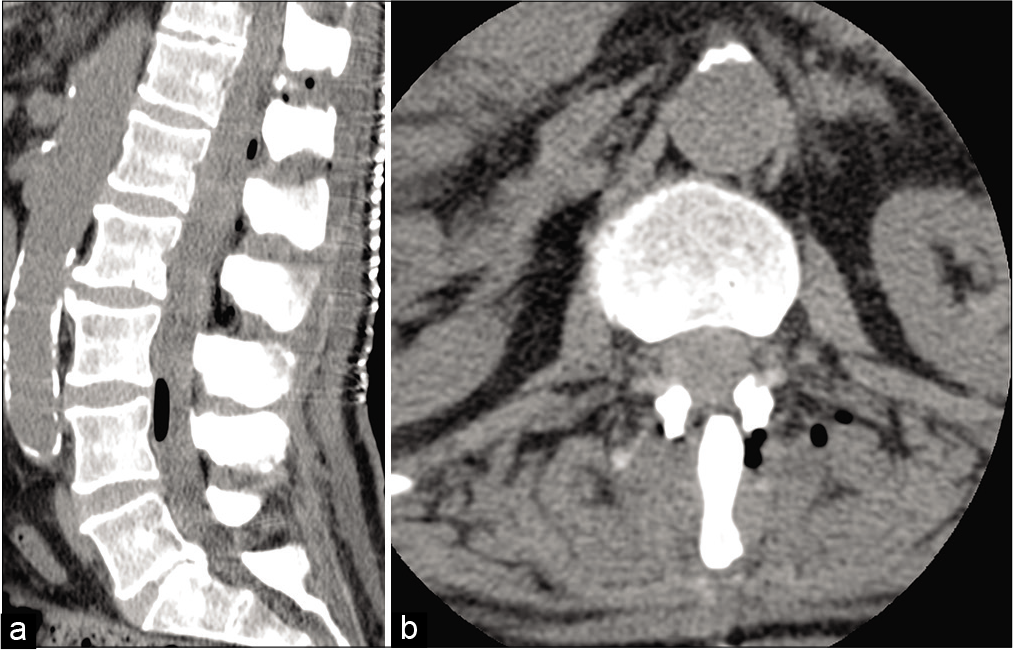
Postoperatively, the patient partially recovered muscular strength, the pain disappeared and he started a rehabilitation program, but did not regain urinary continence [
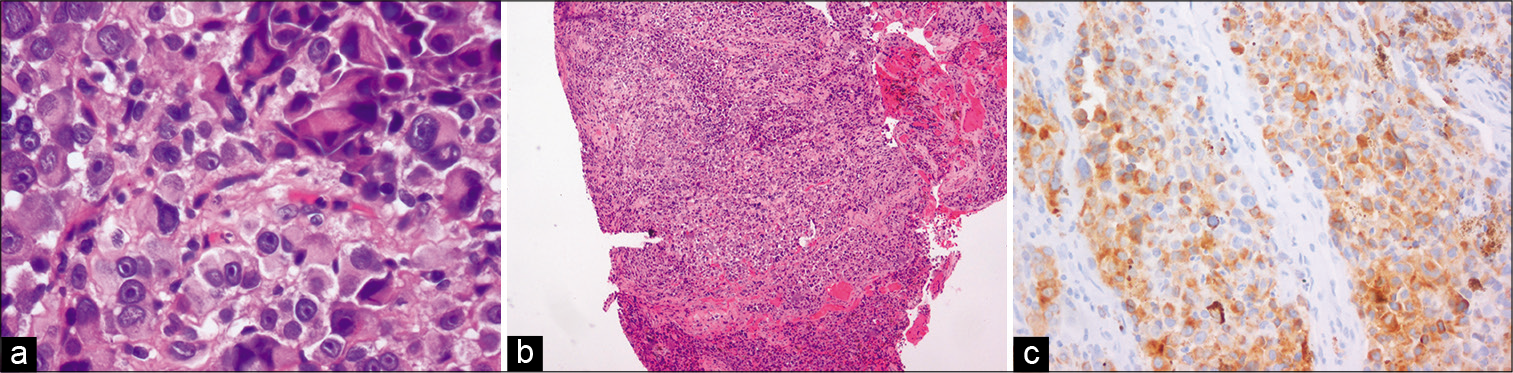
Notably, a positron emission tomography (PET)-SCAN, with tumor markers, ophthalmological, and dermatological examinations were performed, but no other primary tumor was identified. Further, primary malignant melanoma was confirmed with histopathology and immunohistochemical (e.g., positive immunoreactivity for S100 protein and Melan A) [
Figure 3:
(a) Hematoxylin and eosin stain ×40 - large, irregular cells with moderate pleomorphism, with hyper-chromatic nucleus and prominent nucleoli visible. Some binucleated cells are also identified, (b) Hematoxylin and eosin stain ×4 - small magnification of the biopsy fragments, (c) Melan-A 20x - neoplasic cells with cytoplasmic marking.
The patient refused radiation therapy and chemotherapy and was lost to follow-up at 3 months.
