- Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan.
- Department of Pathology, Juntendo University Urayasu Hospital, Urayasu, Japan.
Correspondence Address:
Satoshi Tsutsumi, Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan.
DOI:10.25259/SNI_1085_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hideaki Ueno1, Satoshi Tsutsumi1, Akane Hashizume2, Natsuki Sugiyama1, Hisato Ishii1. Atypical meningioma originating from the spinal accessory nerve. 30-Dec-2022;13:598
How to cite this URL: Hideaki Ueno1, Satoshi Tsutsumi1, Akane Hashizume2, Natsuki Sugiyama1, Hisato Ishii1. Atypical meningioma originating from the spinal accessory nerve. 30-Dec-2022;13:598. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12085
Abstract
Background: Atypical meningiomas rarely originate from the spinal accessory nerve at the C1–C2 level.
Case Description: A 57-year-old female presented with a 1-month history of headache. The cervical MR revealed a well-demarcated intradural/extramedullary tumor compressing the spinal cord at the C1–C2 level that measured 12 mm × 10 mm × 25 mm. She underwent microsurgical tumor resection. Intraoperatively, the tumor was adherent to the spinal accessory nerve, rather than the dura mater. Gross total tumor resection was performed, and the pathology was consistent with an atypical meningioma.
Conclusion: Atypical meningiomas rarely originate from the spinal accessory nerve. Gross total resection is the procedures of choice to mitigate the risk of tumor recurrence.
Keywords: Atypical meningioma, High cervical, Spinal accessory nerve, Spinal
INTRODUCTION
Spinal meningioma without apparent dural attachment has rarely been reported [
CASE PRESENTATION
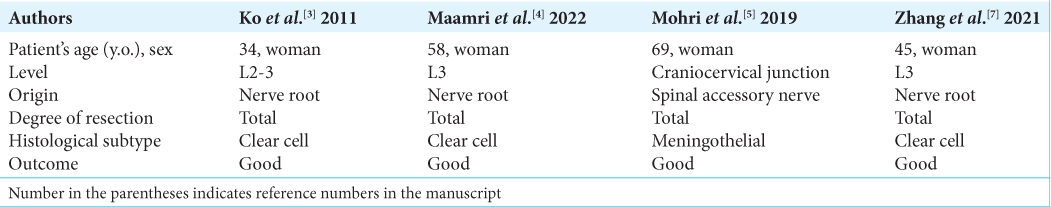
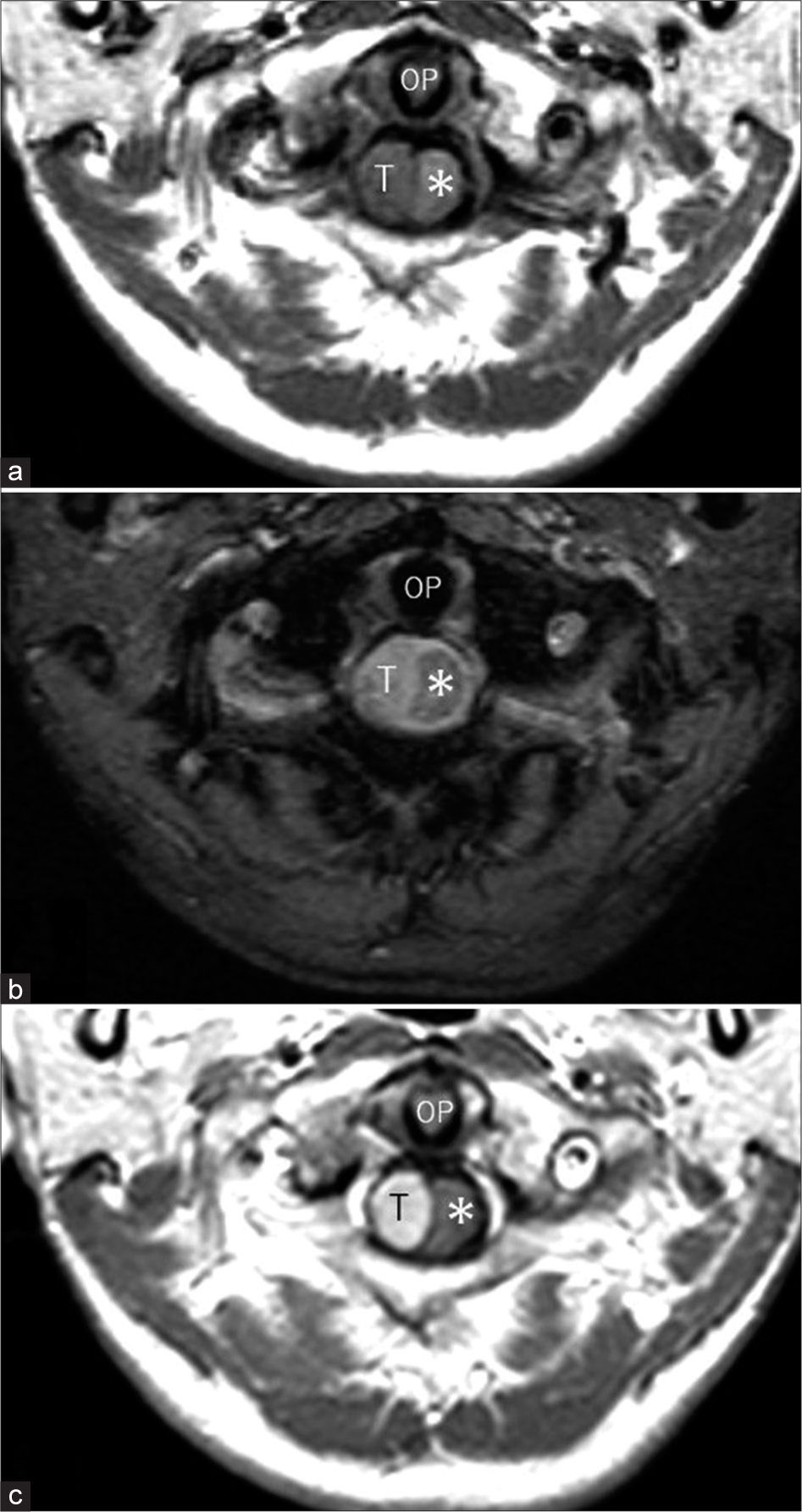
A 57-year-old female, without a history of neurofibromatosis, presented with a 1-month history of headache. The cervical magnetic resonance imaging (MR) revealed a right-sided, oval, and intradural/extramedullary lesion (i.e., 12 mm × 10 mm × 25 mm) at the C1–C2 level. The lesion was hypointense on T1- and hyperintense on T2-weighted sequences, and intensely enhanced with contrast, but showed no “dural tail” (i.e., as typically seen with meningiomas) [
Figure 1:
Axial T1- (a), T2- (b), and post-contrast axial (c) T1-weighted magnetic resonance images at the same level showing a well-demarcated extramedullary tumor (T) compressing the spinal cord from the right lateral side (asterisk). The tumor appears hypointense on T1- and hyperintense on T2-weighted sequences relative to the spinal cord, and intensely enhanced. OP: Odontoid process.
