- Department of Neurobiology and Anatomy, Clinical Neurosciences Center, Salt Lake City, Utah, USA
- Department of Neurosurgery, Clinical Neurosciences Center, Salt Lake City, Utah, USA
- Department of Radiology, University of Utah, Salt Lake City, Utah, USA
Correspondence Address:
John D. Rolston
Department of Neurosurgery, Clinical Neurosciences Center, Salt Lake City, Utah, USA
DOI:10.4103/sni.sni_210_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Stephanie V. Avila, Brooke Van Noy, Michael Karsy, Matthew Alexander, John D. Rolston. Bilateral blunt cerebrovascular injury resulting in direct carotid-cavernous fistulae: A case report and review of the literature. 19-Nov-2018;9:229
How to cite this URL: Stephanie V. Avila, Brooke Van Noy, Michael Karsy, Matthew Alexander, John D. Rolston. Bilateral blunt cerebrovascular injury resulting in direct carotid-cavernous fistulae: A case report and review of the literature. 19-Nov-2018;9:229. Available from: http://surgicalneurologyint.com/surgicalint-articles/9072/
Abstract
Background:Bilateral blunt cerebrovascular injury (BCVI) has been documented in 32 patients in the English-language literature and bilateral carotid-cavernous fistulae (CCFs) have been reported in only 1 patient. Here, we present a case of severe, unexpected bilateral BCVI with bilateral direct CCF and review the literature of BCVI, particularly cases of bilateral injury.
Case Description:A 65-year-old woman with episodic bradycardia presented after a motor vehicle accident. On arrival, she had a Glasgow Coma Scale of 3T and progressive dilation of her right pupil. Computed tomography imaging showed a 1.8-cm right epidural hematoma (EDH) with 6 mm of right-to-left shift. No acute skull-base fracture or injury in the area of the carotid canal was noted. The patient was treated with 3% hypertonic saline and mannitol before being taken to the operating room for emergent decompression of the hematoma. Although the patient initially presented with an EDH, significant intraoperative hemorrhage was identified during surgical evacuation and later confirmed as bilateral direct CCFs during angiographic evaluation. Because of the patient's devastating injuries, life-extending measures were not continued and the patient died.
Conclusions:A review of the literature indicates that bilateral CCFs are rare, having been reported only once previously. As this case demonstrates, CCFs may occur in high-energy injuries and should be considered even if the patient does not meet traditional screening criteria.
Keywords: Blunt cerebrovascular injury, carotid-cavernous fistula, dissection
INTRODUCTION
Blunt cerebrovascular injury (BCVI) is a potentially morbid result of traumatic brain injury that can result in dissection of blood vessels.[
The use of computerized tomography angiography has enabled rapid evaluation of patients with BCVI; however, a high index of clinical suspicion is required because BCVI and CCF can be missed. For instance, the antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS) trial, which evaluated BCVI treatment modalities, demonstrated difficulty in diagnosing BCVI in up to 20% of cases.[
We present a case of severe, unexpected bilateral BCVI with bilateral direct CCF and provide a review of the literature describing the diagnosis, management, and outcomes of bilateral BCVI.
