- Department of Orthopedics, Hospital Español, Mendoza, Argentina,
- Department of Orthopedics, Hospital Churruca Visca, Argentina
- Department of Neurosurgery, Hospital Clinico Regional, Concepcion, Chile,
- Department of Neurosurgery, Hospital Español de La Plata, La Plata, Argentina
- Department of Orthopedics, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina,
- Department of Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil.
Correspondence Address:
Alfredo Guiroy
Department of Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil.
DOI:10.25259/SNI_44_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alfredo Guiroy, Marcelo Valacco, Martin Gagliardi, Juan Pablo Cabrera, Juan Emmerich, Gaston Camino Willhuber, Asdrubal Falavigna. Barriers of neurophysiology monitoring in spine surgery: Latin America experience. 30-May-2020;11:130
How to cite this URL: Alfredo Guiroy, Marcelo Valacco, Martin Gagliardi, Juan Pablo Cabrera, Juan Emmerich, Gaston Camino Willhuber, Asdrubal Falavigna. Barriers of neurophysiology monitoring in spine surgery: Latin America experience. 30-May-2020;11:130. Available from: https://surgicalneurologyint.com/surgicalint-articles/10057/
Abstract
Background: Intraoperative neurophysiological monitoring (IOM) has become valuable in spine surgery. Unfortunately, it is not always available in many spine centers, especially in developing countries. Our aim was to evaluate the accessibility and barriers to IOM in spine surgery in Latin America.
Methods: We designed a questionnaire to evaluate the characteristics of surgeons and their opinions on the usefulness of IOM for different spine operations. The survey was sent to 9616 members and registered users of AO Spine Latin America (AOSLA) from August 1, 2019, to August 21, 2019. Major variables studied included nationality, years of experience, specialty (orthopedics or neurosurgery), level of complexity of the hospital, number of spine surgeries performed per year by the spine surgeon, the types of spinal pathologies commonly managed, and how important IOM was to the individual surgeon. General questions to evaluate use included accessibility, limitations of IOM usage, management of IOM changes, and the legal value of IOM. The results were analyzed and compared between neurosurgeon and orthopedics, level of surgeon experience, and country of origin.
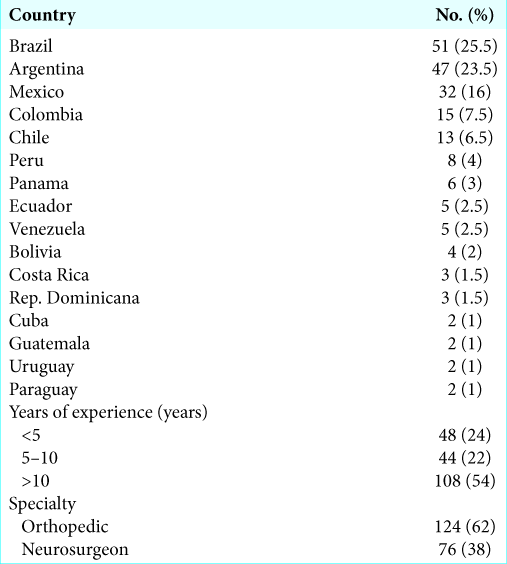
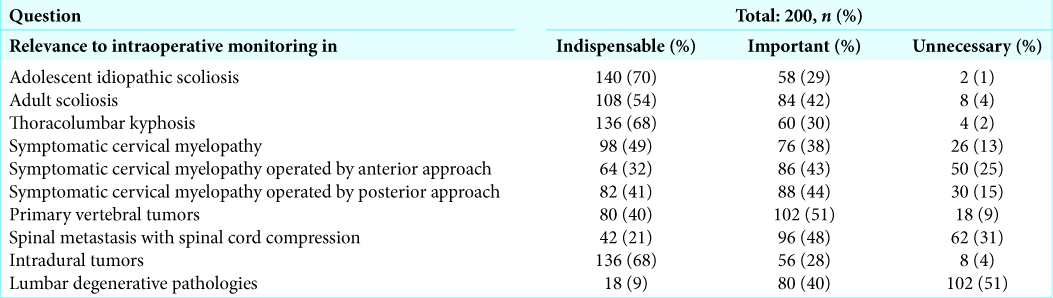
Results: Questionnaires were answered by 200 members of AOSLA from 16 different countries. The most common responses were obtained from orthopedic surgeons (62%), those with more than 10 years of practice (54%); majority of surgeons performed more than 50 spine surgeries per year (69%) and treated mainly spine degenerative diseases (76%). Most surgeons think that IOM has a real importance during surgeries (92%) and not just a legal value. Although surgeons mostly considered IOM essential to scoliosis surgery in adolescents (70%), thoracolumbar kyphosis correction (68%), and intramedullary tumors (68%), access to IOM was limited to 57% for economic reasons. Of interest, in 64% of cases, where IOM was available and significant change occurred, the actual operative procedures were significantly altered.
Conclusion: Despite the fact that 68% of spine surgeons believe IOM to be indispensable for complex spine surgery, cost remains the main barrier to its use/availability in Latin America.
