- Department of Neurosurgery, Hospital Clínica Kennedy, Guayaquil, Ecuador
- Department of Medicine, Universidad de Especialidades Espíritu Santo, Samborondon, Ecuador,
- Department of Neurosurgery, Clinical Hospital, Universidad de la Republica, Montevideo, Uruguay, Guayaquil, Ecuador
- Department of Neurosurgery, Clínica Guayaquil, Guayaquil, Ecuador
- Department of Medicine, Universidad Católica de Santiago de Guayaquil, Guayaquil, Ecuador,
- Department of Neurosurgery, National Institute of Neurology and Neurosurgery Manuel Velasco Suarez, México City, Mexico.
Correspondence Address:
Paula Gabriela Veintimilla, Department of Medicine, Universidad de Especialidades Espíritu Santo, Samborondon, Ecuador.
DOI:10.25259/SNI_650_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jimmy Achi1, Paula Gabriela Veintimilla2, Fernando Martinez3, Giuliano Faggioni4, Karolina Achi Zúñiga5, Xavier Wong Achi6. Anconeus epitrochlearis muscle resulting in cubital nerve compressive neuropathy: Two case reports. 27-Oct-2023;14:381
How to cite this URL: Jimmy Achi1, Paula Gabriela Veintimilla2, Fernando Martinez3, Giuliano Faggioni4, Karolina Achi Zúñiga5, Xavier Wong Achi6. Anconeus epitrochlearis muscle resulting in cubital nerve compressive neuropathy: Two case reports. 27-Oct-2023;14:381. Available from: https://surgicalneurologyint.com/surgicalint-articles/12613/
Abstract
Background: The anconeus epitrochlearis muscle is an anatomical variant prevalent in amphibians but unusual in humans. In favorable cases, this muscle provides protection to the cubital nerve but can result in neuropathy due to compression of the cubital nerve.
Case Description: We present two cases with different clinical manifestations but both did not respond to conservative treatment. We opted for a surgical decompression where the anconeus epitrochlearis muscle was found intraoperatively, and the muscle fibers were dissected.
Conclusion: Considering the presence of the muscle variant is the key point to intraoperatively achieve a complete dissection of the muscle fibers of the anconeus epitrochlearis muscle variant and obtain the decompression of the cubital nerve with satisfactory postoperative results.
Keywords: Anatomical variant, Anconeus epitrochlearis muscle, Compression, Cubital nerve, Neuropathy
INTRODUCTION
