- Department of Medicine, State University of Para,
- Department of Neurosurgery, Ophir Loyola Hospital,
- Federal University of Para, Belem, Para, Brazil.
Correspondence Address:
Camila Furtado Leao
Department of Neurosurgery, Ophir Loyola Hospital,
DOI:10.25259/SNI_569_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Camila Furtado Leao, Maira Piani Couto, Jose Antonio Santos de Lima, Eric Homero Albuquerque Paschoal, Jose Reginaldo Nascimento Brito. Brainstem abscess treated conservatively. 25-Jul-2020;11:205
How to cite this URL: Camila Furtado Leao, Maira Piani Couto, Jose Antonio Santos de Lima, Eric Homero Albuquerque Paschoal, Jose Reginaldo Nascimento Brito. Brainstem abscess treated conservatively. 25-Jul-2020;11:205. Available from: https://surgicalneurologyint.com/surgicalint-articles/10159/
Abstract
Background: Brainstem abscess is a rare condition with a variety of treatment approaches. In this paper, we report an unusual case of a brainstem abscess with a positive outcome in an immunocompetent patient who was treated with antibiotic therapy.
Case Description: A 22-year-old female presented with bilateral tetraparesis that was worse on the left hemibody, appendicular tremor, and left upper eyelid ptosis. Brain magnetic resonance imaging showed an abscess in the pons and midbrain due to possible nocardiosis. She was treated with dexamethasone, phenytoin, vancomycin, and meropenem for 8 weeks and trimethoprim-sulfamethoxazole for 6 weeks. The brain injury decreased, and the patient’s neurological status significantly improved.
Conclusion: Brainstem abscess may be treated conservatively, leading to improvement of the clinical condition and decreased lesion size on imaging.
Keywords: Antibiotic therapy, Brain abscess, Brainstem, Nocardia infections
INTRODUCTION
Brainstem abscess is an uncommon and severe condition.[
The clinical manifestations depend on the size and stage of the infection. Symptoms include fever, headache, vomiting (due to an increase in intracranial pressure), tetraparesis, and diplopia, with or without sepsis.[
CASE REPORT
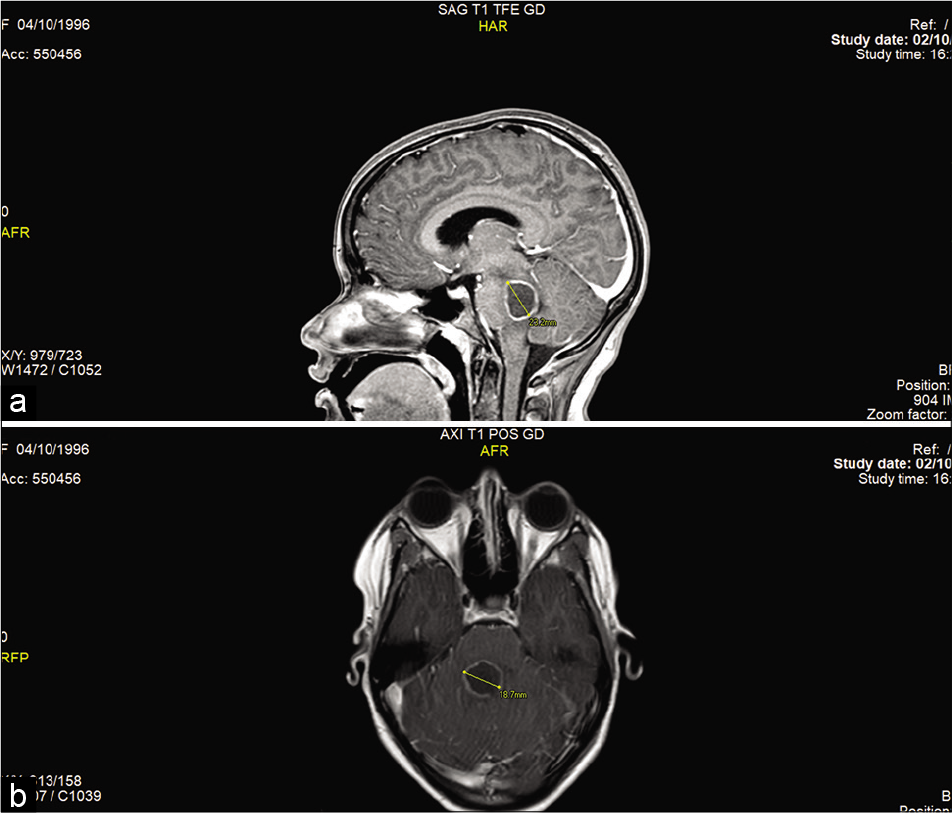
A 22-year-old immunocompetent female was referred to Ophir Loyola Hospital presenting a 6-day history of tetraparesis, which was worst in the left hemibody, appendicular tremor, and left upper eyelid ptosis. On admission, the Glasgow coma scale (GCS) was 13, and she presented tetraparesis, which was worst in left hemibody, ataxia, hypoesthesia of the left side of the face and the left hemibody, left upper eyelid ptosis, right 6th cranial nerve paresis, right peripheral facial paralysis, vertigo, and nausea. She could not walk and was using a nasogastric tube. No other alterations were observed. Magnetic resonance imaging (MRI) of the brain showed an encapsulated lesion with peripheral contrast in the brainstem (pons and midbrain), suggestive of abscess; after spectrometric study, the lesion measured 18.7 mm axially and 23.2 mm sagittally [
Figure 1:
(a) Magnetic resonance imaging showing contrast (gadolinium) lesions in the pons and midbrain in the sagittal orientation before antibiotic treatment. (b) Magnetic resonance imaging showing contrast (gadolinium) lesions in the pons and midbrain in the axial orientations before antibiotic treatment.