Keywords: Evoked potentials, Intraoperative neurophysiological monitoring, Latin America, Spine surgery, Spine
INTRODUCTION
Intraoperative multimodal neurophysiological monitoring (IOM) helps to prevent new neurological deterioration in real time, particularly during high complex spine surgeries.[
This study evaluated the current frequency of use/availability of IOM for spine surgeons operating in Latin America.
MATERIALS AND METHODS
Study design
This cross-sectional study was performed using an IOM survey. The survey was sent to spine surgeons who were members of AO Spine Latin America (AOSLA).
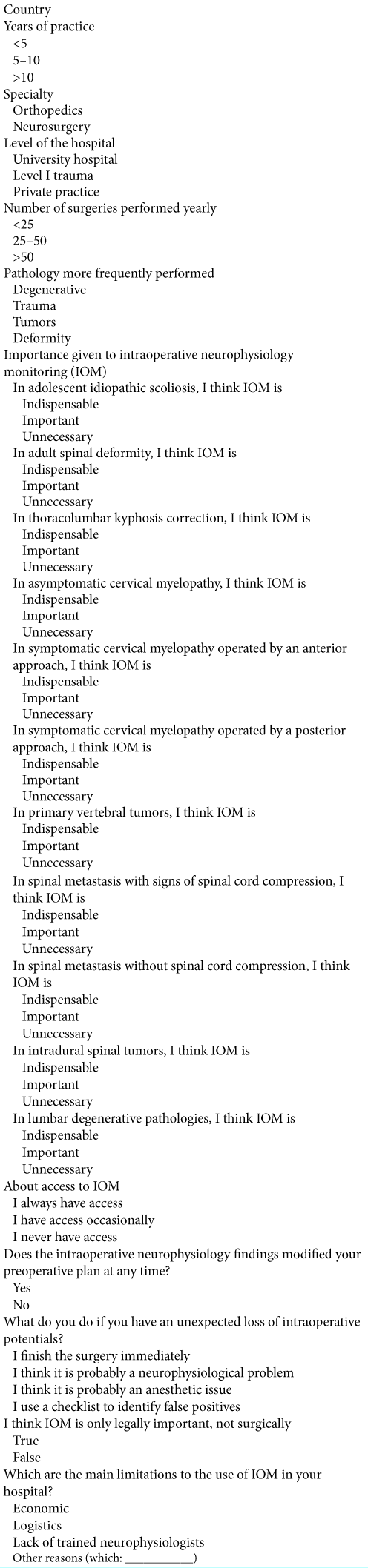
Intraoperative monitoring questionnaire
AO Spine has more than 1400 members and more than 9000 associated members in Latin America with clinical and research interest in spine care. Questionnaires were mailed to assess surgeon characteristics and opinions regarding the usage and barriers to IOM in spine operations. Variables analyzed included nationality, age, specialty, years of experience, level of complexity of the hospitals, number of surgeries per year, type of pathology, and level of importance given by the surgeon to IOM. General questions evaluated regarding IOM accessibility encompassed; barriers to usage, attitudes after IOM changes, and the legal value [
Statistical analysis
Surgeons’ opinions were compared by country, years of experience, and specialty. Comparisons were performed using the Fisher’s exact test. Post hoc comparisons were adjusted using the Bonferroni procedure. Data were processed and analyzed using SPSS version 22.0 (IBM, Armonk, New York, USA).
RESULTS
Surgeon characteristics
The questionnaire was answered by 200 members of AOSLA; they were from different countries, and the number of participants in each country, along with their specialties and years of experience, was assessed [
Barriers for IOM usage
The most common limitations to access/use of IOM were economic reasons (57%) followed by availability (20%) and finally lack of trained neurophysiologists (16%).
More surgeons considered IOM to be essential for adolescent scoliosis surgery, thoracolumbar kyphosis correction, and removal of intramedullary tumors [
Notably, 64% of surgical plans were altered intraoperatively due to significant IOM changes. About 89% used a checklist in case of loss of IOM; 5% finished the procedure, 4% thought that it was a neurophysiological problem, and 1% attributed it to anesthetic issues. The vast majority of the surgeons answered that IOM was of real clinical importance during surgeries (92%) and not just used to address legal issues.
DISCUSSION
IOM has been widely used as an important adjunct in spine surgery. In a large, nationally representative dataset,[
Use of IOM during spine surgery in different countries
Different countries found varying rates for using/advocating IOM for spine surgery.
A Germany-Austria-Switzerland study involved 575 centers with 63.8% response rate (e.g., mostly spine centers). IOM was more heavily used by neurosurgery versus orthopedics.[
IOM in cervical pathology
Motor-evoked potentials can be especially useful in anterior cervical spine surgery where motor tracts are particularly at risk. In the USA, from 2007 to 2014, 15,395 patients underwent an ACDF in the treatment of spondylotic myelopathy/radiculopathy, a patient group considered low risk compared with patients with fractures, tumors, or deformities. However, the overall incidence of neurological injuries after ACDF surgery was 0.27%. IOM was used in 2627 patients (17.1%), and there was a significant decrease in the use of ACDF from 22.8% in 2007 to 4.3% use in 2014.[
Cost-benefit relation
A point of permanent debate is the cost-benefit relation of IOM.[
In government hospitals and university hospitals, there is greater access to IOM versus private hospitals since they have trained personnel to perform IOM. Only a single case is needed with a bad neurological result to justify many IOM cases.[
CONCLUSION
It is essential to better educate Latin America spine surgeons regarding the clinical value and cost/benefit ratio of performing safer IOM monitored spine surgery.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
AOSLA for survey distribution, writing assistance, and proofreading.
