- Department of Neurosurgery, IRCCS, Istituto Ortopedico Galeazzi, Milan, Italy.
- Department of Functional Neurosurgery, IRCCS Istituto Neurologico Carlo Besta, Milan, Italy.
Correspondence Address:
Guglielmo Iess
Department of Neurosurgery, IRCCS, Istituto Ortopedico Galeazzi, Milan, Italy.
DOI:10.25259/SNI_876_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Edvin Zekaj1, Guglielmo Iess2, Domenico Servello1. Anterior cervical spine surgical complications: Safety comparison between teacher and student. 03-Feb-2021;12:43
How to cite this URL: Edvin Zekaj1, Guglielmo Iess2, Domenico Servello1. Anterior cervical spine surgical complications: Safety comparison between teacher and student. 03-Feb-2021;12:43. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10572
Abstract
Background: Anterior cervical surgery has a widespread use. Despite its popularity, this surgery can lead to serious and life-threatening complications, and warrants the attention of skilled attending spinal surgeons with many years of experience.
Methods: We retrospectively evaluated postoperative complications occurring in 110 patients who underwent anterior cervical surgery (anterior cervical discectomy without fusion, anterior cervical discectomy and fusion, and anterior cervical disc arthroplasty) between 2013 and 2020. These operations were performed by an either an attending surgeon with 30 years experience versus a novice neurosurgeon (NN) with less than 5 years of training with the former surgeon. Complications were variously identified utilizing admission/discharge notes, surgical reports, follow-up visits, and phone calls. Complications for the two groups were compared for total and specific complication rates (using the Pearson’s Chi-square and Fisher’s test).
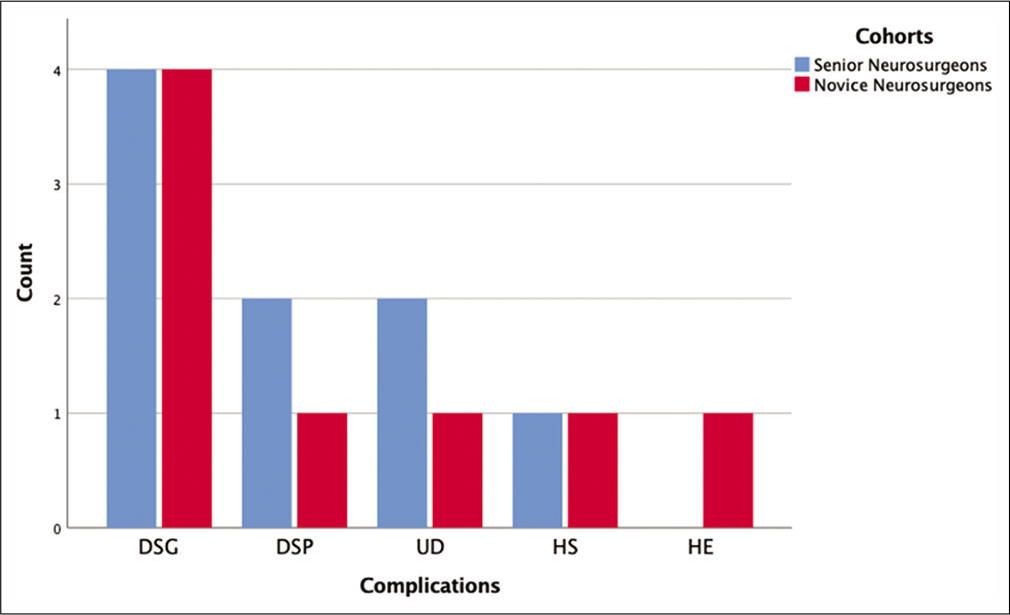
Results: The total cumulative complication rate was 15.4% and was not significantly different between the two cohorts. The most frequent postoperative complication was dysphagia. Notably, there were no significant differences in total number of postoperative instances of dysphagia, dysphonia, unintended durotomy, hypoasthenia, and hypoesthesia; the only difference was the longer operative times for NNs.
Conclusion: Surgeons’ years of experience proved not to be a critical factor in determining complication rates following anterior cervical surgery.
