- Long School of Medicine, University of Texas Health San Antonio, San Antonio, Texas, United States.
- Department of Neurosurgery, University of Texas Health San Antonio, San Antonio, Texas, United States.
Correspondence Address:
Mehdi Siddiqui
Department of Neurosurgery, University of Texas Health San Antonio, San Antonio, Texas, United States.
DOI:10.25259/SNI-59-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mehdi Siddiqui, Dewey Thoms, Derek Samples, Jean Caron. Atypical teratoid/rhabdoid tumor presenting with subarachnoid and intraventricular hemorrhage. 05-Jul-2019;10:139
How to cite this URL: Mehdi Siddiqui, Dewey Thoms, Derek Samples, Jean Caron. Atypical teratoid/rhabdoid tumor presenting with subarachnoid and intraventricular hemorrhage. 05-Jul-2019;10:139. Available from: https://surgicalneurologyint.com/surgicalint-articles/9456/
Abstract
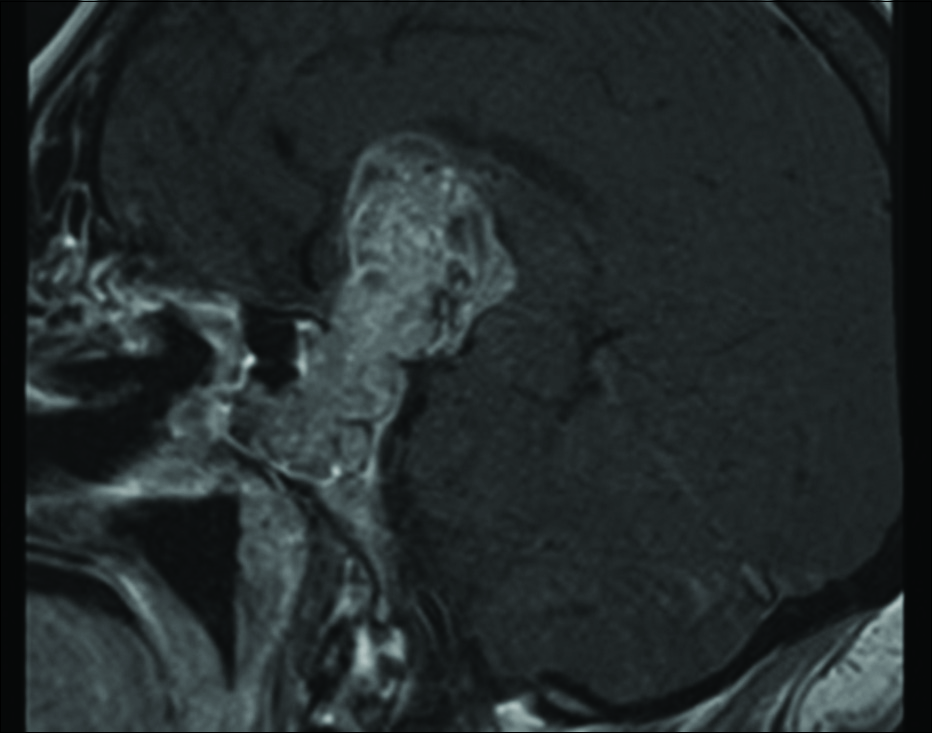
Background: Sellar masses comprise 14–18% of all intracranial tumors. Pituitary adenomas account for 85% of these lesions, while 15% of sellar masses stem from other etiologies. Intratumoral hemorrhage (apoplexy), while not exceptionally common, can be discovered at presentation. While the hemorrhage pattern is typically contained within the tumor, an extension of bleeding beyond the sella has been reported.
Case Description: A 55-year-old female presented with an anterior interhemispheric subarachnoid hemorrhage and extensive intraventricular hemorrhage (IVH). Initially, the IVH was thought to be due to a ruptured aneurysm. After further workup, a hemorrhagic sellar mass was diagnosed. The patient underwent transsphenoidal resection of a pituitary adenoma. The patient returned to the emergency department6 weeks later with an atypical rapidly expanding sellar mass. After tumor debulking, the pathology revealed an atypical teratoid/rhabdoid tumor (ATRT). Here, we reviewed this and other such cases of sellar ATRT.