CLINICAL PRESENTATION
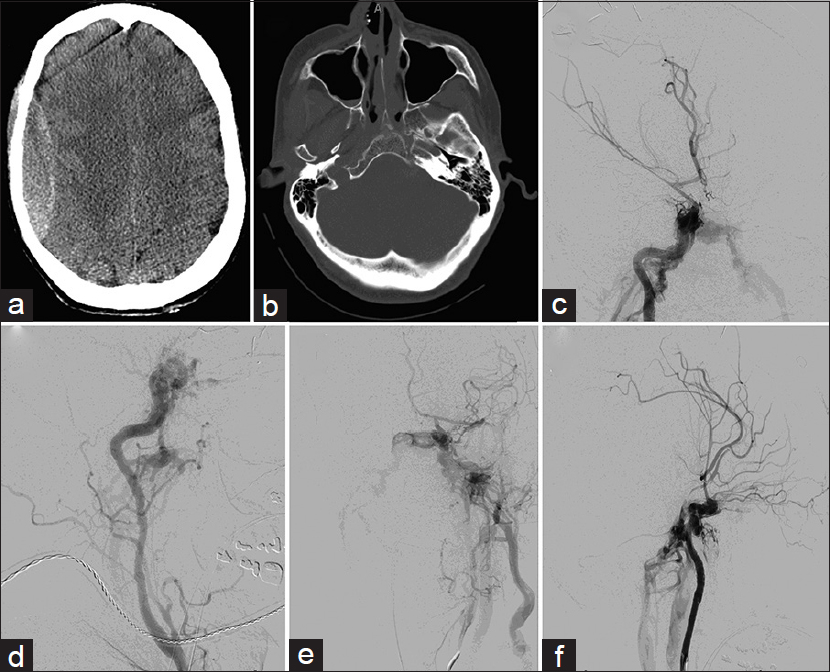
A 65-year-old woman with unknown past medical history presented after a motor vehicle rollover in which she was restrained with a seatbelt. The patient was intubated at the scene, stabilized at an outside hospital, and transferred to our hospital. She exhibited episodic bradycardia en route but retained reactive pupils. On arrival, the patient's Glasgow Coma Scale (GCS) score was 3T with progressive dilation of her right pupil. Computed tomography (CT) imaging showed a 1.8-cm right epidural hematoma (EDH) with 6-mm right-to-left shift but no acute skull-base fracture or injury in the area of the carotid canal [Figure
Figure 1
Bilateral blunt cerebrovascular injury (BCVI) with associated high-flow caroticocavernous fistulas (CCFs) is shown. (a) Non-contrast axial CT demonstrates a 1.8-cm right EDH with 6 mm of right-to-left shift. (b) Axial bone window CT shows no acute skull-base fracture or injury in the area of the carotid canal. (c) Townes and (d) lateral digital subtraction angiographic (DSA) images during right internal carotid artery (ICA) injection undertaken after the patient continued to have uncontrolled bleeding intraoperatively show a direct CCF with drainage through the bilateral inferior petrosal sinuses. Flow through the anterior cerebral (ACA) and middle cerebral (MCA) arteries was significantly slow, with displacement of the MCA branches due to mass effect. (e) Townes and (f) lateral DSA images of a left ICA injection show a direct CCF with outflow through the inferior petrosal sinuses, as well as egress through the left external jugular system. Flow through the ACA and MCA was diminished
We completed evacuation of the EDH without difficulty; however, significant unexpected bleeding was uncovered from the skull-base and carotid-cavernous triangle. There was worsening bleeding from deep within the Sylvian fissure, prompting us to open the dura to achieve additional decompression. Extradural coagulation of the middle meningeal artery and ipsilateral neck pressure reduced the bleeding, but incompletely. We packed the wound and proceeded for emergent angiography to identify the source of bleeding.