Keywords: Anterior approach, Cervical spine, Complication rate, Learning curve, Retrospective study
INTRODUCTION
Using the anterior approach to the cervical spine, many spinal surgeons perform anterior cervical discectomy and fusion (ACDF), anterior cervical discectomy (ACD) without fusion, anterior cervical corpectomy and fusion, anterior cervical discectomy and arthroplasty (ACDA), or hybrid surgeries.[
One study documented an average 137,000 ACDF performed/year in the U.S. between 2006 and 2013.[
Despite its widespread use, the anterior approach is not devoid of potential serious complications.
Here, we evaluated whether the postoperative complication rates following anterior cervical surgery varied based on the surgeons’ years of practice: senior neurosurgeons (SNs) (SN, with more than 30 years of experience) versus novice neurosurgeons (NNs) (NN, with <5 years of training with the former surgeons).
MATERIALS AND METHODS
This was a retrospective study on complications rates obtained from medical records (follow-up time of 1 year) of patients undergoing (through a right-sided anterior cervical spine approach) ACD (1 patient), ACDF (105 patients), and ACDA (4 patients).
The procedures were performed from 2013 to 2020 (with 0-Arm Guidance at our institution, IRCCS “Istituto Ortopedico Galeazzi”) by either a SN versus a NN. Data were obtained from admission/discharge notes, clinical diaries, operative summaries, follow-up visits, and phone calls.
Data of interest included patients’ age and symptoms, radiological diagnosis, type of surgery (ACDF, ACD, and ACDA), operative time, and peri/postoperative complications.
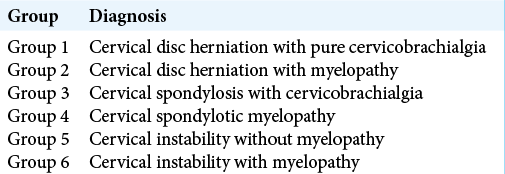
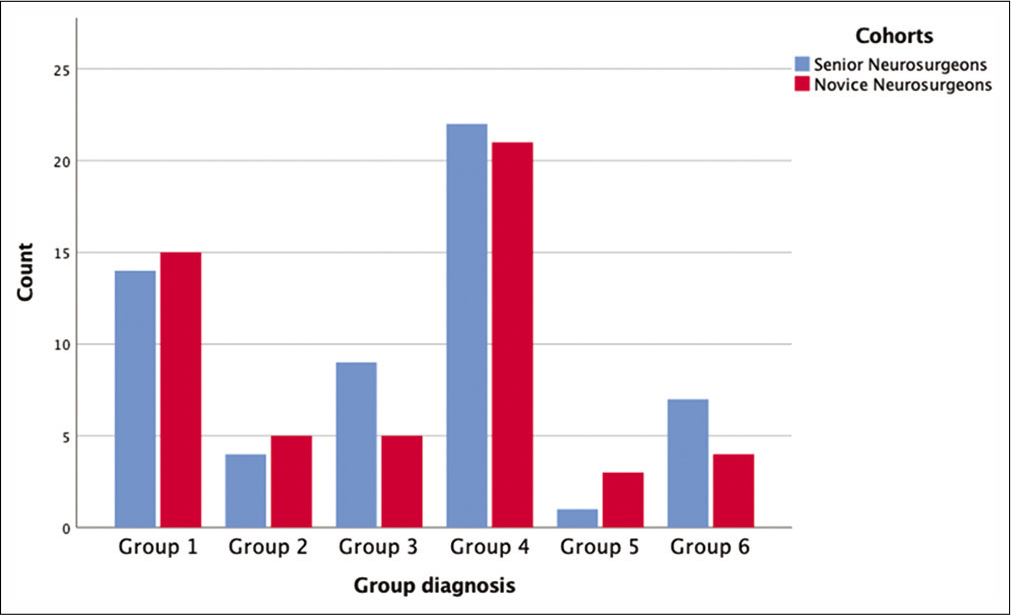
Based on a combination of clinical and radiological features, patients were divided into six groups [
Clinical parameters
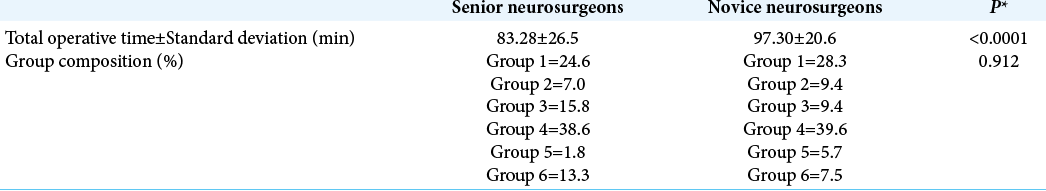
Patients in the SN’ and NN’ groups, respectively, averaged 57 (standard deviation [SD] = 13.36) and 54 (SD = 14.69) years of age and exhibited comparable degrees of radiculopathy and/or myelopathy. Mean operative times for the two cohorts were evaluated and compared utilizing Mann– Whitney U-test; surgical procedure durations ranged from 41 to 161 min (mean = 83.28, SD = 26.5) and from 60 to 158 min (mean = 97.30, SD = 20.6) for the SN and NN, respectively [
Surgical complications divided into eight groups
Complications were analyzed in patients who underwent ACD, ACDF, and ACDA.
