- Department of Neurosurgery, Lenox Hill Hospital, New York City, New York, United States.
Correspondence Address:
Omer Doron, Department of Neurosurgery, Lenox Hill Hospital, New York City, New York, United States.
DOI:10.25259/SNI_120_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Omer Doron, Julia R. Schneider, Jason Andre Ellis. Application of the subdural evacuating port system for the drainage of postoperative tension pneumocephalus: A technical note. 20-May-2022;13:204
How to cite this URL: Omer Doron, Julia R. Schneider, Jason Andre Ellis. Application of the subdural evacuating port system for the drainage of postoperative tension pneumocephalus: A technical note. 20-May-2022;13:204. Available from: https://surgicalneurologyint.com/surgicalint-articles/11612/
Abstract
Background: Tension pneumocephalus is a neurosurgical emergency requiring prompt intervention. A variety of either temporizing or definitive methods was previously described as part of its management. Here, we report on an off-label use of a bed-side device and the subdural evacuating port system (SEPS)™ for the treatment of tension pneumocephalus.
Methods: The SEPS™ (Medtronic Dublin, Ireland) is a minimally invasive tool that is indicated for the removal of chronic or subacute subdural hematomas and at the patient’s bedside. We describe the use of this system to evacuate tension pneumocephalus.
Results: A 44-year-old patient operated in our institution was presented with sudden obtundation 4 days post resection of esthesioneuroblastoma. Imaging confirmed a significant tension pneumocephalus. Immediate bedside decompression using a SEPS bolt placed frontally was performed, achieving rapid evacuation and patient regained consciousness. A definitive skull base reconstruction was done at the operating room at a later stage.
Conclusion: The SEPS™, well-known for evacuation of CSDH, can be potentially used as a bed-side tool to effectively treat mass effect created by tension pneumocephalus. As a readily-available and commercially used device, it can provide a simple and standard toolkit suitable for an emergent temporizing procedure.
Keywords: Brain compression, Burr hole, Craniotomy, Subdural evacuating port system, Tension pneumocephalus
INTRODUCTION
Tension pneumocephalus is a treatable neurosurgical emergency that occurs when air enters through a dural defect and becomes trapped, creating a mass effect.[
There are two postulated mechanisms leading to the development of pneumocephalus: the “ball- valve” and the “inverted bottle” mechanisms. The former suggests that positive pressure (e.g., sneezing, coughing, Valsalva maneuvers) pulls air intracranially through a cranial defect, and resists outflow leading to tension pneumocephalus.[
CT is the gold standard for the diagnosis of both pneumocephalus and tension pneumocephalus, requiring only 0.55 mL of air for detection.[
MATERIALS AND METHODS
The subdural evacuating port system (SEPS)™ (Medtronic Dublin, Ireland) is a minimally invasive tool that is indicated for the removal of chronic or subacute subdural hematomas and hygromas.[
We report on a case where an off-label use of this system, taking advantage of its rapid and simple bed-side instrumentation, was performed as a temporizing measure for treating an acutely decompensating patient suffering a postoperative tension pneumocephalus.
