- Department of Neurosurgery, Kumamoto University Hospital, Kumamoto, Japan.
- Department of Metabolic Medicine, Kumamoto University Hospital, Kumamoto, Japan.
- Department of Diagnostic Pathology, Kumamoto University Hospital, Kumamoto, Japan.
Correspondence Address:
Naoki Shinojima, Department of Neurosurgery, Kumamoto University Hospital, Kumamoto, Japan.
DOI:10.25259/SNI_835_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tatsuya Kawano1, Naoki Shinojima1, Satoko Hanatani2, Eiichi Araki2, Yoshiki Mikami3, Akitake Mukasa1. Atypical pituitary abscess lacking rim enhancement and diffusion restriction with an unusual organism, Moraxella catarrhalis: A case report and review of the literature. 20-Dec-2021;12:617
How to cite this URL: Tatsuya Kawano1, Naoki Shinojima1, Satoko Hanatani2, Eiichi Araki2, Yoshiki Mikami3, Akitake Mukasa1. Atypical pituitary abscess lacking rim enhancement and diffusion restriction with an unusual organism, Moraxella catarrhalis: A case report and review of the literature. 20-Dec-2021;12:617. Available from: https://surgicalneurologyint.com/surgicalint-articles/11300/
Abstract
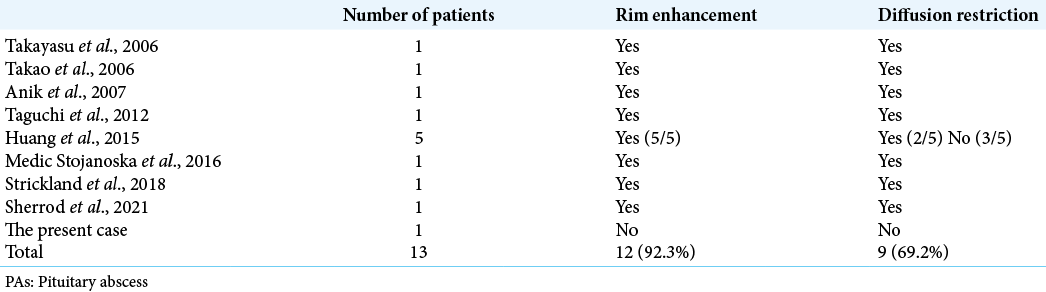
Background: Pituitary abscess (PA) can be fatal if diagnosed late. Rim enhancement is a typical radiological finding of PA on postgadolinium T1-weighted magnetic resonance imaging (MRI). Diffusion-weighted imaging is helpful in distinguishing PA from other sellar cystic lesions. Herein, we report the first atypical case of PA showing neither rim enhancement nor diffusion restriction with an unusual organism, Moraxella catarrhalis.
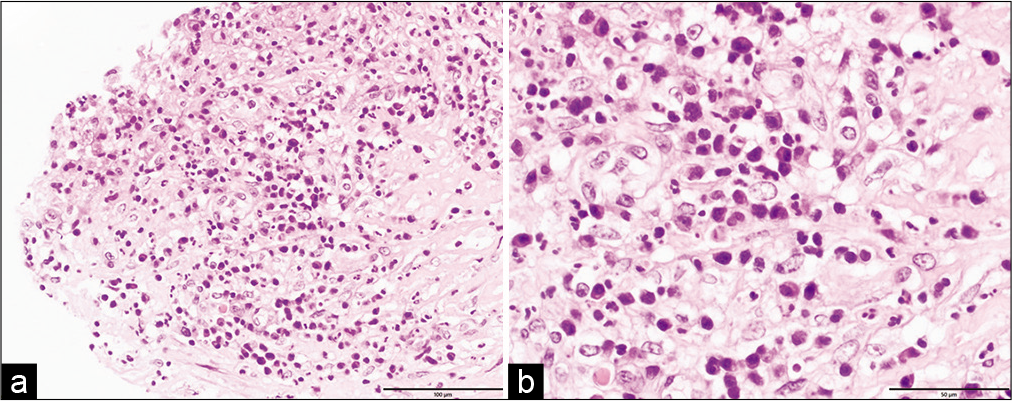
Case Description: A 77-year-old woman presented with headache, polyuria, polydipsia, and fatigue for a month before presenting to a local hospital. MRI showed pituitary enlargement with contrast enhancement. She had neither fever nor visual deficits and was followed up with hormonal replacement. Six months later, she complained of visual impairment, and MRI showed further pituitary enlargement with a thickened stalk compressing the optic chiasma. Neither rim enhancement nor diffusion restriction was observed. Endoscopic endonasal transsphenoidal surgery was performed based on the radiological diagnosis of lymphocytic hypophysitis or pituitary tumors. A thick, creamy yellow pus was drained from the sellar lesion. Intraoperative rapid histopathological findings revealed polymorphonuclear leukocytes infiltrating the pituitary gland. PA was diagnosed, and irrigation and open drainage of the abscess was performed. Bacterial culture of the pus detected M. catarrhalis by mass spectrometer, confirming the diagnosis. She underwent appropriate antibiotic administration, and her visual deficits improved.