Compressive neuropathy of the cubital nerve is the second most common compression due to entrapment after carpal tunnel syndrome. In common situations, cubital nerve compression can be static, between the cubital tunnel retinaculum and Osborne’s ligament, specifically between the two heads of the flexor carpi ulnaris, or dynamic compression when the nerve has an inconsistent location outside the ulnar groove. The ulnar nerve sensory innervates the anterior and posterior surfaces of the fifth finger and the ulnar half of the fourth finger.[
ILLUSTRATIVE CASES
Case 1
A 14-year-old female patient who works in high effort tasks comes for examination due to bilateral paresis of the hands. Physical exploration showed severe hypertrophy in the hypothenar eminences of both hands and decreased articular strength in metacarpophalangeal flexion and interphalangeal extension. An electrical study showed a drop of conduction potentials at the elbow region bilaterally with predominance on the left side, which confirms the diagnosis of bilateral ulnar compression at the level of the epitrocholecranial canal. The patient was submitted to bilateral surgical decompression of the ulnar nerve. Intraoperatively, muscle fibers were recognized at the superior border of the insertion of the flexor carpi ulnaris corresponding to the anatomical anomalous variant anconeus epitrochlearis [
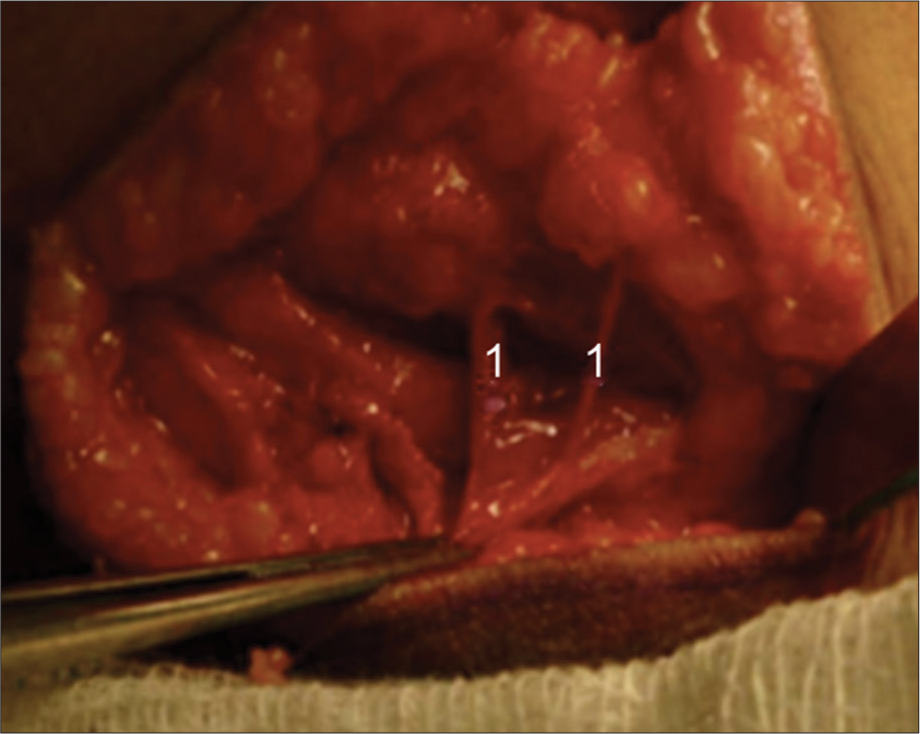
Figure 1:
Cubital tunnel, left side. In the dissection of the flexor carpi ulnaris, is evidenced muscle fascicles of the anconeus epitrochlearis.[
Case 2
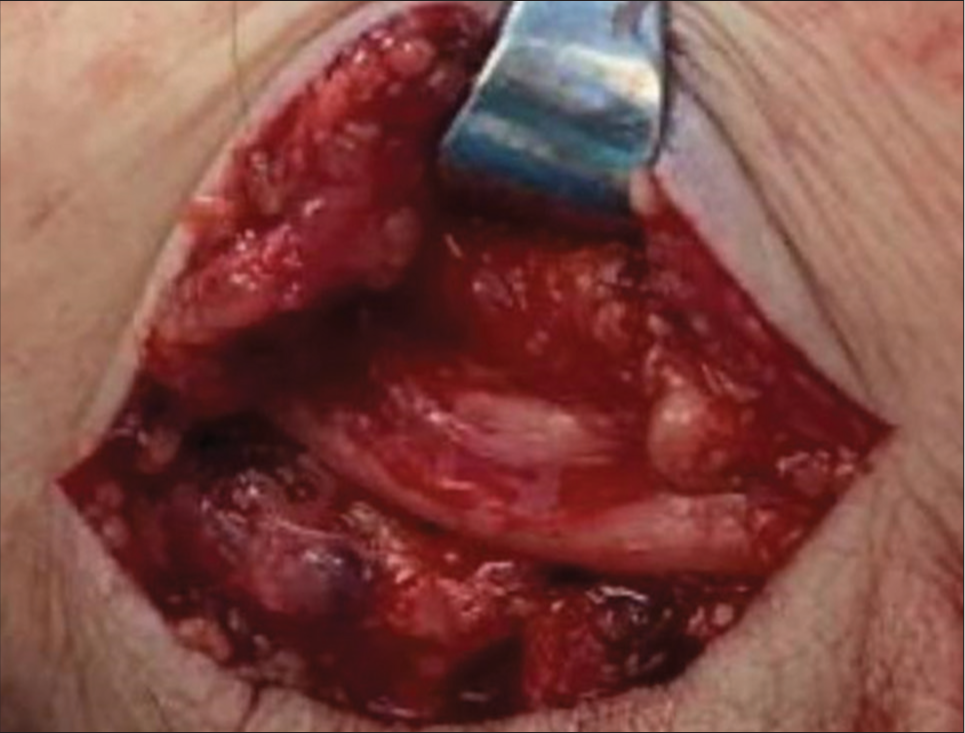
A 53-year-old male patient comes to the consultation for a clinical picture of paresthesia in the right hand with hyperalgesia with 3 months of evolution after a lumbar narrow lumbar canal surgery. The patient mentioned that his pain increased as an electric shock. Electromyography confirms the diagnosis of cubital nerve compression. There was no response to conservative treatment, so surgery was indicated. Intraoperatively, muscle fibers from the anconeus epitrochlearis muscle variant were identified compressing the cubital nerve, and they were liberated [
DISCUSSION
Entrapment neuropathies are pathologies that are frequently seen in the neurosurgeon’s medical office, among which ulnar nerve entrapment neuropathy is the second most common neuropathy.[