Conclusion: The early diagnosis of sellar ATRT with lack of integrase interactor 1 expression and elevated Ki67 proliferation indices can prompt more aggressive attempted gross total resection, chemotherapy, and radiation treatments.
Keywords: Atypical teratoid/rhabdoid tumor, Intraventricular hemorrhage, Sellar mass
INTRODUCTION
Sellar masses occur in 0.1% of the population and represent 14–18% of intracranial tumors. Hemorrhage is an uncommon finding, only occurring in 1.6–2.8% of pituitary adenomas which account for 85% of sellar tumors.[
CASE REPORT
A 55-year-old female presented with 1 week of headache, blurred vision, and the acute onset of altered mental status. On examination, she opened her eyes to voice, followed commands in all four extremities, and had a slight right hemiparesis. She also exhibited panhypopituitarism and hypernatremia secondary to diabetes insipidus.
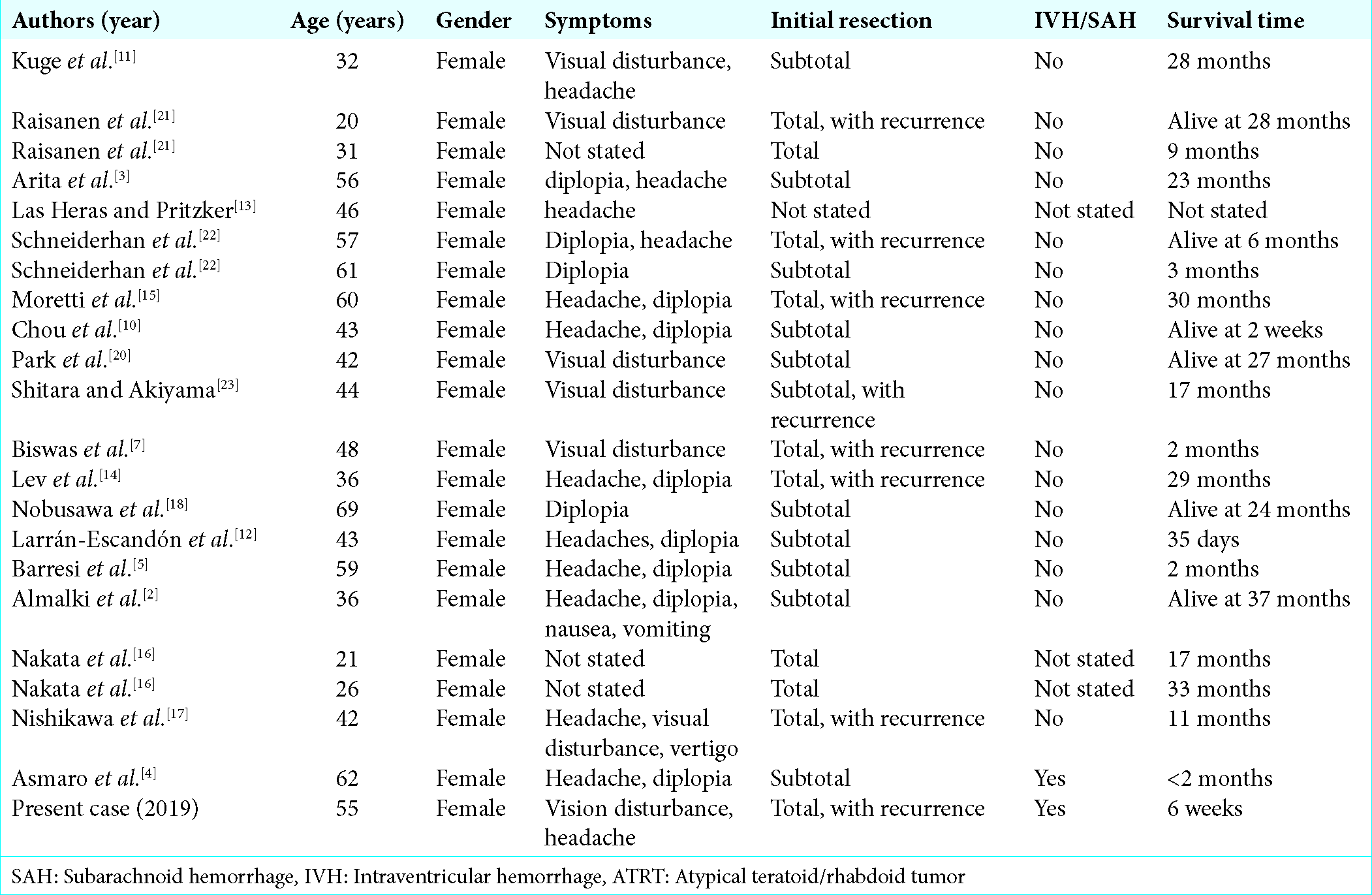
Computer tomography and magnetic resonance findings
The brain computer tomography (CT) revealed a suprasellar cistern and anterior interhemispheric SAH with IVH; this required placement of a right ventricular drain [
Figure 1:
(a) Axial noncontrast head computer tomography showing significant bilateral frontal horn, third and fourth ventricular hemorrhage. (b) Sagittal noncontrast head computer tomography showing third and fourth ventricular hemorrhage. The lateral ventricles are not well visualized here, but some intraventricular hemorrhage is still seen.
Computer tomography and cerebral angiography
The CT angiogram suggested a 3 mm right supraclinoid internal carotid artery aneurysm. Two cerebral angiograms performed 3 days later showed incidental pathology (e.g., 2 mm left middle cerebral artery bifurcation aneurysm; left anterior choroidal artery aneurysm; and a 2 mm right paraophthalmic aneurysm), which was not considered to be contributing to her symptomatology.