Conclusion: We report the first atypical case of PA showing neither rim enhancement nor diffusion restriction with M. catarrhalis. Even if preoperative findings are not suggestive of PA, it should be considered as a differential diagnosis. Intraoperative rapid histopathological findings are useful for accurately diagnosing PA and initiating appropriate surgical treatment.
Keywords: Diffusion-weighted imaging, Intraoperative rapid histopathological findings, Moraxella catarrhalis, Pituitary abscess, Rim enhancement
INTRODUCTION
Pituitary abscess (PA) was first described by Simmonds in 1914.[
CASE REPORT
A 77-year-old woman presented to a local hospital with headache, polyuria, polydipsia, and fatigue for a month, but had no fever. Her laboratory studies showed panhypopituitarism without inflammatory findings such as an increase in white blood cells or C-reactive protein. MRI showed a 15 mm enlarged pituitary gland with heterogeneous contrast enhancement. She was referred to our hospital, where an ophthalmological evaluation showed normal visual acuity and no visual field disturbance. She was started on hormonal replacement therapy and was followed up.
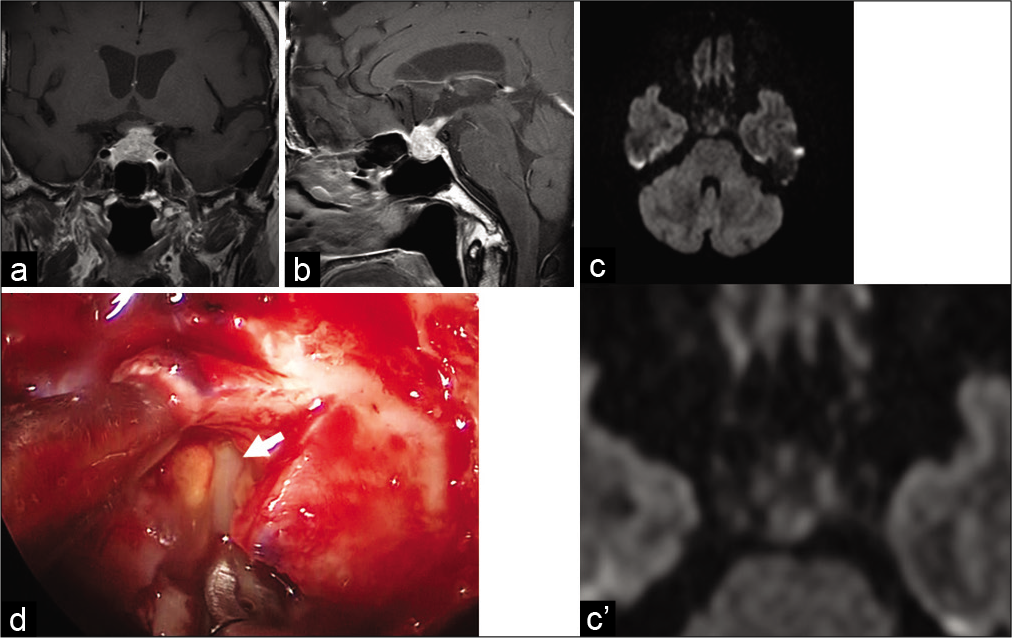
Six months later, she had blurred vision in the left eye, and an ophthalmological evaluation showed a decrease in visual acuity with bitemporal hemianopia. MRI showed further pituitary enlargement with thickening of the pituitary stalk compressing the optic chiasma and a positive dural tail sign. Neither ring enhancement nor diffusion restriction was observed [
Figure 1:
Brain magnetic resonance imaging scans. (a) Coronal postgadolinium T1-weighted image, (b) sagittal postgadolinium T1-weighted image, (c) axial diffusion-weighted image, and (c’) the enlarged pituitary part of diffusion-weighted image of c. (a-c’) Magnetic resonance imaging showing pituitary enlargement with heterogeneous enhancement and thickened pituitary stalk compressing the optic chiasma. There is no high signal on diffusion-weighted imaging, indicating lack of diffusion restriction. (d) Yellow and creamy pus observed intraoperatively (arrow).