RESULTS AND CASE PRESENTATION
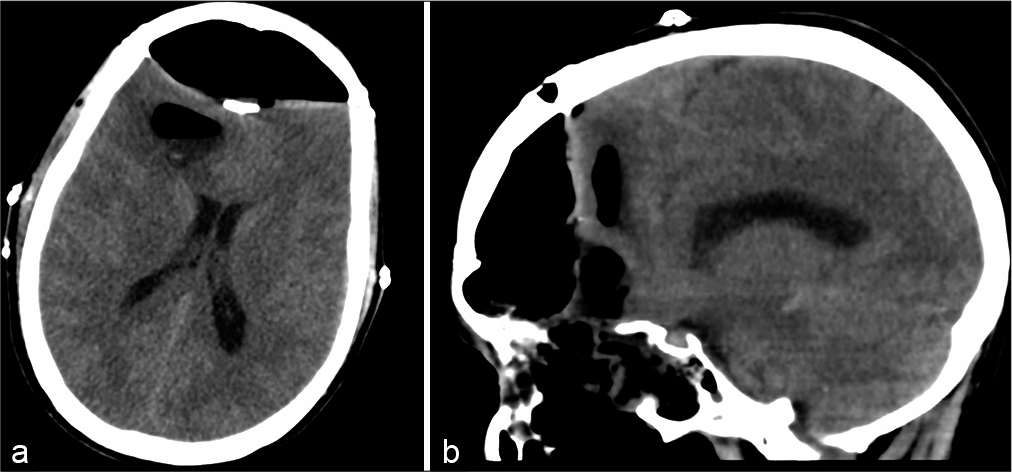
A 44-year-old man underwent a resection of a large esthesioneuroblastoma in our institution, using a cranial open approach. Four days postoperatively, he was found obtunded, with a sudden impairment in level of consciousness. The patient then undergone an emergent head computed tomography (CT) in the ICU showing a significant bifrontal extradural pneumocephalus compressing the frontal lobes [
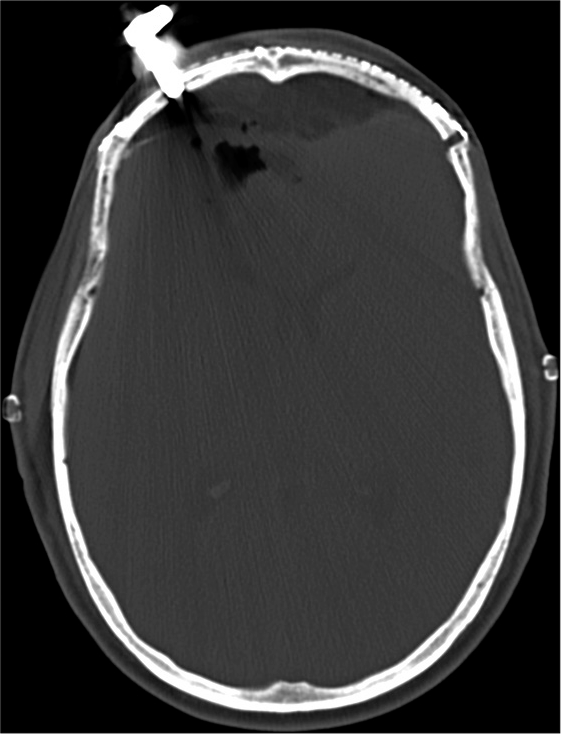
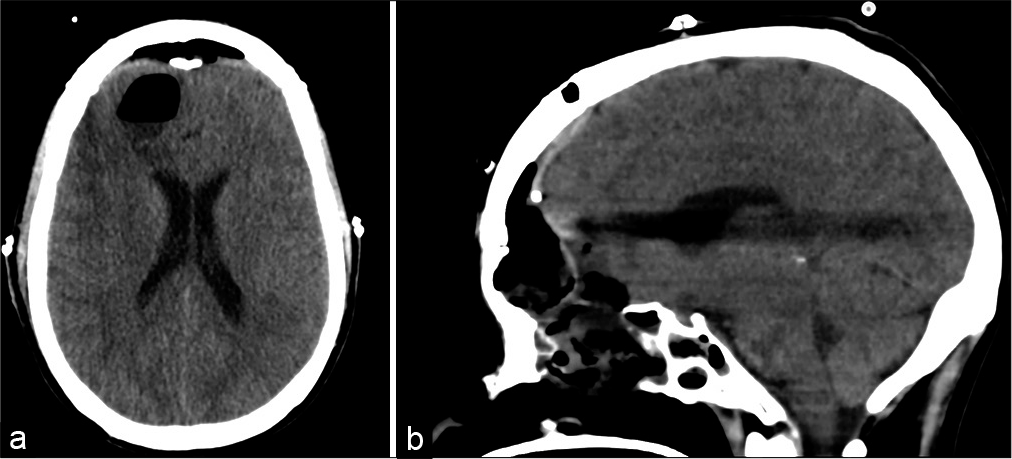
A diagnosis of tension pneumocephalus was made and it was decided by the attending neurosurgeon to utilize the SEPS for rapid decompression as the right frontal side was chosen as the insertion point. The patient was immediately prepared and using local anesthetic; a stab incision was made in his right forehead down to the bone. A twist drill burr hole was placed and the SEPS bolt was screwed in. The SEPS JP drain was then attached and placed at self-suction. The entire procedure time took approximately 5 min. Following air drainage into the bag, the patient immediately improved and regained full consciousness. Follow-up CT imaging performed several hours later confirmed excellent brain decompression [
The patient subsequently underwent elective skull base reconstruction to seal the postoperative defect in his anterior cranial base [
DISCUSSION
Although rarely under tension, pneumocephalus is a common occurrence after neurosurgical procedures.[
This case, to the best of our knowledge, is the first to report on the utilization of the SEPS at the bedside as an emergent temporizing treatment of tension pneumocephalus.
