- Department of Neurosurgery, Atlanta Medical Center, Atlanta, GA, USA
- Ross University School of Medicine, Banana Trail, Portsmouth, Dominica
Correspondence Address:
Ovais Inamullah
Ross University School of Medicine, Banana Trail, Portsmouth, Dominica
DOI:10.4103/2152-7806.164694
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: King P, Khan S, Inamullah O. Astounding recovery after resection of an intradural nerve sheath tumor in an adult male from Vietnam. Surg Neurol Int 07-Sep-2015;6:145
How to cite this URL: King P, Khan S, Inamullah O. Astounding recovery after resection of an intradural nerve sheath tumor in an adult male from Vietnam. Surg Neurol Int 07-Sep-2015;6:145. Available from: http://surgicalneurologyint.com/surgicalint_articles/astounding-recovery-after-resection-of-an-intradural-nerve-sheath/
Abstract
Background:Spinal cord tumors can be classified as intramedullary, intradural extramedullary, or extradural. The differential diagnosis of spinal cord tumors includes meningiomas, astrocytomas, ependymomas, metastasis, nerve sheath tumors such as schwannomas or neurofibromas, and multiple sclerosis plaques. Radiology can provide clues to the type of tumor, but a pathology evaluation of a specimen is necessary to provide an accurate diagnosis. These tumors can cause a variety of neurological symptoms from spinal cord compression including pain, weakness, and paresthesia. They are treated by surgical resection, with a variety of outcomes possible depending on the severity of the preoperative symptoms, location and extent of the tumor, and efficacy of the surgery performed.
Case Description:A 59-year-old male from Vietnam came to the Atlanta Medical Center for evaluation of severe ride sided hemiparesis and paresthesias. He first noticed alterations in his handwriting and quickly deteriorated to the point of being unable to walk or move his right arm. A cervical spinal mass was identified and analyzed on magnetic resonance imaging. Surgical resection was performed under a microscope in a joint operation between an orthopedic surgeon and neurosurgeon. A specimen of the tumor was sent to pathology for further evaluation.
Conclusion:The mass was determined to be an intradural extramedullary schwannoma. The severity of the patient's symptoms and the location and size of the tumor made full recovery unlikely and postoperative quadriplegia a real possibility. The tumor was surgically resected, which led surprisingly, however, to a full and prompt resolution of the patient's symptoms. Less than 2 weeks after surgery, the patient was able to walk and had almost fully regained use of his hands.
Keywords: Cervical spinal cord mass, extramedullary, hemiparesis, intradural, nerve sheath tumor, schwannoma
INTRODUCTION
Tumors of the spinal cord are a rare occurrence, constituting 2–4% of central nervous system (CNS) neoplasms. The annual incidence rates for primary spinal neoplasms are reported as between 1.3 and 10/100,000.[
Extramedullary lesions, despite not infiltrating the spinal cord, can compress the spinal cord and nerve roots causing a variety of neurological symptoms including pain, weakness, and paresthesia.[
CASE REPORT
Presentation
A 59-year-old Vietnamese male presented to the Atlanta Medical Center complaining of severe posterior neck pain, right-sided hemiparesis, and right sided paresthesia. This began 4 months ago when he noticed difficulty writing and using the right hand. He had rapidly deteriorated to the point of being unable to walk or move his right arm. He had a magnetic resonance imaging (MRI) done in Vietnam, which had showed an abnormal mass in the cervical spine, which is what brought him to Dr. King at the Atlanta Medical Center.
Examination
The patient's ability to speak English was limited, but his son provided translations as necessary. The patient was alert and oriented to person, place, and time, and not invisible distress. The neurological physical exam showed significantly decreased strength in the right upper and lower extremity, as well as decreased proprioception, and light touch sensation on the right. The patient was unable to walk without assistance. Palpation of the posterior neck produced pain and paresthesia. The rest of the exam, including the complete blood count and comprehensive metabolic panel were within normal limits.