Surgery
Transsphenoidal resection of the pituitary mass and evacuation of the sellar hematoma were undertaken. The frozen and permanent pathology was negative for hormonal stains. She was, therefore, originally diagnosed as having a pituitary adenoma with apoplexy and recovered within weeks without a persistent neurological deficit.
Six-week postoperative readmission
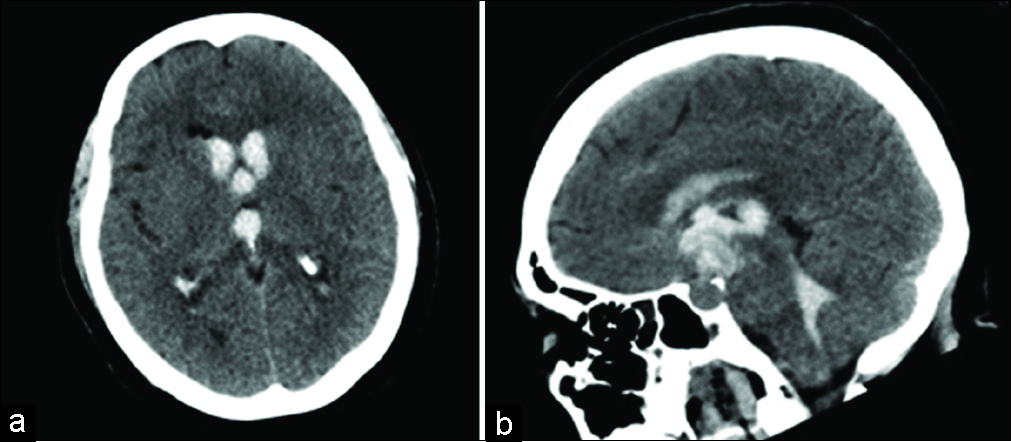
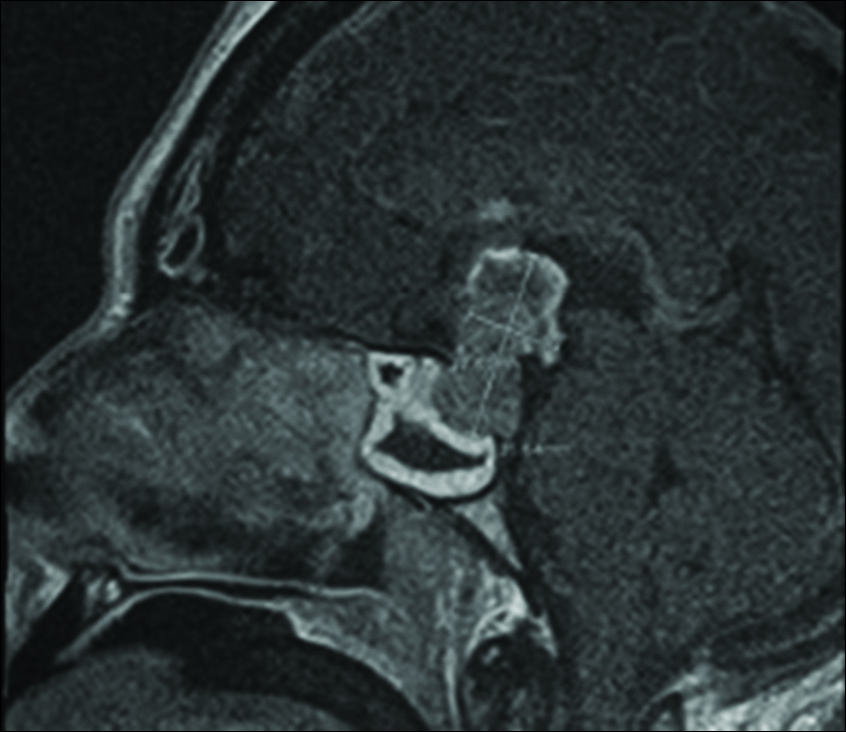
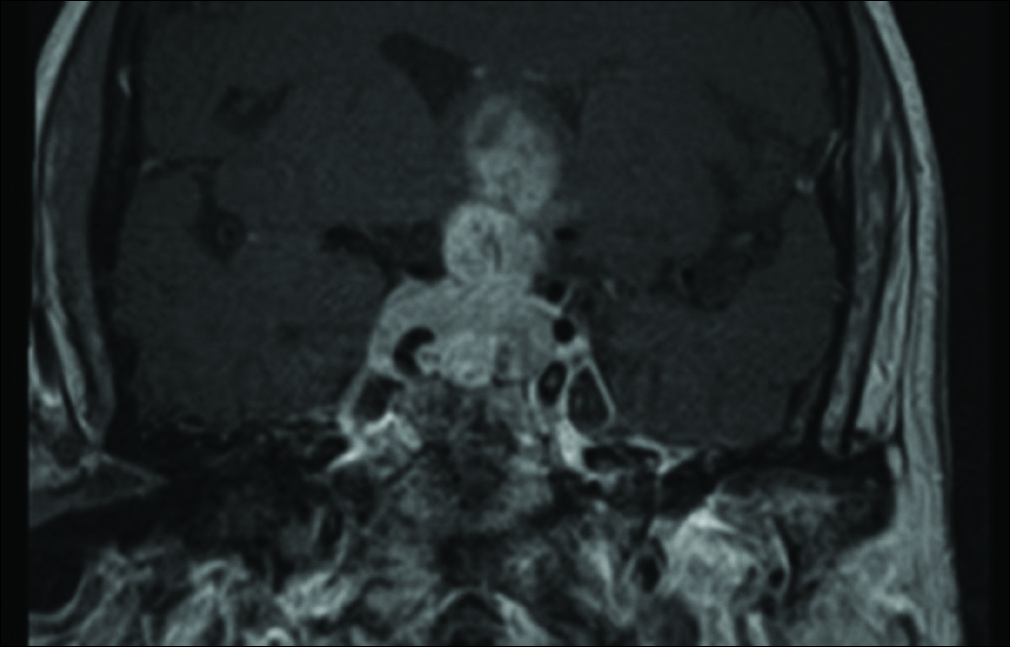
Six weeks later, however, she developed worsening of the headaches accompanied by visual loss. The MRI now showed a significant interval increase in the size of the sellar/suprasellar enhancing mass with the invasion of the cavernous sinus and encasement of the internal carotid arteries bilaterally [
DISCUSSION
ATRT typically is a central nervous system tumor, most commonly found in the posterior fossa.[
Behavior of sellar atypical teratoid/rhabdoid tumor
Sellar ATRT rapidly recurs after transsphenoidal resection; this also occurred in our patient. Of the previously reported adult sellar/suprasellar ATRT cases, only one presented with SAH and IVH[
Radiographic presentation of sellar atypical teratoid/ rhabdoid tumor on magnetic resonance
On MR, sellar ATRT invades the suprasellar space and cavernous sinus. The tumor in our patient showed moderate enhancement throughout most of the mass, including increased dorsal heterogeneous enhancement. Typically, on MR scans, these tumors demonstrate heterogeneous enhancement with peripherally located cysts.
Radiographic presentation of sellar atypical teratoid/ rhabdoid tumor on computer tomography