DISCUSSION
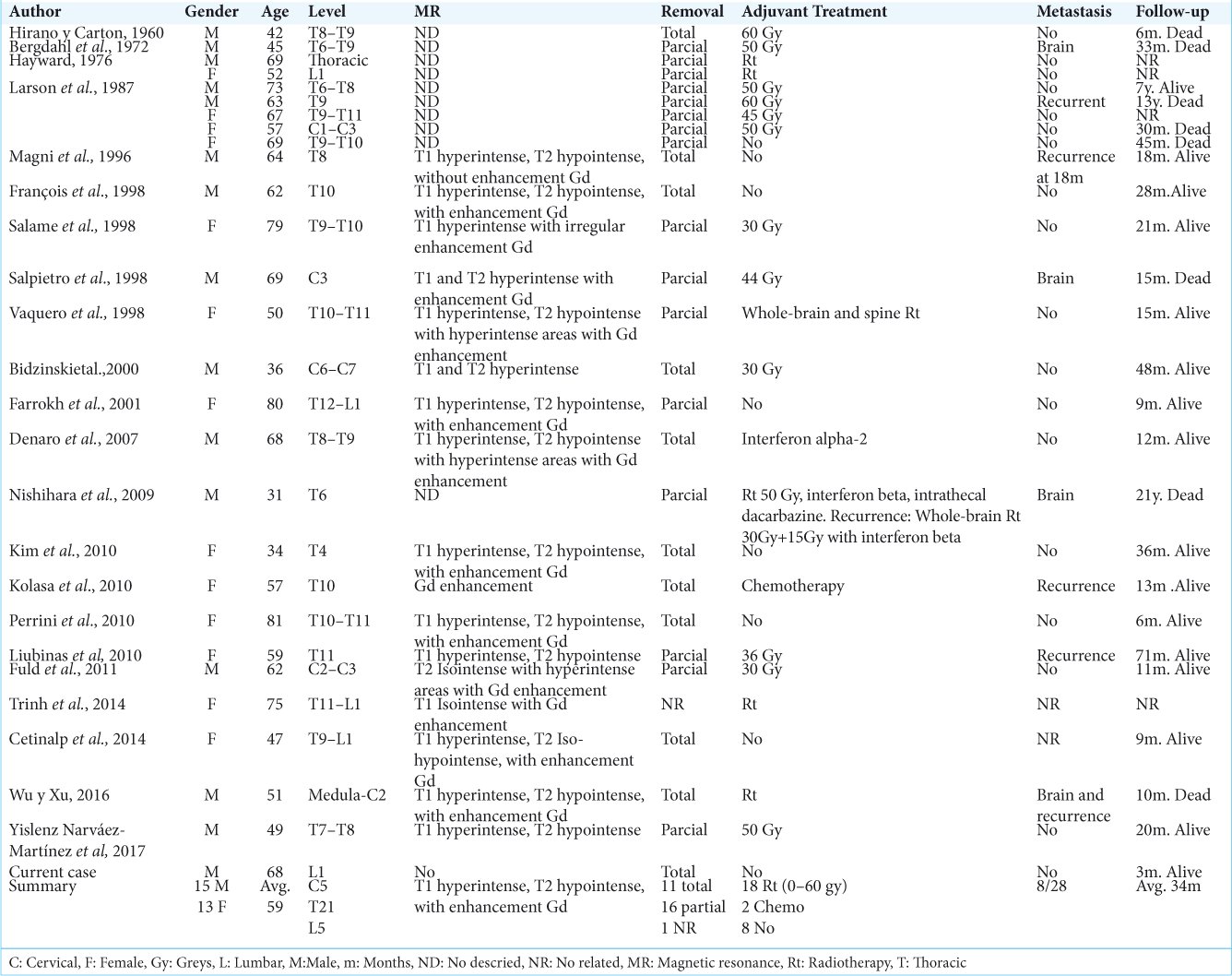
The case presented was remarkable because the melanoma presented as an intramedullary lesion in the conus. Only, 27 similar intramedullary melanoma cases can be found in the literature [
Although MR is study of choice, here it could not be done due to the patient’s pacemaker. The CT however showed a hyperdense lesion in the conus, suggestive of hemorrhage.[
As the diagnosis must be pathologically and immunohistologically confirmed, the patient in this study underwent gross total excision; this is preferred over biopsy or partial excision where feasible.[
Postoperatively, it is imperative to carry out dermatological, ophthalmological, and gastrointestinal examinations, along with a PET scanning to determine whether the intramedullary mass was primary or metastatic.[
Postoperative radiotherapy and/or chemotherapy are often recommended but there is no, clear evidence regard their efficacy.[
CONCLUSION
Primary intramedullary spinal melanoma is very rare and unpredictable pathology and surgery remains the first choice of treatment with gross total resection utilizing microsurgical techniques and intraoperative monitoring.[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chatterjee R, Nascimento FA, Heck KA, Ropper AE, Sabichi AL. Primary spinal cord melanoma-an uncommon entity. Can J Neurol Sci. 2019. 46: 348-50
2. Iga T, Iwanami A, Funakoshi T, Mikami S, Tsuji O, Nagoshi N. Multifocal primary melanoma of the cervical spinal cord successfully treated by tumorectomy: A case report. Spinal Cord Ser Cases. 2018. 4: 24-
3. Liang W, Yao N, Fang J, Yang J, Xu Y. Clinical features and long-term outcomes of primary spinal malignant melanoma: A single center experience. J Neurooncol. 2017. 135: 513-9
4. Narváez-Martínez Y, Ossa N, López-Martos R, Cohn-Reinoso C, Castellví-Juan M, Martin-Ferrer S. Intramedullary primary melanoma: Case report and literature review. Neurocirugia. 2017. 28: 190-6
5. Sharm A, Sinha VD. Primary spinal cord melanoma of intradural extramedullary origin. J Neurosci Rural Pract. 2019. 10: 522-5
6. Wu L, Xu Y. Primary spinal intramedullary malignant melanoma involving the medulla oblongata. Spine J. 2016. 16: 188-91
7. Wuerdeman M, Douglass S, Abda RB, Krasnokutsky CM. A rare case of primary spinal cord melanoma. Radiol Case Rep. 2018. 13: 424-6
8. Zhang M, Liu R, Xiang Y, Mao J, Li G, Ma R. Primary spinal cord melanoma: A case report and a systemic review of overall survival. World Neurosurg. 2018. 114: 408-20