Imaging
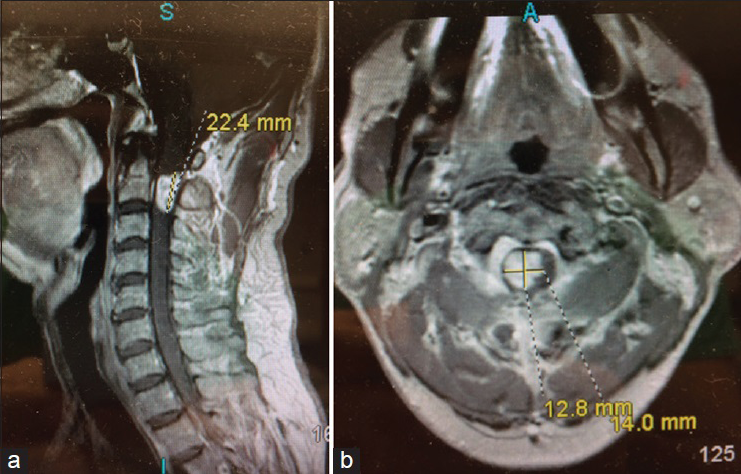
A repeat MRI with and without contrast showed an exophytic homogenously enhancing mass beginning at the C2 vertebral body level, and extending to the C2–C3 disc space, with surrounding edema within the cervical spinal cord [
The cervical spine showed normal alignment, and the rest of the spinal cord was unaffected. The differential provided by radiology was primary cervical spinal cord glioma versus metastatic lesion versus schwannoma versus neurofibroma.
Management
A laminectomy and resection were planned with possible stabilization. This would be a joint surgical procedure done by a neurosurgeon and orthopedic surgeon, using a microscope to better observe the relevant area. Risks and complications including quadriplegia, paraplegia, and respiratory dependence were explained to the patient and family.
The patient was taken to the operating suite and laid prone on the operating table with appropriate preoperative protocol directions and in a sterile fashion. An incision was made from the sub-occipital region down to C5 and then deepened down to the nuchal ligament with subperiosteal stripping of C1, C2, C3, and C4 bilaterally. The soft tissues from the remaining portions of the spine were then removed, and laminectomies were performed on C1, C2, C3, and C4. A drill was used to burrow through each side of the midline, and Rongeurs and Kerrison punches were used to complete the laminectomy. The spinous processes of C2, C3, and C4 were cut using Horsely bone cutters. Once the facet complexes were laterally removed, the dura was then palpated and opened with an 11-blade and tacked to the dural leaves to get a good retraction.
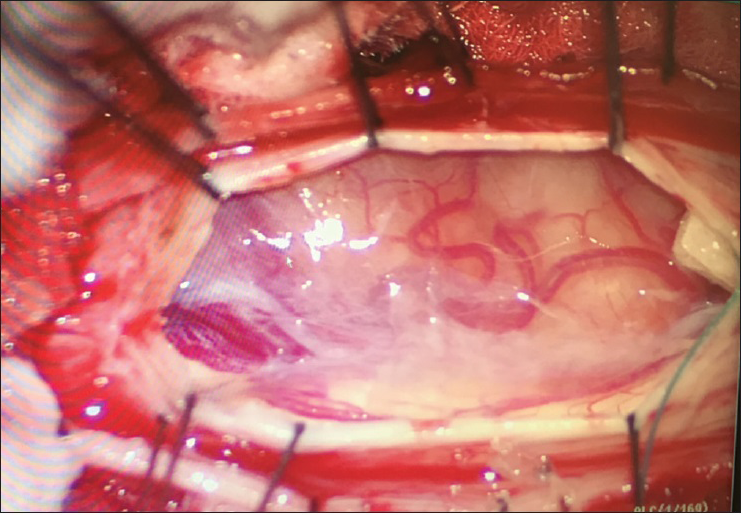
A mass was noted on the right side pushing the spinal cord and compressing it toward the left side. It was an orange pinkish mass with multiple blood vessels surrounding, and nerves were attached to the inferior lateral portion of the mass [
The dura was then closed in running fashion with a 5.0 Prolene stitch, and Evicel was placed over the dura, along with a drain in the epidural space to remove excess fluid. The wound layers were closed with vicryl and staples were placed on the skin. There were no obvious complications noted, and the patient was transferred to the Intensive Care Unit (ICU) [
The patient remained in ICU for 7 days and then transferred to a regular floor where he stayed for 5 days. He was extubated after his 2nd day in the ICU without complications. Day by day, the patient's strength in the right arm was improving, along with sensation, and strength in the right leg. The physical therapists commented on the rapid progression seen in this patient's recovery. Toward the end of his hospital stay, the patient had resolved all neurological deficits present before surgery. The patient could walk, dress himself, and feed himself with both hands. He had regained almost the entire strength of his right arm. He was discharged shortly after and returned to Vietnam.
Pathology
An intraoperative frozen consultation was done first. The limited amount of tissue prevented adequate results, but some spindling was seen, as well as other rounded cells. Some pigment was noted, representing hemosiderin. The initial differential provided was a spindle cell lesion such as meningioma or nerve sheath tumor (neurofibroma or schwannoma) versus a glial neoplasm. A nerve sheath tumor was most likely based on the location of the tumor.