Digital subtraction angiography (DSA) showed a large dissecting pseudoaneurysm of the cavernous segment of the right internal carotid artery (ICA), with arteriovenous shunting into the cavernous sinus consistent with a direct CCF. Outflow was noted through the bilateral inferior petrosal sinuses with no visualized cortical venous reflux [Figure
DISCUSSION
CT, magnetic resonance angiography, or DSA can be used to screen for BCVI.[
The Canadian Stroke Best Practice Recommendations for the Secondary Prevention of Stroke[
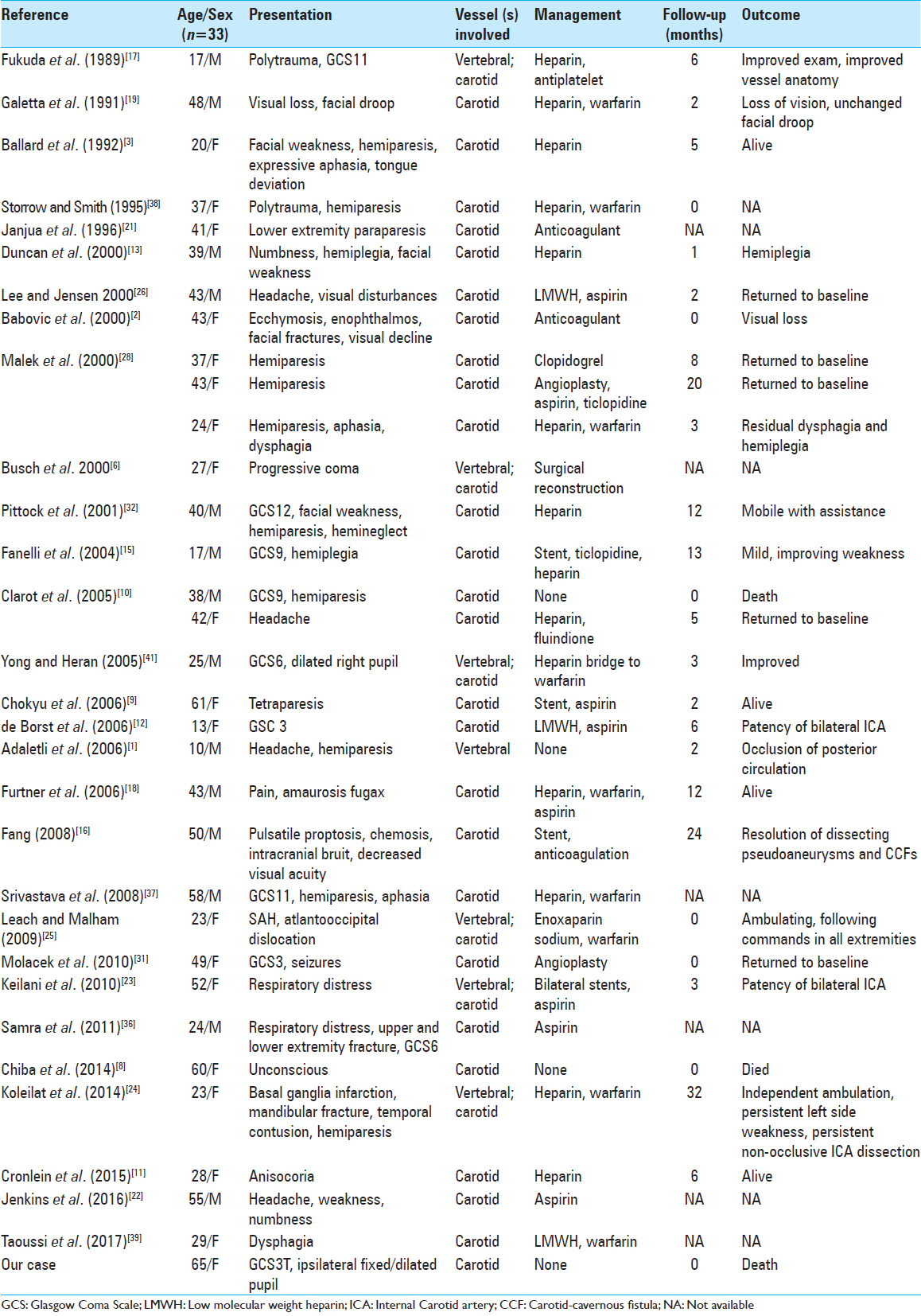
We identified 29 studies with 32 patients who had bilateral BCVI [
Bilateral CCFs are rare, with only 1 prior case reported after traumatic ICA dissection. Fang[
CONCLUSION
Bilateral CCFs due to trauma are exceedingly rare, having been reported only once previously. Although the injury was fatal in our case, we believe that continued improvements in the diagnosis and treatment of BCVI, as well as awareness that CCFs may occur in high-energy injuries and should be considered even if the patient does not meet traditional screening criteria, will improve future outcomes in cases of bilateral CCF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adaletli I, Sirikci A, Ulus S, Yilmaz MH, Kervancioglu S, Kurugoglu S. Traumatic bilateral vertebral artery dissection at the dural entry point site in a 10-year-old boy. Pediatr Surg Int. 2006. 22: 468-70
2. Babovic S, Zietlow SP, Garrity JA, Kasperbauer JL, Bower TC, Bite U. Traumatic carotid artery dissection causing blindness. Mayo Clin Proc. 2000. 75: 296-8
3. Ballard JL, Bunt TJ, Fitzpatrick B, Malone JM. Bilateral traumatic internal carotid artery dissections: case report. J Vasc Surg. 1992. 15: 431-5
4. Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: Implications of a new grading scale. J Trauma. 1999. 47: 845-853
5. Burlew CC, Biffl WL, Moore EE, Barnett CC, Johnson JL, Bensard DD. Blunt cerebrovascular injuries: Redefining screening criteria in the era of noninvasive diagnosis. J Trauma Acute Care Surg. 2012. 72: 330-5
6. Busch T, Aleksic I, Sirbu H, Kersten J, Dalichau H. Complex traumatic dissection of right vertebral and bilateral carotid arteries: a case report and literature review. Cardiovasc Surg. 2000. 8: 72-4
7. Markus HS, Hayter E, Levi C, Feldman A, Venables G. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): A randomised trial. Lancet Neurol. 2015. 14: 361-7
8. Chiba F, Makino Y, Motomura A, Inokuchi G, Ishii N, Torimitsu S. Bilateral middle cerebral artery infarction associated with traumatic common carotid artery dissection: A case report and review of literature. Forensic Sci Int. 2014. 236: e1-4
9. Chokyu I, Tsumoto T, Miyamoto T, Yamaga H, Terada T, Itakura T. Traumatic bilateral common carotid artery dissection due to strangulation. A case report. Interv Neuroradiol. 2006. 12: 149-54