Several temporizing measures for tension pneumocephalus have been described. Bed rest, raising the bed head, hyperosmolar therapy, and abstaining from valsalva-like maneuvers comprise the conservative approaches. Normobaric hyperoxia with 100% inspired oxygen facilitates faster resorption of pneumocephalus and has been described in the literature.[
The SEPS is indicated for subacute and chronic subdural hematomas and hygromas and has been shown to be effective, safe, and durable for the indicated uses.[
The kit is composed of a bolt connected to a drain with a closed self-suction system and can be inserted through a 5-mm incision after twist-drilling the skull [
Therefore, the system is capable of decompressing tension pneumocephalus in a similar manner to evacuating a subdural hematoma through a minimally invasive and quick procedure conducted at the bedside, rather than the operating room.
We believe that a potential advantage of this technique lies both in the rapid, bedside nature of this device, as well as the fact, it is an already assembled kit, which does not require gathering of different instruments, which could be challenging in an emergent ward setup. Importantly, the bolt can be left in place for a few days, allowing ample time for evacuation of air, which can accumulate in significant amounts particularly after skull base surgery.[
CONCLUSION
The SEPS™, known for its use in evacuation of CSDH, can be potentially used as a bed-side tool to effectively treat mass effect created by air trapped within the cranium. As a readily-available and off-the shelf device, it can provide a simple and standard toolkit suitable for an emergent temporizing procedure for the treatment of tension pneumocephalus.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dabdoub CB, Salas G, Silveira E, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int. 2015. 6: 155
2. Healy J, Grant M, Melnyk S, Boldt B. Tension pneumocephalus a rare complication of cerebrospinal fluid leak. Radiol Case Rep. 2018. 14: 365-7
3. Hong B, Biertz F, Raab P, Scheinichen D, Ertl P, Grosshennig A. Normobaric hyperoxia for treatment of pneumocephalus after posterior fossa surgery in the semisitting position: A prospective randomized controlled trial. PLoS One. 2015. 10: e0125710
4. Hubbard JL, McDonald TJ, Pearson BW, Laws ER. Spontaneous cerebrospinal fluid rhinorrhea: Evolving concepts in diagnosis and surgical management based on the Mayo Clinic experience from 1970 through 1981. Neurosurgery. 1985. 16: 314-21
5. Karavelioglu E, Eser O, Haktanir A. Pneumocephalus and pneumorrhachis after spinal surgery: Case report and review of the literature. Neurol Med Chir. 2014. 54: 405-7
6. Kenning TJ, Dalfino JC, German JW, Drazin D, Adamo MA. Analysis of the subdural evacuating port system for the treatment of subacute and chronic subdural hematomas. J Neurosurg. 2010. 113: 1004-10
7. Klein J. Normobaric pulmonary oxygen toxicity. Anesth Analg. 1990. 70: 195-207
8. Lunsford LD, Maroon JC, Sheptak PE, Albin MS. Subdural tension pneumocephalus. Report of two cases. J Neurosurg. 1979. 50: 525-7
9. Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir. 1967. 16: 1-78
10. Pulickal GG, Sitoh YY, Ng WH. Tension pneumocephalus. Singapore Med J. 2014. 55: e46-8
11. Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000. 84: 115-7
12. Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: Case illustrations and review. Neurocrit Care. 2010. 13: 152-8
13. Singla A, Jacobsen WP, Yusupov IR, Carter DA. Subdural evacuating port system (SEPS) minimally invasive approach to the management of chronic/subacute subdural hematomas. Clin Neurol Neurosurg. 2013. 115: 425-31
14. Solomiichuk V, Lebed V, Drizhdov K. Posttraumatic delayed subdural tension pneumocephalus. Surg Neurol Int. 2013. 4: 37
15. Venkatesh SK, Bhargava V. Clinics in diagnostic imaging (119) Post-traumatic intracerebral pneumatocele. Singapore Med J. 2007. 48: 1055-9
16. Yin C, Chen BY. Tension pneumocephalus from skull base surgery: A case report and review of the literature. Surg Neurol Int. 2018. 9: 128