Further examination of the resected tumor under a microscope showed a spindle cell lesion, with Antoni A and Antoni B are as with verocay bodies. There was no significant atypia. Glial fibrillary acidic protein stains were negative, and S100 stains were positive. These features were consistent with a schwannoma.
DISCUSSION
This case was important and valuable for a variety of reasons. It showcased the appropriate method for identifying, diagnosing, and treating the tumor in the spinal cord. Although radiology and symptoms can provide helpful hints, surgical resection, and pathological confirmation are necessary to provide an accurate diagnosis. This is a significant academic topic in the realm of neurosurgery. Other interesting aspects of this case were that the patient flew across the world from Vietnam to be seen and treated by Dr. Paul King at the Atlanta Medical Center, and that the surgical resection of the tumor was a joint operation done under a microscope by a neurosurgeon and orthopedic surgeon. The most important reason this case was unique and important, however, was the rapid extent and pace of recovery of this patient. In <2 weeks, the patient made a full neurological recovery regaining the ability to walk and use his right arm, a pace that exceeded even the most optimistic expectations.
Even if this case were more routine it is important to thoroughly investigate and analyze patients that have spinal cord tumors due to the exceedingly rare nature of these tumors. CNS tumors are <1% of tumors and spinal cord tumors account for about 3% of CNS tumors. Intradural spinal cord tumors are about two-third of spinal cord tumors, and schwannomas account for about 25% of intradural spinal cord tumors. That makes an intradural spinal cord schwannoma about 0.005% of tumors seen, an extremely rare case.
Spinal cord tumors have a broad differential that includes neurofibromas, schwannomas, meningiomas, astrocytomas, lymphoma, metastasis, and multiple sclerosis plaques. These tumors can be classified as extradural, intradural extramedullary, or intramedullary depending on their location in relation to the dura and the spinal cord itself. The most common presenting symptom is a pain,[
Although there have been major advances in the management and prognosis of intradural tumors, many patients still experience a poor postoperative outcome due to the severity of the preoperative condition and risks of surgery.[
Predictors of outcome include preoperative functional status, histologic grade of the tumor, and the extent of surgical resection.[
Based on the preoperative neurological prognosis, the rapid pace and the extent of recovery, in this case, was astounding. It was very possible that the patient would be paralyzed permanently after the procedure due to the location and size of the tumor. Due to the extent of the patient's neurological deficits, a full neurological recovery was considered unlikely. Spinal roots affected by schwannomas are often permanently nonfunctional at the time of surgery, and frequently need to be sacrificed.[
CONCLUSION
A 59-year-old male from Vietnam, complaining of right-sided hemiparesis and paresthesia, came to the Atlanta Medical Center for evaluation and treatment of cervical spinal mass that was identified on an MRI. The mass was determined to be an intradural extramedullary schwannoma. The severity of the patient's symptoms made full recovery unlikely and postoperative quadriplegia a real possibility. The tumor was surgically resected, which led surprisingly to a full and prompt resolution of the patient's symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahn DK, Park HS, Choi DJ, Kim KS, Kim TW, Park SY. The surgical treatment for spinal intradural extramedullary tumors. Clin Orthop Surg. 2009. 1: 165-72
2. Albanese V, Platania N. Spinal intradural extramedullary tumors. Personal experience. J Neurosurg Sci. 2002. 46: 18-24
3. Chamberlain MC, Tredway TL. Adult primary intradural spinal cord tumors: A review. Curr Neurol Neurosci Rep. 2011. 11: 320-8
4. Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine. 2010. 13: 67-77
5. Fernandes RL, Lynch JC, Welling L, Gonçalves M, Tragante R, Temponi V. Complete removal of the spinal nerve sheath tumors. Surgical technics and results from a series of 30 patients. Arq Neuropsiquiatr. 2014. 72: 312-7
6. Kim P, Ebersold MJ, Onofrio BM, Quast LM. Surgery of spinal nerve schwannoma. Risk of neurological deficit after resection of involved root. J Neurosurg. 1989. 71: 810-4
7. Liu WC, Choi G, Lee SH, Han H, Lee JY, Jeon YH. Radiological findings of spinal schwannomas and meningiomas: Focus on discrimination of two disease entities. Eur Radiol. 2009. 19: 2707-15
8. Parsa AT, Lee J, Parney IF, Weinstein P, McCormick PC, Ames C. Spinal cord and intradural-extraparenchymal spinal tumors: Current best care practices and strategies. J Neurooncol. 2004. 69: 291-318