Endoscopic endonasal transsphenoidal surgery was performed, and a thick, creamy yellow pus was drained out of the sellar lesion [
Figure 3:
Brain magnetic resonance imaging scans. (a) Coronal postgadolinium T1-weighted image, (b) sagittal postgadolinium T1-weighted image, (c) sagittal diffusion-weighted image. (a-c) Postoperative magnetic resonance imaging showing no apparent change from preoperative magnetic resonance imaging (MRI) scan. There is no high signal on diffusion-weighted imaging as same as preoperative MRI scan.
DISCUSSION
PA can be a life-threatening condition and is associated with high mortality rates.[
DWI is useful for the differential diagnosis of PA, other sellar cystic lesions,[
The development of PA is thought to be due to hematogenous dissemination[
Intracranial infections caused by Moraxella are very rare, and there have been few reports of intracerebral abscesses caused by M. catarrhalis.[
To the best of our knowledge, this is the first case of PA affected by M. catarrhalis. In our case, the atypical MRI findings of PA, in addition to the abscess stage, may be related to this rare organism.
CONCLUSION
PA is rare and potentially life threatening if not promptly treated. However, its correct diagnosis is challenging. Our case reveals that PA can present without rim enhancement and diffusion restriction and M. catarrhalis can be an organism of PA. Therefore, even if PA is not suggested preoperatively, it is necessary to consider it as a possible diagnosis. Finally, intraoperative rapid histopathological findings are useful for determining the correct diagnosis of PA and instituting appropriate surgical treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anik Y, Koc K, Anik I, Meric M, Demirci A. Diffusion weighted MRI of primary pituitary abscess. Case report. Neuroradiol J. 2007. 20: 282-6
2. Burdette JH, Elster AD, Ricci PE. Acute cerebral infarction: Quantification of spin-density and T2 shine-through phenomena on diffusion-weighted MR images. Radiology. 1999. 212: 333-9
3. Dutta P, Bhansali A, Singh P. Pituitary abscess: Report of four cases and review of literature. Pituitary. 2006. 9: 267-73
4. Dalan R, Leow MK. Pituitary abscess: Our experience with a case and a review of the literature. Pituitary. 2008. 11: 299-306
5. Erdogan G, Deda H, Tonyukuk V. Magnetic resonance imaging and computerized tomography images in a case of pituitary abscess. J Endocrinol Invest. 2001. 24: 887-91
6. Falcone S, Post MJ. Encephalitis, cerebritis, and brain abscess: Pathophysiology and imaging findings. Neuroimaging Clin N Am. 2000. 10: 333-53
7. Gao L, Guo X, Tian R, Wang Q, Feng M, Bao X. Pituitary abscess: Clinical manifestations, diagnosis and treatment of 66 cases from a large pituitary center over 23 years. Pituitary. 2017. 20: 189-94
8. Haimes AB, Zimmermann RS, Morgello S, Weingarten K, Becker RD, Jennis R. MR imaging of brain abscess. AJR Am J Roentgenol. 1989. 152: 1073-85
9. Huang KT, Bi WL, Smith TR, Zamani AA, Dunn IF, Laws ER. Intrasellar abscess following pituitary surgery. Pituitary. 2015. 18: 731-7
10. Kotani H, Abiru H, Miyao M, Kakimoto Y, Kawai C, Ozeki M. Pituitary abscess presenting a very rapid progression: Report of a fatal case. Am J Forensic Med Pathol. 2012. 33: 280-3