On CT, Biswas et al. described ATRT as hyperdense lesions with heterogeneous enhancement, and calcifications (40%).[
Pathology of atypical teratoid/rhabdoid tumor
Key distinguishing features of ATRT are an elevated Ki67 proliferation index, and the loss of INI1 protein expression due to partial deletion of chromosome 22 (e.g., which contains the SMARCB1 gene). The latter two findings were noted in our patient’s pathology report.[
Treatment of atypical teratoid/rhabdoid tumor
At present, there is no standard treatment for sellar ATRT. Although various therapies have been attempted including resection, radiation, and chemotherapy, they have been met with varying success and are largely based on pediatric protocols.[
CONCLUSION
A 55-year-old female acutely presented with a sellar ATRT characterized by both a subarachnoid and IVH. Although the initial diagnosis was pituitary apoplexy attributed to an adenoma, the secondary bleed led to further histopathological confirmation of an ATRT (e.g., INI1 expression and elevated Ki67 proliferation index).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Dahmani K, Mohammad S, Imran F, Theriault C, Doucette S, Zwicker D. Sellar masses: An epidemiological study. Can J Neurol Sci. 2016. 43: 291-7
2. Almalki MH, Alrogi A, Al-Rabie A, Al-Dandan S, Altwairgi A, Orz Y. Atypical teratoid/Rhabdoid tumor of the sellar region in an adult with long survival: Case report and review of the literature. J Clin Med Res. 2017. 9: 216-20
3. Arita K, Sugiyama K, Sano T, Oka H. Atypical teratoid/ rhabdoid tumour in sella turcica in an adult. Acta Neurochir (Wien). 2008. 150: 491-5
4. Asmaro K, Arshad M, Massie L, Griffith B, Lee I. Sellar atypical teratoid/Rhabdoid tumor presenting with subarachnoid and intraventricular hemorrhage. World Neurosurg. 2019. 123: e31-e38