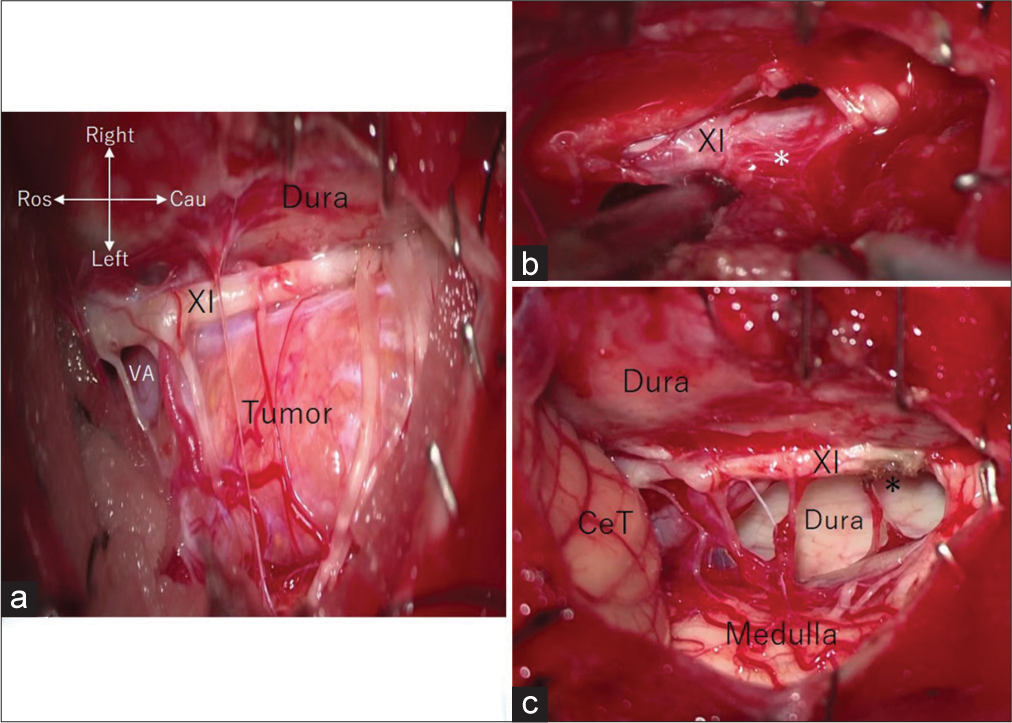
Pathology
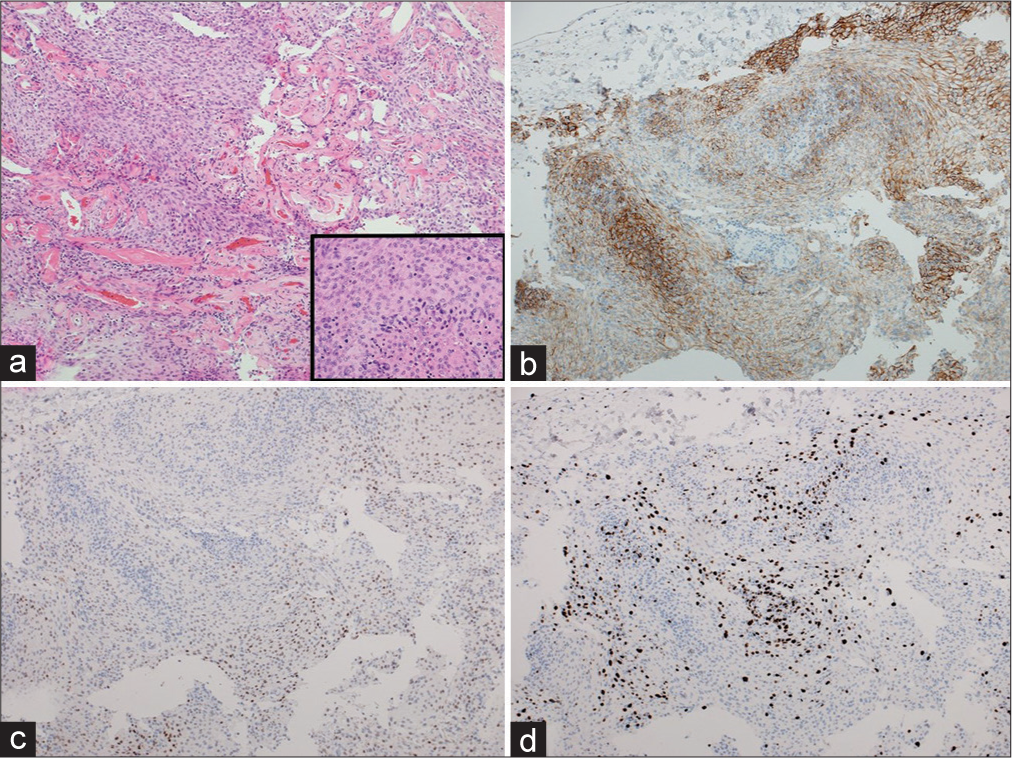
The following pathological features were consistent with an atypical meningioma; anaplastic cells with short spindle-shaped nuclei and an intervening rich vasculature, four mitotic figures per 10 high-power fields; and scattered necrotic foci [
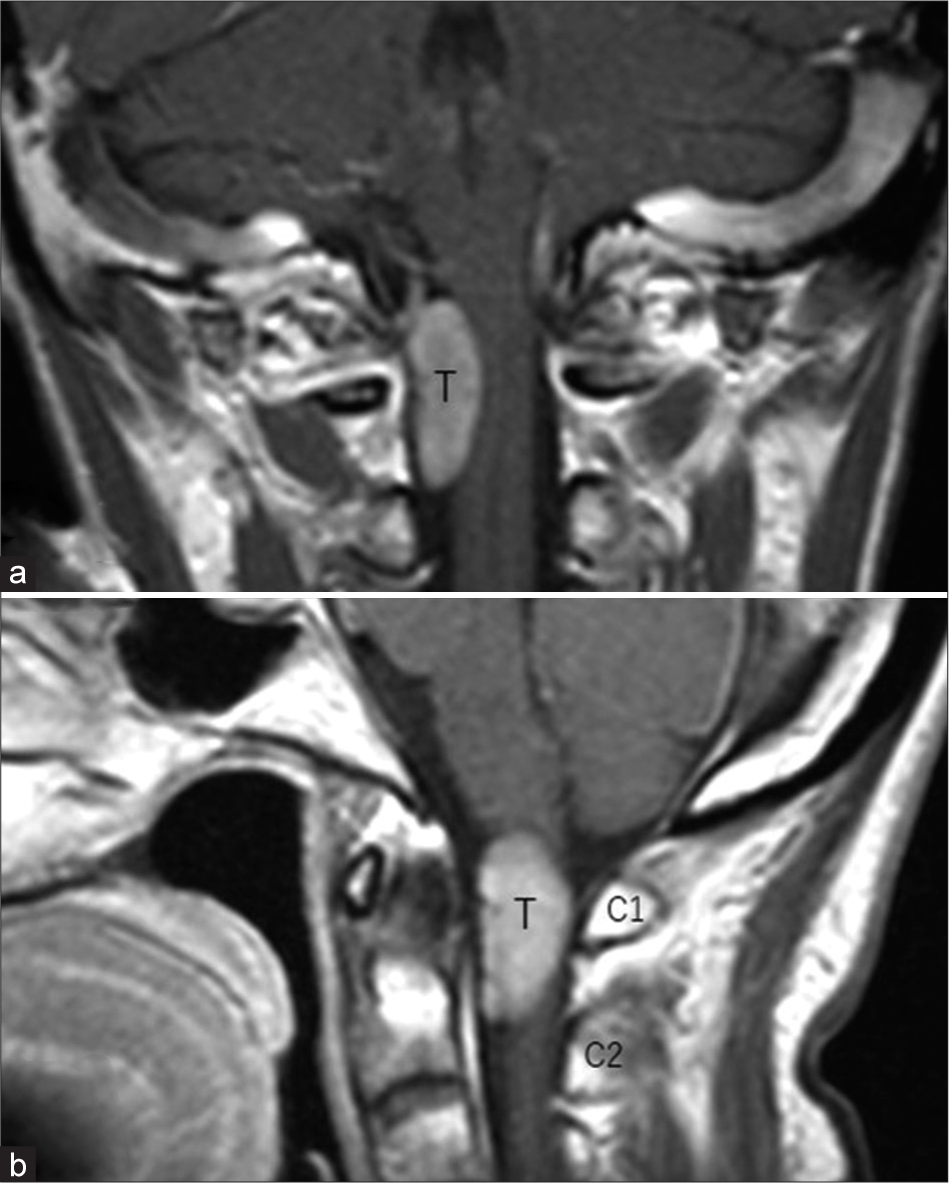
Figure 3:
Intraoperative photos showing (a) reflection of the dura mater exposing the tumor adjacent to the right spinal accessory nerve (XI) and vertebral artery (VA), (b) tumor adhesion (asterisk) to the right spinal accessory nerve (XI) exposed following partial tumor resection, and (c) post-total resection with the intact medulla, spinal accessory nerve (XI), tumor attachment site (asterisk), and the surrounding dura mater. Cau: Caudal; CeT: Cerebellar tonsil; Ros: Rostral.
