- Department of Neurosurgery, College of Medicine, University of Baghdad, Baghdad, Iraq.
Correspondence Address:
Moneer K. Faraj M.B., Ch.B., FICMS, FACS, FICS, IFAANS, Department of Neurosurgery, College of Medicine, University of Baghdad, Baghdad, Iraq. drmkfaraj@comed.uobaghdad. edu.iq
DOI:10.25259/SNI_664_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Faraj MK. Are innovation and creativity possible in a country at war? My story of neurosurgery in Baghdad, Iraq. Surg Neurol Int 02-Sep-2022;13:402
How to cite this URL: Faraj MK. Are innovation and creativity possible in a country at war? My story of neurosurgery in Baghdad, Iraq. Surg Neurol Int 02-Sep-2022;13:402. Available from: https://surgicalneurologyint.com/surgicalint-articles/11840/
Editor’s Note:
In a recent SNI-sponsored educational conference with neurosurgeons in Baghdad, the SNI faculty and attendees from Iraq had an opportunity to hear from Baghdad neurosurgeons on their work during the difficult time of war in their recent history. The description of the meeting can be found in SNI “The most inspiring and mind-blowing meetings ever”: Highlights of the 15th SNI Baghdad Neurosurgery Online Meeting, from Participants’ Perspectives. One of the talks given was by Dr. Moneer Faraj, who was Chief of the Department of Neurosurgery and Hospital Director of The Hospital of Neurosciences, Baghdad, Iraq and he is now Deputy Rapporteur for the Arabian Board of Neurosurgery. Dr Faraj was educated in Iraq, and is a member of multiple international specialty neurosurgical societies. He took courses in many subspecialties in neurosurgery around the world. He has organized meetings throughout Iraq in multiple specialties, and on the use of the Gamma Knife. After hearing his inspiring and innovative talk, I asked him to send me a description of his background and experience in neurosurgery in Iraq. I decided to publish his answer as submitted in its entirety for our readers to enjoy.
Emeritus Editor-in-Chief
James I. Ausman, MD, PhD
My dear professor James Ausman,
It was an honor for me to participate in this outstanding meeting.
I did not expect this response reflected in the comments and feedback from the audience.
I would like to discuss our activities in Iraq.
Functional neurosurgery started in the 1980s with the admission of the Leksell stereotactic frame, but the actual work with deep brain stimulation (DBS) was first started in 2007, and I would like to tell you how we began that work.
A few years before 2007, several doctors trained in the USA and performed surgeries under the supervision of American and French surgeons in Jordan and Amman. Still, due to the war condition, only one of the team, a neurologist, returned to Iraq.
We face a problem that we have about $1 million DBS stuff that will be expired, there are patients in need of it, and nobody can implant it for them.
The neurologist Dr. Akeel, the Neurosciences hospital manager, asked me to solve this problem. After several negotiations with the Ministry of Health, they agreed to send me with the neurologist Dr. Akeel and a biomedical engineer to India to take two patients with us and train there.
We noticed that the surgeon took instructions from the Indian biomedical engineer and performed only nine patients before we came to him; he used the Radionics frame, in which we do not have in Iraq. He used the software of the Novalis radiosurgery to do the planning.
I communicated with the Medtronic office and told him their project would fail in Iraq unless you sent someone to train us on it. They sent us an engineer I regard as my spiritual father in DBS. He is Mr. Janardan, and in 1 day, from 9 AM to 7 PM, he gave us a detailed lecture that I continued with my Sony camera. Every few hours, I changed the memory chip to continue documenting it. In 1 day, he explained to us the whole process from preoperative selection, preparation, how to do the surgery, and the postoperative programming.
When we returned, we faced several issues:
First, we saw the frame of radionics, and we have the Leksell, in which I did not have any training on. I spent 2 weeks assembling and disassembling the frame to understand how it works.
Second, the Micro-target Drive should be fixed over the arch of the stereotactic frame. I did not see this before, so I started to take pictures of several attempts to fix this drive on the arch of the frame. I sent the images to Janardan, and he thankfully guided me on how to assemble that Drive.
Third, at that time, we had only an open MRI with 0.25 Tesla, and nobody in the world worked with this device for DBS. The nearby hospital that has a 1.5 T closed MRI they have no zip drive to record the patient; so we had to play with the software of the open MRI to get a good picture that is accepted by the Frame Link software of the DBS on an account that the patient will be in the MRI gantry for 45 min.
Fourth, when we transmit the CD of the MRI to the frame link software, the CDs were based on the Windows operating system, and the frame link is a Linux-based operating system, so it cannot recognize that there is a CD. We had to make a video conference at the time with the Medtronic personnel to make changes in the Lenox program to let it be capable of reading windows Cd.
After resolving all these problems, we started our first DBS surgery. It lasts for 13 h. During surgery, we faced several issues intraoperatively that made us think of stopping the surgery, but we resolved them later.