10. Clarot F, Vaz E, Papin F, Proust B. Fatal and non-fatal bilateral delayed carotid artery dissection after manual strangulation. Forensic Sci Int. 2005. 149: 143-150
11. Cronlein M, Sandmann GH, Beirer M, Wunderlich S, Biberthaler P, Huber-Wagner S. Traumatic bilateral carotid artery dissection following severe blunt trauma: A case report on the difficulties in diagnosis and therapy of an often overlooked life-threatening injury. Eur J Med Res. 2015. 20: 62-
12. de Borst GJ, Slieker MG, Monteiro LM, Moll FL, Braun KP. Bilateral traumatic carotid artery dissection in a child. Pediatr Neurol. 2006. 34: 408-411
13. Duncan MA, Dowd N, Rawluk D, Cunningham AJ. Traumatic bilateral internal carotid artery dissection following airbag deployment in a patient with fibromuscular dysplasia. Br J Anaesth. 2000. 85: 476-8
14. Ellis JA, Goldstein H, Connolly ES, Meyers PM. Carotid-cavernous fistulas. Neurosurg Focus. 2012. 32: E9-
15. Fanelli F, Salvatori FM, Ferrari R, Pacella S, Rossi P, Passariello R. Stent repair of bilateral post-traumatic dissections of the internal carotid artery. J Endovasc Ther. 2004. 11: 517-21
16. Fang C. Endovascular treatment of a high-flow direct traumatic carotid cavernous fistula with a two year follow-up. Interv Neuroradiol. 2008. 14: 297-301
17. Fukuda I, Meguro K, Matsusita S, Shigeta O, Oohashi N, Nakata Y. Traumatic disruption of bilateral vertebral arteries and internal carotid arteries: case report. J Trauma. 1989. 29: 263-6
18. Furtner M, Werner P, Felber S, Schmidauer C. Bilateral carotid artery dissection caused by springboard diving. Clin J Sport Med. 2006. 16: 76-8
19. Galetta SL, Leahey A, Nichols CW, Raps EC. Orbital ischemia, ophthalmoparesis, and carotid dissection. J Clin Neuroophthalmol. 1991. 11: 284-7
20. Herbert JP, Venkataraman SS, Turkmani AH, Zhu L, Kerr ML, Patel RP. Pediatric blunt cerebrovascular injury: The McGovern screening score. J Neurosurg Pediatr. 2018. 21: 639-49
21. Janjua KJ, Goswami V, Sagar G. Whiplash injury associated with acute bilateral internal carotid arterial dissection. J Trauma. 1996. 40: 456-8
22. Jenkins JM, Norton J, Hampton T, Weeks R. Rare case of bilateral traumatic internal carotid artery dissection. BMJ Case Rep. 2016. 2016: bcr2016217262-
23. Keilani ZM, Berne JD, Agko M. Bilateral internal carotid and vertebral artery dissection after a horse-riding injury. J Vasc Surg. 2010. 52: 1052-7
24. Koleilat I, Gandhi R, Boulos A, Bonville D. Traumatic bilateral carotid and vertebral artery dissection. J Emerg Trauma Shock. 2014. 7: 47-8
25. Leach JC, Malham GM. Complete recovery following atlantoaxial fracture-dislocation with bilateral carotid and vertebral artery injury. Br J Neurosurg. 2009. 23: 92-4
