- Department of Neurological Surgery, University Hospitals Cleveland Medical Center, Cleveland, Ohio, United States.
- Department of Neurosurgery, Ascension St Mary’s Hospital, Saginaw, Michigan, United States.
Correspondence Address:
Theresa A. Elder
Department of Neurosurgery, Ascension St Mary’s Hospital, Saginaw, Michigan, United States.
DOI:10.25259/SNI_732_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Theresa A. Elder1, Joseph G. Adel2. Aneurysmal subarachnoid hemorrhage, a presentation of metastatic carcinoma: A case report and review of the literature. 08-Apr-2021;12:143
How to cite this URL: Theresa A. Elder1, Joseph G. Adel2. Aneurysmal subarachnoid hemorrhage, a presentation of metastatic carcinoma: A case report and review of the literature. 08-Apr-2021;12:143. Available from: https://surgicalneurologyint.com/surgicalint-articles/10700/
Abstract
Background: Neoplastic cerebral aneurysms related to metastatic processes are exceptionally rare and carry a dismal prognosis. Only four previous reports exist of neoplastic aneurysms secondary to metastatic adenocarcinoma, all of which were found to be lung cancer in origin. We present the fifth reported metastatic adenocarcinomatous cerebral aneurysm, and the first case is secondary to a non-lung cancer primary.
Case Description: The patient presented with complaining of headache and was found to have a large right-sided intraparenchymal hemorrhage and smaller left-sided hemorrhage on head CT, and CTA revealed a vascular pouch in the region of the hemorrhage. The patient showed sudden neurologic decline, and repeat imaging revealed enlargement of the hematoma with significant brain compression. The patient underwent emergent angiography revealing a distal cortical middle cerebral artery aneurysm, suspicious for mycotic etiology, which was treated through microsurgical excision at the time of hematoma evacuation. The aneurysm specimen was sent for cultures and pathology, revealing the diagnosis of metastatic non-small-cell carcinoma. Further inpatient workup did not reveal the primary neoplastic source.
Conclusion: Although diagnostic workup should search for more common pathologic mimics than metastatic neoplastic cerebral aneurysms, clinicians must be able to recognize and expeditiously treat this devastating lesion. Further investigation and analysis of treatment options are necessary to better understand this rare pathology and improve patient outcomes.
Keywords: Adenocarcinoma, Aneurysm, Case report, Intracranial hemorrhage, Metastatic
INTRODUCTION
Cerebral aneurysms secondary to metastatic neoplastic processes are exceedingly rare, with less than 100 cases reported in the literature.[
We present a patient with no known cancer history, who presented with aneurysmal hemorrhage, initially presumed to be mycotic in etiology due to the lesion’s location and morphology. Intraoperative pathology, however, revealed non-small-cell adenocarcinoma. Imaging of the chest, abdomen, and pelvis did not reveal a culprit lesion, rendering lung adenocarcinoma an unlikely source and leaving breast adenocarcinoma as the leading primary diagnosis among adenocarcinoma of other distant sites. This case would represent the first reported case of metastatic aneurysm secondary to adenocarcinoma of the breast or of any non-lung origin.
CASE SUMMARY
Clinical presentation
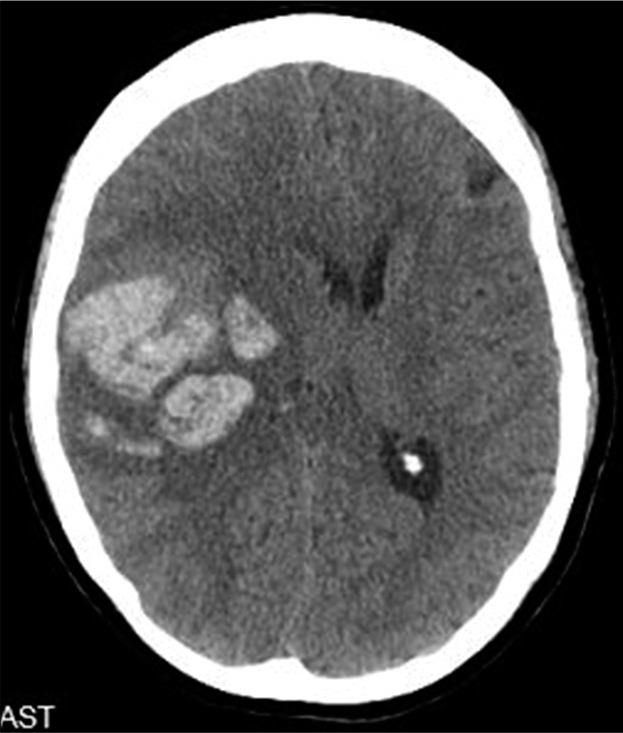
A 67-year-old right-handed female presented to the hospital with a headache which began the day prior. Head CT revealed a 4.7 × 3.8 × 2.2 cm right parietal intraparenchymal hemorrhage and 1 cm left parietal intraparenchymal hemorrhage [
Intraoperative course
The patient was taken emergently for angiography with the intent to identify and treat the underlying vascular malformation if amenable to endovascular treatment, before craniotomy for hematoma evacuation. Angiogram revealed a distal cortical middle cerebral artery (MCA) fusiform aneurysm, raising suspicion for mycotic etiology given the location [
Histopathology and post-operative course
Given the suspicion for mycotic aneurysm, a transesophageal echocardiogram was obtained and was negative for any evidence of endocarditis or atrial myxoma. Final intraoperative cultures and blood cultures were negative for any infectious process. Head CTs demonstrated small contralateral hemorrhage without evidence of vascular pathology or metastatic disease on cerebral angiography or MRI.