I can assure you that all DBS surgeries in Iraq were performed without direct available Medtronic’s intraoperative supervision.
We are now performing the surgeries with an average of 3 1/2 h. I trained two teams working on their own in two tertiary centers in Baghdad; we plan to conduct several workshops in Iraq to expand the work in DBS here.
Another issue I would like to inform you about is when the Arabian board of neurosurgery administration office was changed in 2014, and I became the director of the local committee. The main issue was that the success rate for our students every year was <20%. With one of my colleagues, I sought to attend the examination committee as a guest at our own expense and noticed how they performed the exam. After this, we decided to make simulated examinations for several years for all students before they attend the test. Nowadays, we use the team software with different classes, and almost every 2 weeks, we send them an inquiry with explanations so that they use the method of the exam and the proper way of answering.
In the past 4 years, we had a more than 80% success rate.
I also negotiated with the American Association of the neurological surgeon, and we got free membership in that association for all our students until they graduate from the Arabian board.
We agreed with Professor Atul Goel of Mumbai and professor Mika Niemela from Finland to send our students for 1 month’s fellowship in India and Finland to see different systems and diverse opinions on surgeries.
But unfortunately, these fellowships stopped after the corona pandemic.
The first Gamma Knife radiosurgery perfection machine was installed in 2016 in our center. And since then, we had more than 4000 patients (
We trained several local neurosurgeons on the techniques of the Gamma Knife. And nowadays, we have four Gamma Knives in Iraq, two in Baghdad and one in each north and south of Iraq. A recent upgrade to the Icon version was installed recently for the two machines in Baghdad.
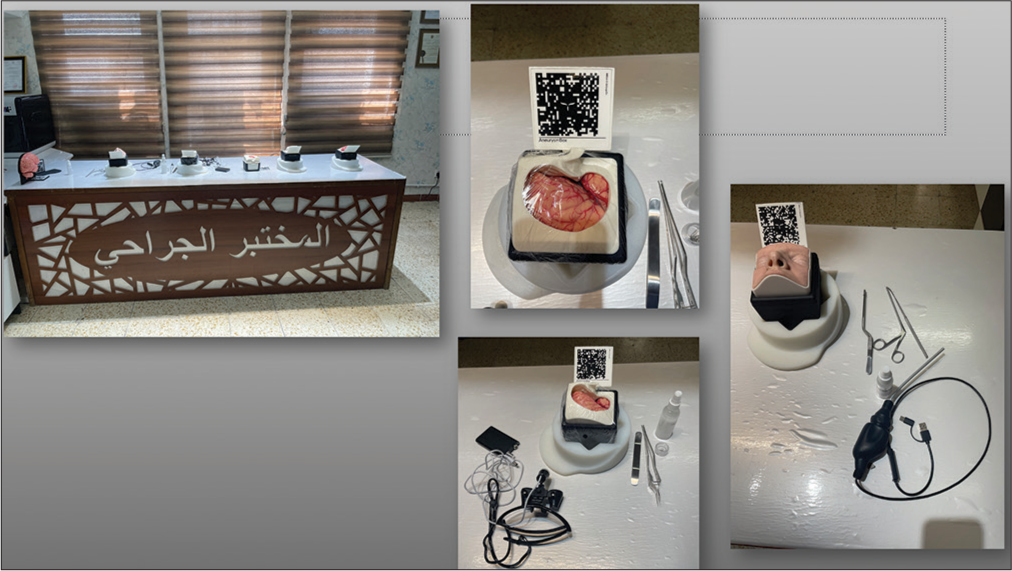
Our surgical laboratory was established in 2016 with personal funding. In
Every student will not be eligible to perform the final examination on the board without completing these three courses.
We also established the first 3D printer section in the laboratory devoted to neurosurgical research. Several papers were issued, and patents were recorded with the 3D printing technology.[
We also had our first digital library, with more than 25 terabytes of materials, for basic and clinical neurosciences, including books, lectures, and video courses [
However, in the creative work as a neurosurgeon, I work alone, but as Wilder Penfield mentioned in his life story that “no man alone,” I started to make my team by creating a friendship with those who are interested in our jobs, especially biomedical technicians who work with me when they have access time. I opened a channel with biomedical engineering and medical physics colleges to cooperate with them by sending students on master’s or Ph.D. thesis to work with me on our projects.
I have now a very good group of personnel who are working with me directly on several projects:
We are now working on the Gamma Knife icon facemask, which usually costs around US$250. We created a new mask which typically cost no more than 4 dollars.
Another project is making a free face mask that fits with the Gamma Knife and any linear accelerator for any patient whose head looks like it.
We are working on making certain accessories in the Leksell frame to fix it in the head without using painful screws. These projects now are in corporation wave medical physicist on her master thesis.
