- Department of Neurosurgery, NTT Medical Center Tokyo, Tokyo, Japan.
DOI:10.25259/SNI_102_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sho Tsunoda, Tomohiro Inoue, Masafumi Segawa, Atsuya Akabane. Anterior transpetrosal resection of the lower ventral pontine cavernous malformation: A technical case report with operative video. 07-Jun-2021;12:261
How to cite this URL: Sho Tsunoda, Tomohiro Inoue, Masafumi Segawa, Atsuya Akabane. Anterior transpetrosal resection of the lower ventral pontine cavernous malformation: A technical case report with operative video. 07-Jun-2021;12:261. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10866
Abstract
Background: Surgical treatment of pontine cavernous malformations (CMs) is challenging due to the anatomical difficulties and potential risks involved. We successfully applied an anterior transpetrosal approach (ATPA) to remove a lower ventral pontine CM, and herein we discuss the outline of our procedure accompanied by a surgical video.
Case Description: A 50-year-old woman presenting with progressively worsening diplopia was urgently admitted to our hospital. Preoperative images showed a lower ventral pontine CM compressing the corticospinal tract posteriorly. Considering the location of the CM, we determined that an ATPA was the appropriate approach to achieve a more anterolateral trajectory. We performed extradural anteromedial petrosectomy and penetrated the brainstem from the point just below the anterior inferior cerebellar artery and above the root exit zone of the abducens nerve, which might be located in the somewhat lowest border of actual maneuverability in the ATPA. Maneuverability through this corridor was sufficient without hindering and darkening the high magnification microscopic view, as demonstrated in our surgical video.
Conclusion: This report demonstrates surgical treatment of a lower ventral pontine CM using the ATPA. The surgical video we present provides information that is useful for understanding this technique’s maneuverability and working window.
Keywords: Anterior transpetrosal approach, Cavernous malformation, Peritrigeminal zone
INTRODUCTION
Although surgical treatment of brainstem cavernous malformations (CMs) is challenging due to its anatomical difficulties and potential risks, it is a crucial course of action when bleeding recurs or when symptoms are progressively deteriorating.[
Herein, we share our experience with the application of an ATPA to surgically remove a lower ventral pontine CM from the peritrigeminal zone (PTZ) in a case patient along with a surgical video.