26. Lee WW, Jensen ER. Bilateral internal carotid artery dissection due to trivial trauma. J Emerg Med. 2000. 19: 35-41
27. Lin TC, Mao SH, Chen CH, Chen YL, Wong HF, Chang CJ. Systematic analysis of the risk factors affecting the recurrence of traumatic carotid-cavernous sinus fistula. World Neurosurg. 2016. 90: 539-45 e531
28. Malek AM, Higashida RT, Halbach VV, Dowd CF, Phatouros CC, Lempert TE. Patient presentation, angiographic features, and treatment of strangulation-induced bilateral dissection of the cervical internal carotid artery. Report of three cases. J Neurosurg. 2000. 92: 481-7
29. Menon R, Kerry S, Norris JW, Markus HS. Treatment of cervical artery dissection: A systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2008. 79: 1122-7
30. Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M. Prospective screening for blunt cerebrovascular injuries: Analysis of diagnostic modalities and outcomes. Ann Surg. 2002. 236: 386-
31. Molacek J, Baxa J, Houdek K, Ferda J, Treska V. Bilateral post-traumatic carotid dissection as a result of a strangulation injury. Ann Vasc Surg. 2010. 24: 1133.e9-11
32. Pittock SJ, Moroney JT, Alexander M, Brennan P, Moorhouse D. Traumatic bilateral carotid dissection with concomitant cerebral infarction. J Emerg Med. 2001. 20: 33-8
33. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018. 49: e46-e110
34. Ravindra VM, Riva-Cambrin J, Sivakumar W, Metzger RR, Bollo RJ. Risk factors for traumatic blunt cerebrovascular injury diagnosed by computed tomography angiography in the pediatric population: A retrospective cohort study. J Neurosurg Pediatr. 2015. 15: 599-606
35. Redekop GJ. Extracranial carotid and vertebral artery dissection: A review. Can J Neurol Sci. 2008. 35: 146-52
36. Samra NS, Ravi AK, Johnson LW, Williams M. Traumatic bilateral carotid artery dissection. J La State Med Soc. 2011. 163: 26-8
37. Srivastava A, Bradley M, Kelly M. Bilateral carotid artery dissection after high impact road traffic accident. J Radiol Case Rep. 2008. 2: 23-8
38. Storrow AB, Smith BA. Traumatic bilateral carotid dissection. J Emerg Med. 1995. 13: 169-74
39. Taoussi N, Alghamdi AJ, Bielewicz J, Luchowski P, Rejdak K. Traumatic bilateral dissection of cervical internal carotid artery in the wake of a car accident: A case report. Neurol Neurochir Pol. 2017. 51: 432-8
40. Wein T, Lindsay MP, Cote R, Foley N, Berlingieri J, Bhogal S. Canadian stroke best practice recommendations: Secondary prevention of stroke, sixth edition practice guidelines, update 2017. Int J Stroke. 2018. 3: 420-43
41. Yong RL, Heran NS. Traumatic carotid cavernous fistula with bilateral carotid artery and vertebral artery dissections. Acta Neurochir (Wien). 2005. 147: 1109-13