I am working with a master’s degree biomedical engineer on the special pressure sensor on the brain tractors as part of the eletronics integrated with surgical instruments (EISI) project.[
I also have another biomedical engineer with a Ph.D. thesis for manufacturing the pen needle holder presented in the webinar.
Unfortunately, all these ideas and projects were made individually without my neurosurgeon colleagues’ cooperation or interest. I do not know when the companies will pay attention to them since most of them we cannot manufacture locally. But I continue my work despite anything.
For writing, I’m planning to write two essays which will take a long time before completing them.
Title “An invitation to change the way we learn anatomy neuroanatomy as an example” in this essay, I want to criticize many issues like the way we describe a structure and the names of tissues and suggest a new system suitable more for the 21st century Title “'Literaturization’ of science: A scientific essay in a nonscientific way.”
How we learn the facts makes artificial intelligence better than the human brain. This is not because IA is better than the human brain, but the educational process must be changed before AI beats us.
Outside my professional Carrier, I am interested in reading. I have a library with more than 15,000 books on different knowledge. In the recent few years, I have been interested in human development, especially after reading the diary of neurosurgeon James Dotty the first CEO of Cyberknife; it is called “in the cabinet of the magician,” and actually, he led me to look for David Hawkins books and his 1000° of the level of consciousness. I spend 3 years in the Academy of self-development in Kuwait, after which I am now a member of the self-realization fellowship of Paramahansa Yogananda in Los Angeles. Also, I participated in several courses at Naropa University in Colorado for Buddhist studies. They helped me in expanding my knowledge, change my priorities in life, and change the way I look at everything.
I am sorry for this very long letter. You asked me to write something to know me, and I thank you very much for your nice letter.
With my best regards
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arkawazi BM, Faraj MK, Al-Attar Z, Hussien HA. Short term effectiveness of gamma knife radiosurgery in the management of brain arteriovenous malformation. Open Access Maced J Med Sci. 2019. 7: 3221-4
2. Faraj MK, Al-Baldawi IA, Alzubaidi F. New modified suction tip for trans nasal skull base surgery: Technical note. Interdiscip Neurosurg. 2018. 11: 68-9
3. Faraj MK, Hafidh AN, Taresh AA. Early magnetic resonance image volumetric changes of vestibular schwannoma after gamma knife radiosurgery: A prospective study of 18 cases. Egypt J Neurosurg. 2018. 33: 5
4. Faraj MK, Hoz SS, Mohammad AJ. The use of three-dimensional anatomical patient-specific printed models in surgical clipping of intracranial aneurysm: A pilot study. Surg Neurol Int. 2020. 11: 381
5. Faraj MK, Kailan SL, Al-Neami AQ. A new simple, cost-effective navigation system (EASY Navigator) for neurosurgical interventions. World Neurosurg. 2022. 164: 143-7
6. Faraj MK, Naji NA, Alazawy NM. The efficiency of the prescribed dose of the gamma knife for the treatment of trigeminal neuralgia. Interdiscip Neurosurg. 2018. 14: 9-13
7. Faraj MK, Sagban WJ. Endoscopic transsphenoidal approach to skull base lesions. A clinical prospective study. Neurosciences (Riyadh). 2018. 23: 35-8
8. Faraj MK. Programmable baclofen pump implantation as a treatment modality for spasticity: A clinical prospective study. Interdiscip Neurosurg. 2017. 10: 62-5
9. Faraj MK. Surgical treatment of Parkinson’s disease. Iraqi J Med Sci. 2015. 13: 45-50
10. Faraj MK. What are microergonomics, penization, and electronics integrated with surgical instruments?. World Neurosurg. 2021. 152: 144-51
11. Hade NA, Ramadhan RS, Faraj MK. Deformation of androgen receptor gene causing an accelerated growth of glioma in Iraqi patients. Biochem Cell Arch. 2020. 20: 155-9
12. Hade NA, Ramadhan RS, Faraj MK. Genetic polymorphism in braf gene associated with the incidence of brain tumors in a sample of Iraqi patients. Biochem Cell Arch. 2020. 20: 149-54
13. Mohammed Ali HA, Abdullah SS, Faraj MK. High impedance analysis in recordings of deep brain stimulation surgery. Interdiscip Neurosurg. 2021. 24: 101-15
14. Mohammed Ali HA, Abdullah SS, Faraj M. An in-vitro study of electrodes impedance in deep brain stimulation. J Phys. 2019. 1829: 012019
15. Moneer K, Faraj BA. Three-dimensional printing applications in the neurosurgery: A pilot study. Maced J Med Sci. 2021. 9: 403-6
16. Moneer K, Faraj BA. Treatment of primary trigeminal neuralgia: A comparative study of microvascular decompression surgery and stereotactic gamma knife radiosurgery. Int Med J. 2020. 25: 163-73