CLINICAL PRESENTATION
Preoperative course
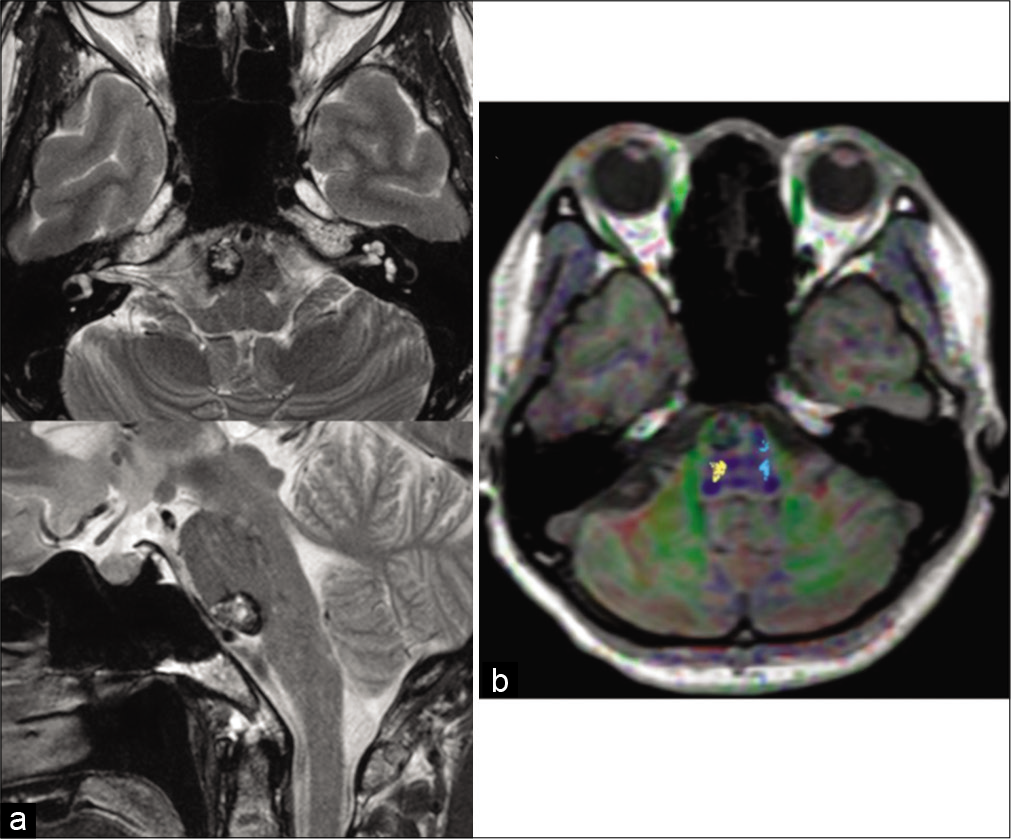
A 50-year-old woman presenting with sudden-onset diplopia associated with headache and vomiting was urgently admitted to our hospital. On admission, neurological examinations revealed esotropia in the right eye (5° angle at the front) and abducens nerve disorder (approximately Grade 4 on a five-grade evaluation of right gaze). These symptoms had been worsening progressively for several days before the admission. Magnetic resonance imaging revealed a heterogenous hyperintense mass (maximum diameter of 16 mm) with a hypointense rim located at the lower half of the ventral pons [
We diagnosed the patient with pontine CM. We initially selected conservative treatment, but the patient’s symptoms were not mitigated and she eventually opted for surgical treatment. Therefore, we decided to remove the CM. Because of the ventral location of the patient’s CM, as preoperative tractography showed posterior displacement of the corticospinal tract (CST) [
Surgical procedure
The patient underwent surgical removal with motor-evoked potential, auditory brainstem response, and facial nerve monitoring throughout the operation. A lumbar drain was preoperatively inserted to minimize brain retraction during surgery.
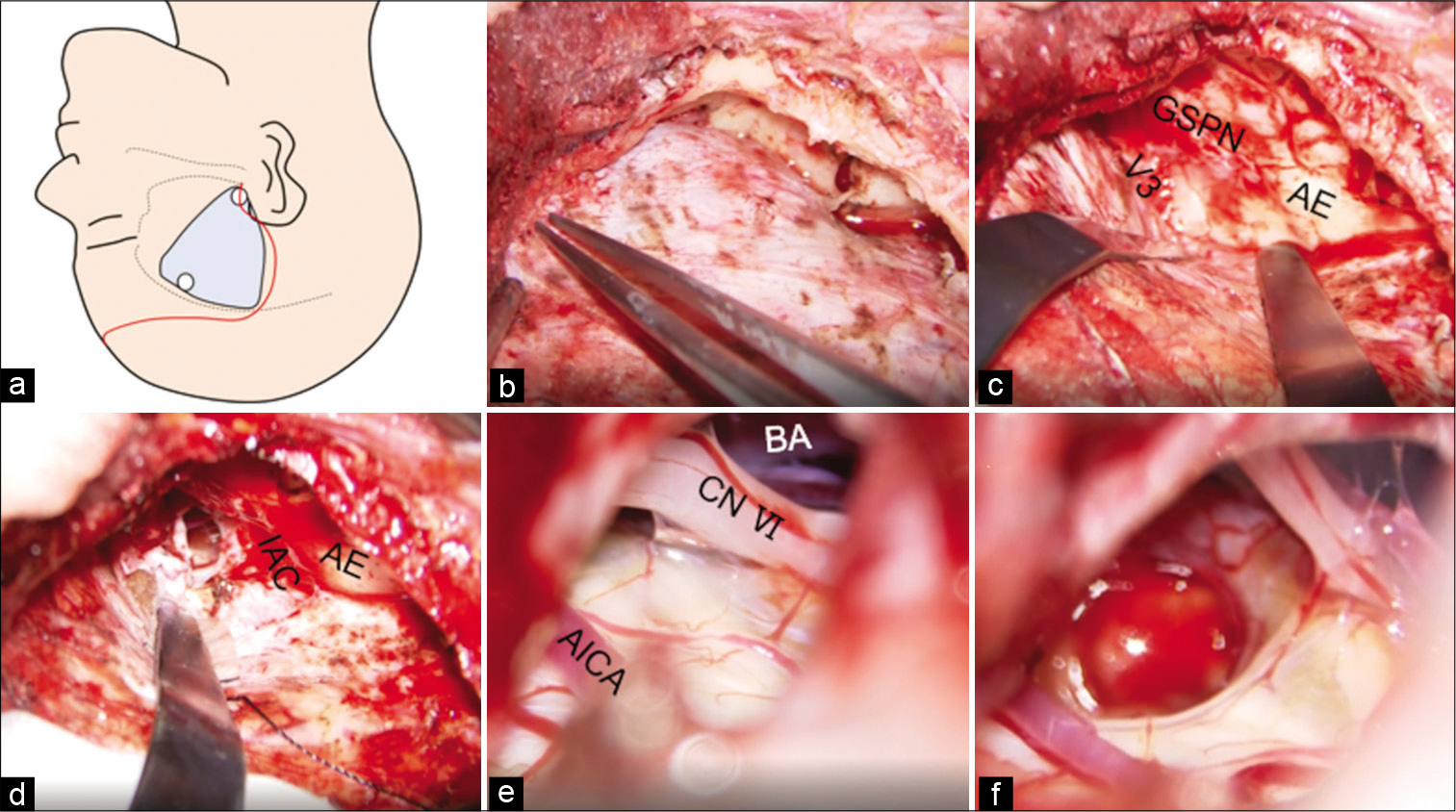
With the patient in a 10° semi-Fowler position, the head was rotated until parallel with the floor and fixed in a Mayfield skull clamp. A question mark scalp incision started at the midpoint of the zygomatic arch (anterior to the tragus), extended by one fingerbreadth posteriorly, and then turned anteriorly to the superior frontal area [
Figure 2:
(a) Schema demonstrating the scalp incision and craniotomy range. (b) The middle base was flattened. (c) The dura mater was elevated up to the point where the GSPN submerges inside the V3. (d) Extradural anterior–medial petrosectomy was carried out in the range up to the GSPN on the lateral border, ICA on the deep anterior border, geniculate ganglion, basal turn of the cochlea and AE on the posterior border, and V3 on the medial border. The extent further expanded inferior-posteriorly by opening the anterior superior wall of the IAC and removing the tip of the petrous bone up to the height of the IPS. (e) The REZs of the trigeminal nerve, swollen pons, BA, AICA, and CN VI were confirmed. (f) The brainstem was incised at the point of the Peritrigeminal zone with yellow discoloration between the AICA loop and CN VI, and the hemangioma was completely removed. GSPN: Greater superficial petrosal nerve, V3: Mandibular division of the trigeminal nerve, AE: Arcuate eminence, IAC: Internal auditory canal, BA: Basilar artery, AICA: Anterior inferior cerebellar artery, CN VI: Abducens.