Immunochemistry
The immunohistochemical examination was consistent with an atypical meningioma showing; positive staining for epithelial membrane antigen and progesterone receptors; and negative staining for glial fibrillary acidic protein. The Mindbomb Homolog-1 index was 10% [
Figure 4:
Photomicrographs of the resected specimens showing tumor tissue comprised short spindle-shaped nuclei and intervening vasculature. The magnified view of the tumor cells (a), immunohistochemical analysis showed positive staining for epithelial membrane antigen (b), and progesterone receptor (c). The Mindbomb Homolog-1 index accounted for 10% (d). (a) Hematoxylin and eosin stain, ×100; inset in (a), ×400; (b-d) ×100.
Postoperative course
The postoperative course was uneventful as the patient remained neurologically intact. Although she received no prophylactic postoperative radiotherapy, she remains under close surveillance with MRI scans repeated every 6 months looking for tumor recurrence.
DISCUSSION
Original of spinal meningiomas
Most spinal meningiomas develop as dural-based and intradural extramedullary tumors.[
Recommendation for gross total excision for atypical spinal meningiomas to achieve the best long-term prognosis
Spinal atypical meningiomas are typically aggressive lesions with a poor prognosis, and, therefore, warrant aggressive treatment.[
CONCLUSION
Atypical meningiomas can originate from the spinal accessory nerve. Timely, surgery with gross total removal results in the best long-term outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bayoumi AB, Laviv Y, Karaali CN, Ertilav K, Kepoglu U, Toktas ZO. Spinal meningiomas: 61 cases with predictors of early postoperative surgical outcomes. J Neurosurg Sci. 2020. 64: 446-51
2. Kawaguchi Y, Ishihara H, Abe Y, Seki S, Tokunaga A, Urushizaki A. Fatal prognosis of an atypical meningioma in the cervical spine. J Orthop Sci. 2008. 13: 155-9
3. Ko JK, Choi BK, Cho WH, Choi CH. Non-dura based intraspinal clear cell meningioma. J Korean Neurosurg Soc. 2011. 49: 71-4
4. Maamri K, Taieb MA, Trifa A, Elkahla G, Njima M, Darmoul M. Spinal clear cell meningioma without dural attachment: A case report and literature review. Radiol Case Rep. 2022. 17: 1760-4
5. Mohri M, Yamano J, Saito K, Nakada M. Spinal accessory nerve meningioma at the foramen magnum with medullary compression: A case report and literature review. World Neurosurg. 2019. 128: 158-61
6. Roux FX, Nataf F, Pinaudeau M, Borne G, Devaux B, Meder JF. Intraspinal meningiomas: Review of 54 cases with discussion of poor prognosis factors and modern therapeutic management. Surg Neurol. 1996. 46: 458-64
7. Zhang X, Zhang P, Wang JJ, Dong S, Wu Y, Zhang H. Intraspinal clear cell meningioma without dural attachment: A case report and literature review. Medicine (Baltimore). 2021. 100: e25167