Studies in various countries around the world have reported cases of neuropathy due to ulnar nerve entrapment secondary to the presence of the anconeus epitrochlearis muscle.[
CONCLUSION
Despite its low prevalence, the presence of epitrochlear anchorius muscle should be considered by doctors when the patient does not recover from conservative treatment. Considering the possibility of finding the muscle variable, it is possible to act efficiently and quickly, being able to obtain the best surgical result without less motor deficit due to compression in the postsurgical period of the patients.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Afshar A. Ulnar tunnel syndrome due to an aberrant muscle. Arch Iran Med. 2015. 18: 58-9
2. Andrews K, Rowland A, Pranjal A, Ebraheim N. Cubital tunnel syndrome: Anatomy, clinical presentation, and management. J Orthop. 2018. 15: 832-6
3. Bachoura A, Jacoby SM. Ulnar tunnel syndrome. Orthop Clin North Am. 2012. 43: 467-74
4. Boero S, Sénès FM, Catena N. Pediatric cubital tunnel syndrome by anconeus epitrochlearis: A case report. J Shoulder Elbow Surg. 2009. 18: e21-3
5. Burahee AS, Sanders AD, Shirley C, Power DM. Cubital tunnel syndrome. EFORT Open Rev. 2021. 6: 743-50
6. Cambon-Binder A. Ulnar neuropathy at the elbow. Orthop Traumatol Surg Res. 2021. 107: 102754
7. Cortes Tronch V, Aguilella L. Anconeus epitrochlearis muscle. A infrequent cause of cubital neuropathy of the elbow. Rev Esp Reum Enfeerm Osteoartic. 2017. 52: 163-6
8. Dahners LE, Wood FM. Anconeus epitrochlearis, a rare cause of cubital tunnel syndrome: A case report. J Hand Surg Am. 1984. 9: 579-80
9. Kim N, Stehr R, Matloub HS, Sanger JR. Anconeus epitrochlearis muscle associated with cubital tunnel syndrome: A case series. Hand (N Y). 2019. 14: 477-82
10. Martinez F, Medici C, Algorta M. Cubital tunnel syndrome secondary to anconeus-epitrochlearis muscle: Case report. Rev Arg Anat Online. 2012. 3: 43-6
11. Maslow JI, Johnson DJ, Block JJ, Lee DH, Desai MJ. Prevalence and clinical manifestations of the anconeus epitrochlearis and cubital tunnel syndrome. Hand (N Y). 2020. 15: 69-74
12. Morgenstein A, Lourie G, Miller B. Anconeus epitrochlearis muscle causing dynamic cubital tunnel syndrome: A case series. J Hand Surg Eur Vol. 2016. 41: 227-9
13. Schafer ES, Symington J, Brice TH, editors. Quain’s Elements of Anatomy. Myology. London, UK: Longman Green and Co; 1923. 4: 131 Part II