Video 1
Postoperative course
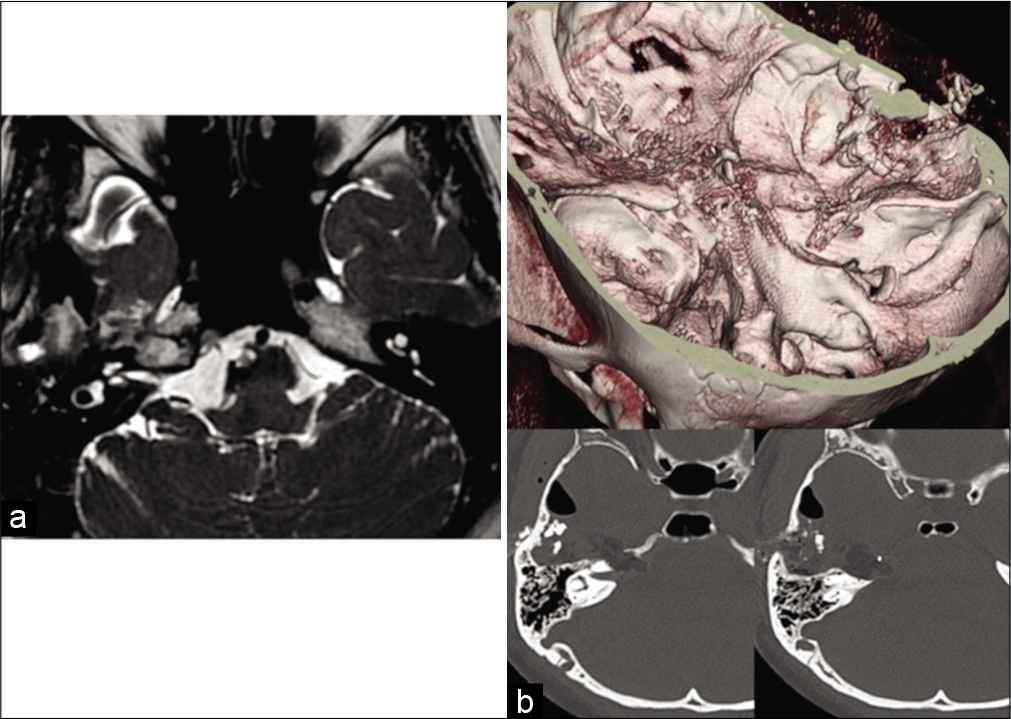
The lesion was completely removed postoperatively [
DISCUSSION
Selecting an access route that preserves essential neural tissue is crucial in the surgical treatment of brainstem CMs, and it is often determined based on the two-point method proposed by Brown [
Although pontine CMs are common, constituting 57–77.8% of brainstem CMs, their anatomical features (large amount of cranial nerve nuclei in addition to sensory and motor pathways) make surgical treatment extremely difficult.[
Lateral access through lateral suboccipital craniotomy can obtain substantial working space along with the longitudinal axis of the brainstem, but the working angle of the horizontal axis is extremely narrow and obstructed by cranial nerves, especially the seventh-to-eighth cranial nerve complex, resulting in higher postoperative risk of auditory impairment and facial palsy.[
Among anterior approaches, the transclival route offers the most linear path to the anterior surface of the brainstem, and some successful cases using transnasal endoscopy have been reported.[
Other methods, such as the transsylvian transtentorial approach[
These data suggest that the ATPA is the ideal approach if the lesion is located more ventral and spreads to the relatively caudal side of pons.
Reports on the observable range of the ATPA vary as well. One report indicated that the range is limited to the upper pons around the trigeminal nerve cranial to the AICA even if the upper edge of the zygoma was drilled off prior to applying the ATPA.[
Although safe entry zones of the pons have been widely reported on,[
In our case, we penetrated the lesion at the point of the PTZ just below the AICA and above the REZ of the abducens nerve, which might be located at the somewhat lowest border of actual maneuverability in an ATPA. By exposing the posterior fossa dura as wide as possible, exposing the anterior dura of the IAC, and exposing the petrous bone to as low as the IPS [
CONCLUSION
Our surgical [
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on:
www.surgicalneurologyint.com
References