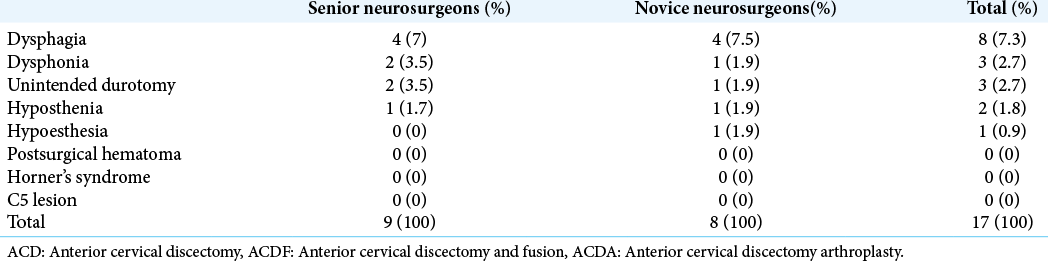
Surgical complications were divided into eight groups as they are in the literature: (1) dysphagia, (2) dysphonia, (3) unintended durotomy, (4) hyposthenia, (5) hypoesthesia, (6) hematoma, (7) Horner’s syndrome, and (8) C5 lesions. The frequencies of these complications were then compared for Cohort I SNs (57 patients) versus Cohort II, NNs, (53 patients) using Pearson’s Chi-square test and Fisher’s test. Computations were made using SPSS (IBM Corp. Release, IBM SPSS Statistics for macOS, Version 26.0).
RESULTS
The cumulative complication rate was 15.4% (17/110) that was similar for both cohorts, 9 in SN (15.7%) versus 8 in NN cohort (15.09%) [
DISCUSSION
Epstein reported morbidity rates of ACD and ACDF spanning from 13.2% to 19.3%.[
CONCLUSION
In Epstein’s review, ACD and ACDF complication rates ranged from 13.2 to 19.3%.[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien). 1989. 99: 41-50
2. Deora H, Kim SH, Behari S, Rudrappa S, Rajshekhar V, Zileli M. Anterior surgical techniques for cervical spondylotic myelopathy: WFNS spine committee recommendations. Neurospine. 2019. 16: 408-20
3. Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA. Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine (Phila Pa 1976). 2000. 25: 1603-6
4. Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int. 2019. 10: 100
5. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007. 32: 2310-7
6. Huang ZY, Wu AM, Li QL, Lei T, Wang KY, Xu HZ. Comparison of two anterior fusion methods in two-level cervical spondylosis myelopathy: A meta-analysis. BMJ Open. 2014. 4: e004581
7. Maharaj MM, Mobbs RJ, Hogan J, Zhao DF, Rao PJ, Phan K. Anterior cervical disc arthroplasty (ACDA) versus anterior cervical discectomy and fusion (ACDF): A systematic review and meta-analysis. J Spine Surg. 2015. 1: 72-85
8. Quinones-Hinojosa A.editors. Schmidek and Sweet: Operative Neurosurgical Techniques 2-Volume Set: Indications, Methods and Results. Amsterdam: Elsevier Health Sciences; 2012. 2: 1747-55
9. Saifi C, Fein AW, Cazzulino A, Lehman RA, Phillips FM, An HS. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018. 18: 1022-9
10. Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017. 3: 444-59