5. Barresi V, Lionti S, Raso A, Esposito F, Cannavò S, Angileri FF. Pituitary atypical teratoid rhabdoid tumor in a patient with prolactinoma: A unique description. Neuropathology. 2018. 38: 260-7
6. Biswas A, Kashyap L, Kakkar A, Sarkar C, Julka PK. Atypical teratoid/rhabdoid tumors: Challenges and search for solutions. Cancer Manag Res. 2016. 8: 115-25
7. Biswas S, Wood M, Joshi A, Bown N, Strain L, Martinsson T. Exome sequencing of an adult pituitary atypical teratoid rhabdoid tumor. Front Oncol. 2015. 5: 236-
8. Boellis A, di Napoli A, Romano A, Bozzao A. Pituitary apoplexy: An update on clinical and imaging features. Insights Imaging. 2014. 5: 753-62
9. Chan V, Marro A, Findlay JM, Schmitt LM, Das S. A systematic review of atypical teratoid rhabdoid tumor in adults. Front Oncol. 2018. 8: 567-
10. Chou S, Lo S, Wong H, Lau P, Chan C, Tang K. Atypical teratoid/rhabdoid tumour in the sella turcica of a female adult. Hong Kong J Radiol. 2013. 16: 65-8
11. Kuge A, Kayama T, Tsuchiya D, Kawakami K, Saito S, Nakazato Y. Suprasellar primary malignant rhabdoid tumor in an adult: A case report. No Shinkei Geka. 2000. 28: 351-8
12. Larrán-Escandón L, Mateo-Gavira I, Vilchez-López FJ, Gómez Cárdenas E, Aguilar Diosdado M. Pituitary apoplexy as presentation of atypical teratoid/rhabdoid tumor in an adult. Endocrinol Nutr. 2016. 63: 364-5
13. Las Heras F, Pritzker KP. Adult variant of atypical teratoid/ rhabdoid tumor: Immunohistochemical and ultrastructural confirmation of a rare tumor in the sella tursica. Pathol Res Pract. 2010. 206: 788-91
14. Lev I, Fan X, Yu R. Sellar atypical teratoid/rhabdoid tumor: Any preoperative diagnostic clues?. AACE Clin Case Rep. 2015. 1: e2-7