Pathology was consistent with metastatic non-small-cell adenocarcinoma within the aneurysmal wall, with immunohistochemistry staining positive for CK7 and negative for CK 5/6, CK 20, TTF-1, and p63. Given these findings, oncology was consulted, and CT of the chest, abdomen, and pelvis was obtained and was negative for a malignancy source. Further workup was planned once the patient improved clinically, including PET scan to determine the location of the underlying malignancy. The patient recovered neurologically; however, she developed pneumonia and sepsis 2 weeks later, and the family elected hospice care.
DISCUSSION
Given the rarity of neoplastic cerebral aneurysms, there is an overall lack of understanding of the pathophysiology involved in their formation. Multiple theories have been postulated regarding the cause of vessel damage that leads to the formation of such aneurysms.[
While lung and breast carcinoma are the most common sources of metastatic brain tumors, there are no reported cases of metastatic cerebral aneurysms secondary to breast cancer or any non-lung origin. Of the seven existing cases, secondary to lung cancer, four were confirmed on histopathology, and the remainder were presumed based on active lung cancer lesions.[
Given the trend toward poor outcomes, awareness and prompt recognition of this potential diagnosis are critical. Similar to mycotic aneurysms, neoplastic aneurysms are generally small, fusiform, and peripherally located. They are best detected on angiography but may only be identifiable by delayed contrast washout in the arterial phase and/or decreased flow in the venous phase.[
There is a shortage of data on the treatment and outcomes of these lesions, with a lacking consensus on optimal management. Of the seven reported neoplastic lung cancer aneurysms, only one patient achieved a good functional outcome (at 6 months).[
CONCLUSION
Neoplastic cerebral aneurysms are rare but devastating lesions with the potential to rupture and carry significant morbidity and mortality risk. Clinicians must be aware of this potential aneurysm etiology and able to promptly conduct the appropriate diagnostic workup for such lesions as well as their pathologic mimics, especially when endovascular treatment is utilized which eliminates the benefit of pathology diagnosis. Further investigation of treatment options and outcomes will allow for better understanding of the underlying pathophysiology behind neoplastic aneurysm formation and may ultimately improve outcomes for these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ashalatha R, Moosa A, Gupta AK, Manohar SR, Sandhyamani S. Cerebral aneurysms in atrial myxoma: A delayed, rare manifestation. Neurol India. 2005. 53: 216-8
2. Gliemroth J, Nowak G, Kehler U, Arnold H, Gaebel C. Neoplastic cerebral aneurysm from metastatic lung adenocarcinoma associated with cerebral thrombosis and recurrent subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1999. 66: 246-7
3. Ho KL. Neoplastic aneurysm and intracranial hemorrhage. Cancer. 1982. 50: 2935-40
4. Kochi N, Tani E, Yokota M, Nakaya Y. Neoplastic cerebral aneurysm from lung cancer. Case report. J Neurosurg. 1984. 60: 640-3
5. Murata J, Sawamura Y, Takahashi A, Abe H, Saitoh H. Intracerebral hemorrhage caused by a neoplastic aneurysm from small-cell lung carcinoma: Case report. Neurosurgery. 1993. 32: 124-6
6. Nomura R, Yoshida D, Kim K, Kobayashi S, Teramoto A. Intracerebral hemorrhage caused by a neoplastic aneurysm from pleomorphic lung carcinoma. Neurol Med Chir (Tokyo). 2009. 49: 33-6
7. Noterman J, Verhest A, Baleriaux D, Brotchi J. A ruptured cerebral aneurysm from choriocarcinomatous origin-a case report and a review. Neurosurg Rev. 1989. 12: 71-4
8. Omofoye OA, Barnett R, Lau W, Trembath D, Jordan JD, Sasaki-Adams DM. Neoplastic cerebral aneurysm from metastatic nonsmall cell lung carcinoma: Case report and literature review. Neurosurgery. 2018. 83: E221-5
9. Radoi MP, Stefanescu F, Arsene D. Brain metastases and multiple cerebral aneurysms from cardiac myxoma: Case report and review of the literature. Br J Neurosurg. 2012. 26: 893-5
10. Sokolowski JD, Guilliams EL, Diaz M, Wildeman ME, Nguyen JH, Gish DS. Neoplastic cerebral aneurysm from metastatic lung adenocarcinoma with neuroendocrine features. World Neurosurg. 2019. 122: 155-60
11. Zheng J, Zhang J. Neoplastic cerebral aneurysm from metastatic tumor: A systematic review of clinical and treatment characteristics. Clin Neurol Neurosurg. 2015. 128: 107-11