References
1. Ajiboye RM, D’Oro A, Ashana AO, Buerba RA, Lord EL, Buser Z. Routine use of intraoperative neuromonitoring during ACDFs for the treatment of spondylotic myelopathy and radiculopathy is questionable: A review of 15,395 cases. Spine (Phila Pa 1976). 2017. 42: 14-9
2. Ajiboye RM, Zoller SD, Sharma A, Mosich GM, Drysch A, Li J. Intraoperative neuromonitoring for anterior cervical spine surgery: What is the evidence?. Spine (Phila Pa 1976). 2017. 42: 385-93
3. Avila EK, Elder JB, Singh P, Chen X, Bilsky MH. Intraoperative neurophysiologic monitoring and neurologic outcomes in patients with epidural spine tumors. Clin Neurol Neurosurg. 2013. 115: 2147-52
4. George J, Das S, Egger AC, Chambers RC, Kuivila TE, Goodwin RC. Influence of intraoperative neuromonitoring on the outcomes of surgeries for pediatric scoliosis in the United States. Spine Deform. 2019. 7: 27-32
5. Ghadirpour R, Nasi D, Iaccarino C, Giraldi D, Sabadini R, Motti L. Intraoperative neurophysiological monitoring for intradural extramedullary tumors: Why not?. Clin Neurol Neurosurg. 2015. 130: 140-9
6. Korn A, Halevi D, Lidar Z, Biron T, Ekstein P, Constantini S. Intraoperative neurophysiological monitoring during resection of intradural extramedullary spinal cord tumors: Experience with 100 cases. Acta Neurochir (Wien). 2015. 157: 819-30
7. Kumar N, Vijayaraghavan G, Ravikumar N, Ding Y, Yin ML, Patel RS. Intraoperative neuromonitoring (IONM): Is there a role in metastatic spine tumor surgery?. Spine (Phila Pa 1976). 2019. 44: E219-24
8. Laratta JL, Shillingford JN, Ha A, Lombardi JM, Reddy HP, Saifi C. Utilization of intraoperative neuromonitoring throughout the United States over a recent decade: An analysis of the nationwide inpatient sample. J Spine Surg. 2018. 4: 211-9
9. Netto MB, Neto MI, Ferreira RJ, Zuiani GR, Cavali PT, Veiga IG. The reality of using intraoperative neurophysiologic monitoring among Brazilian spine surgeons. Coluna Columna. 2012. 11: 310-4
10. Ney JP, van der Goes DN, Nuwer MR. Does intraoperative neurophysiologic monitoring matter in noncomplex spine surgeries?. Neurology. 2015. 85: 2151-8
11. Ney JP, van der Goes DN, Watanabe JH. Cost-benefit analysis: Intraoperative neurophysiological monitoring in spinal surgeries. J Clin Neurophysiol. 2013. 30: 280-6
12. Nixon AT, Smith ZA, Lawton CD, Wong AP, Dahdaleh NS, Koht A. Bilateral neurological deficits following unilateral minimally invasive TLIF: A review of four patients. Surg Neurol Int. 2014. 5: S317-24
13. Nuwer MR, Dawson EG, Carlson LG, Kanim LE, Sherman JE. Somatosensory evoked potential spinal cord monitoring reduces neurologic deficits after scoliosis surgery: Results of a large multicenter survey. Electroencephalogr Clin Neurophysiol. 1995. 96: 6-11
14. Peeling L, Hentschel S, Fox R, Hall H, Fourney DR. Intraoperative spinal cord and nerve root monitoring: A survey of Canadian spine surgeons. Can J Surg. 2010. 53: 324-8
15. Sala F, Dvorak J, Faccioli F. Cost effectiveness of multimodal intraoperative monitoring during spine surgery. Eur Spine J. 2007. 16: S229-31
16. Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F. Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: A historical control study. Neurosurgery. 2006. 58: 1129-43
17. Siller S, Raith C, Zausinger S, Tonn JC, Szelenyi A. Indication and technical implementation of the intraoperative neurophysiological monitoring during spine surgeries-a transnational survey in the German-speaking countries. Acta Neurochir (Wien). 2019. 161: 1865-75
18. Sutter M, Deletis V, Dvorak J, Eggspuehler A, Grob D, Macdonald D. Current opinions and recommendations on multimodal intraoperative monitoring during spine surgeries. Eur Spine J. 2007. 16: S232-7
19. Tamkus A, Rice KS, Kim HL. Intraoperative neuromonitoring alarms: Relationship of the surgeon’s decision to intervene (or not) and clinical outcomes in a subset of spinal surgical patients with a new postoperative neurological deficit. Neurodiagn J. 2017. 57: 276-87