15. Moretti C, Lupoi D, Spasaro F, Chioma L, Di Giacinto P, Colicchia M. Sella turcica atypical teratoid/rhabdoid tumor complicated with lung metastasis in an adult female. Clin Med Insights Case Rep. 2013. 6: 177-82
16. Nakata S, Nobusawa S, Hirose T, Ito S, Inoshita N, Ichi S. Sellar atypical teratoid/Rhabdoid tumor (AT/RT): A Clinicopathologically and genetically distinct variant of AT/ RT. Am J Surg Pathol. 2017. 41: 932-40
17. Nishikawa A, Ogiwara T, Nagm A, Sano K, Okada M, Chiba A. Atypical teratoid/rhabdoid tumor of the sellar region in adult women: Is it a sex-related disease?. J Clin Neurosci. 2018. 49: 16-21
18. Nobusawa S, Nakata S, Hirato J, Kawashima T, Sato K, Fujimaki H. Atypical teratoid/rhabdoid tumor in the sella turcica of an elderly female with a distinct vascular pattern and genetic alterations. Virchows Arch. 2016. 469: 711-5
19. Ojeda-Schuldt MBLarran-Escandon LMateo-Gavira IVilchez-Lopez FJGavilan-Villarejo IAguilar-Diosdado M. Available from: http://www.endocrine-abstracts.org/ea/0037/ea0037EP1181.htm [Last accessed on 2019 Apr 19].
20. Park HG, Yoon JH, Kim SH, Cho KH, Park HJ, Kim SH. Adult-onset sellar and suprasellar atypical teratoid rhabdoid tumor treated with a multimodal approach: A case report. Brain Tumor Res Treat. 2014. 2: 108-13
21. Raisanen J, Biegel JA, Hatanpaa KJ, Judkins A, White CL, Perry A. Chromosome 22q deletions in atypical teratoid/ rhabdoid tumors in adults. Brain Pathol. 2005. 15: 23-8
22. Schneiderhan TM, Beseoglu K, Bergmann M, Neubauer U, Macht S, Hänggi D. Sellar atypical teratoid/rhabdoid tumours in adults. Neuropathol Appl Neurobiol. 2011. 37: 326-9
23. Shitara S, Akiyama Y. Atypical teratoid/rhabdoid tumor in sellar turcica in an adult: A case report and review of the literature. Surg Neurol Int. 2014. 5: 75-