11. Levinson W.editors. Medical Microbiology and Immunology. New York: McGraw Hill; 1998. p.
12. Medic Stojanoska M, Kozic D, Bjelan M, Vulekovic P, Vuckovic N, Vukovic B, Kovacev Zavisic B. Pituitary abscess with unusual clinical course. Acta Clin Croat. 2016. 55: 650-4
13. Obrador S, Blazquez MG. Pituitary abscess in a craniopharyngioma. Case report. J Neurosurg. 1972. 36: 785-9
14. Ramakrishna R, Nair MN, Huber B, Sekhar LN. A rare case of recurrent frontal osteoma complicated by mucopyocele with an unusual organism, Moraxella catarrhalis. World Neurosurg. 2014. 82: 240.e13-9
15. Sabbah P, Bonardel G, Herve R, Marjou F, Hor F, Pharaboz C. CT and MRI findings in primitive pituitary abscess: A case report and review of literature. J Neuroradiol. 1999. 26: 196-9
16. Sherrod BA, Makarenko S, Iyer RR, Eli I, Kestle JR, Couldwell WT. Primary pituitary abscess in an adolescent female patient: Case report, literature review, and operative video. Childs Nerv Syst. 2021. 37: 1423-8
17. Simmonds M. On embolic processes in the pituitary gland. Virchows Arch Path Anat. 1914. 217: 226-39
18. Strickland BA, Pham M, Bakhsheshian J, Carmichael J, Weiss M, Zada G. Endoscopic endonasal transsphenoidal drainage of a spontaneous candida glabrata pituitary abscess. World Neurosurg. 2018. 109: 467-70
19. Taguchi Y, Yoshida K, Takashima S, Tanaka K. Diffusion-weighted MRI findings in a patient with pituitary abscess. Intern Med. 2012. 51: 683
20. Takao H, Doi I, Watanabe T. Diffusion-weighted magnetic resonance imaging in pituitary abscess. J Comput Assist Tomogr. 2006. 30: 514-6
21. Takayasu T, Yamasaki F, Tominaga A, Hidaka T, Arita K, Kurisu K. A pituitary abscess showing high signal intensity on diffusion-weighted imaging. Neurosurg Rev. 2006. 29: 246-8
22. Vates GE, Berger MS, Wilson CB. Diagnosis and management of pituitary abscess: A review of twenty-four cases. J Neurosurg. 2001. 95: 233-41
23. Viagappan GM, Cudlip S, Lee PY, Kitchens N, Bell BA. Brain abscess caused by infection with Moraxella catarrhalis following a penetrating injury. J Infect. 1998. 36: 130-1
24. Wang Z, Gao L, Zhou X, Guo X, Wang Q, Lian W. Magnetic resonance imaging characteristics of pituitary abscess: A review of 51 cases. World Neurosurg. 2018. 114: e900-12
25. Xu XX, Li B, Yang HF, Du Y, Li Y, Wang WX. Can diffusion-weighted imaging be used to differentiate brain abscess from other ring-enhancing brain lesions? A meta-analysis. Clin Radiol. 2014. 69: 909-15
26. Zhang X, Sun J, Shen M, Shou X, Qiu H, Qiao N. Diagnosis and minimally invasive surgery for the pituitary abscess: A review of twenty nine cases. Clin Neurol Neurosurg. 2012. 114: 957-61
27. Zimmerman RD, Weingarten K. Neuroimaging of cerebral abscesses. Neuroimaging Clin North Am. 1991. 1: 1-16