1. Abla AA, Benet A, Lawton MT. The far lateral transpontomedullary sulcus approach to pontine cavernous malformations: Technical report and surgical results. Oper Neurosurg. 2014. 10: 472-80
2. Abla AA, Lekovic GP, Turner JD, de Oliveira JG, Porter R, Spetzler RF. Advances in the treatment and outcome of brainstem cavernous malformation surgery: A single-center case series of 300 surgically treated patients. Neurosurgery. 2011. 68: 403-15
3. Akiyama O, Matsushima K, Nunez M, Matsuo S, Kondo A, Arai H. Microsurgical anatomy and approaches around the lateral recess with special reference to entry into the pons. J Neurosurg. 2017. 129: 740-51
4. Ardeshiri A, Ardeshiri A, Wenger E, Holtmannspötter M, Winkler PA. Subtemporal approach to the tentorial incisura: Normative morphometric data based on magnetic resonance imaging scans. Operative Neurosurgery. 2006. 58: ONS22-8
5. Bricolo A. Surgical management of intrinsic brain stem gliomas. Oper Tech Neurosurg. 2000. 2: 137-54
6. Brown A. The two-point method: Evaluating brain stem lesions. BNI Q. 1996. 12: 20-4
7. Cavalheiro S, Yagmurlu K, da Costa MD, Nicácio JM, Rodrigues TP, Chaddad-Neto F. Surgical approaches for brainstem tumors in pediatric patients. Childs Nerv Syst. 2015. 31: 1815-40
8. Essayed WI, Singh H, Lapadula G, Almodovar-Mercado GJ, Anand VK, Schwartz TH. Endoscopic endonasal approach to the ventral brainstem: Anatomical feasibility and surgical limitations. J Neurosurg. 2017. 127: 1139-46
9. François P, Ben Ismail M, Hamel O, Bataille B, Jan M, Velut S. Anterior transpetrosal and subtemporal transtentorial approaches for pontine cavernomas. Acta Neurochir (Wien). 2010. 152: 1321-9
10. Fritschi JA, Reulen HJ, Spetzler RF, Zabramski JM. Cavernous malformations of the brain stem. Acta Neurochir (Wien). 1994. 130: 35-46
11. Giliberto G, Lanzino DJ, Diehn FE, Factor D, Flemming KD, Lanzino G. Brainstem cavernous malformations: Anatomical, clinical, and surgical considerations. Neurosurg Focus. 2010. 29: E9
12. Hauck EF, Barnett SL, White JA, Samson D. The presigmoid approach to anterolateral pontine cavernomas. Clinical article. J Neurosurg. 2010. 113: 701-8
13. Hebb MO, Spetzler RF. Lateral transpeduncular approach to intrinsic lesions of the rostral pons. Neurosurgery. 2010. 66: 26-9
14. Hu P, Liang J, Bao Y, Li M, Ling F. The pterional transsylvian transtentorial approach to ventrolateral pontine cavernomas: Indications and techniques. World Neurosurg. 2014. 82: 1276-82
15. Kalani MY, Yagmurlu K, Martirosyan NL, Cavalcanti DD, Spetzler RF. Approach selection for intrinsic brainstem pathologies. J Neurosurg. 2016. 125: 1596-607
16. Kumar R, Singhi V. Tuberculous brain stem abscesses in children. J Pediatr Neurol. 2004. 2: 101-6
17. Kyoshima K, Kobayashi S, Gibo H, Kuroyanagi T. A study of safe entry zones via the floor of the fourth ventricle for brainstem lesions: Report of three cases. J Neurosurg. 1993. 78: 987-93
18. Linsler S, Oertel J. Endoscopic Endonasal transclival resection of a brainstem cavernoma: A detailed account of our technique and comparison with the literature. World Neurosurg. 2015. 84: 2064-71
19. MacDonald JD, Antonelli P, Day AL. The anterior subtemporal, medial transpetrosal approach to the upper basilar artery and ponto-mesencephalic junction. Neurosurgery. 1998. 43: 84-9
20. Ohue S, Fukushima T, Friedman AH, Kumon Y, Ohnishi T. Retrosigmoid suprafloccular transhorizontal fissure approach for resection of brainstem cavernous malformation. Neurosurgery. 2010. 66: 306-12
21. Ohue S, Fukushima T, Kumon Y, Ohnishi T, Friedman AH. Surgical management of brainstem cavernomas: Selection of approaches and microsurgical techniques. Neurosurg Rev. 2010. 33: 315-22
22. Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT. Cavernous malformations of the brainstem: Experience with 100 patients. J Neurosurg. 1999. 90: 50-8
23. Reisch R, Bettag M, Perneczky A. Transoral transclival removal of anteriorly placed cavernous malformations of the brainstem. Surg Neurol. 2001. 56: 106-15
24. Saito N, Sasaki T, Chikui E, Yuyama R, Kirino T. Anterior transpetrosal approach for pontine cavernous angioma-case report. Neurol Med Chir (Tokyo). 2002. 42: 272-4
25. Steiger HJ, Hänggi D, Stummer W, Winkler PA. Custom-tailored transdural anterior transpetrosal approach to ventral pons and retroclival regions. J Neurosurg. 2006. 104: 38-46
26. Strauss C, Romstöck J, Fahlbusch R. Pericollicular approaches to the rhomboid fossa. Part II.Neurophysiological basis. J Neurosurg. 1999. 91: 768-75
27. Yagmurlu K, Kalani MY, Preul MC, Spetzler RF. The superior fovea triangle approach: A novel safe entry zone to the brainstem. J Neurosurg. 2016. 127: 1134-8
28. Yokoyama K, Kawanishi M, Sugie A, Yamada M, Tanaka H, Ito Y. Microsurgical resection of a ventral pontine cavernoma via supratrigeminal zone by anterior transpetrosal approach: 2-dimensional operative video. Oper Neurosurg. 2019. 16: 396-6
29. Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Sugie A. Anterior transpetrosal approach for resection of ventral pontine cavernous angiomas: A case report. Surg Cereb Stroke. 2017. 45: 266-9