On the 42nd day of hospitalization, the patient underwent a new chest CT that showed improvement in lung injury, and a presumptive diagnosis of nocardiosis was established by a pneumologist. Thus, trimethoprim-sulfamethoxazole (160 mg + 800 mg) was added to the antibiotic regimen.
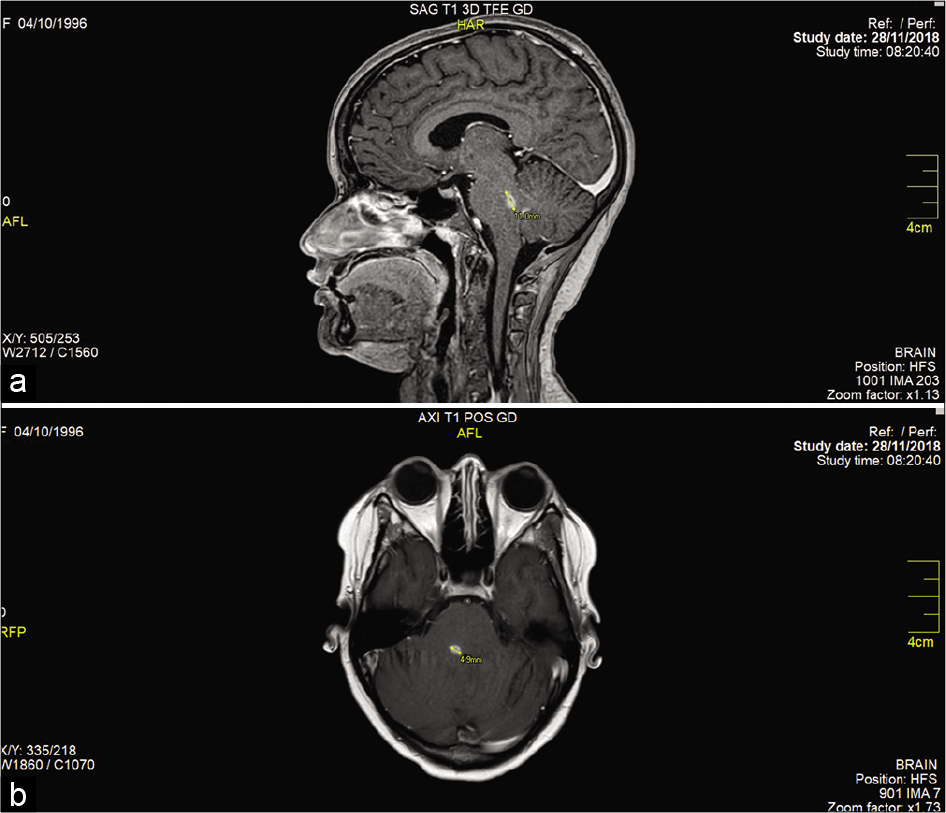
On the 49th day of hospitalization, after 8 weeks of vancomycin and meropenem and 2 weeks of trimethoprim- sulfamethoxazole, the patient was discharged. On physical examination, she was conscious and oriented, with GCS 15 and normal reflexes, presenting retardation of movement of the arm, strength graduated on 4/5 of the left arm, and hypoesthesia of the left hemibody. In addition, the patient presented with right 6th cranial nerve paresis and right peripheral facial paralysis and did not walk. The image examination showed a lesion measuring 4.9 mm (axially) × 11 mm (sagittally) [
Figure 2:
(a) Magnetic resonance imaging showing contrast (gadolinium) lesions in the pons and midbrain in the sagittal orientation after antibiotic treatment. (b) Magnetic resonance imaging showing contrast (gadolinium) lesions in the pons and midbrain in the axial orientation after antibiotic treatment.
After 2 weeks, she returned to the neurosurgery ambulatory service; she was walking with support and had right 6th cranial nerve paresis, right peripheral facial paralysis, diplopia, and GCS 15.
DISCUSSION
Here, we described the evolution of a case of a female patient who was treated at the neurosurgery service of a hospital for brainstem abscess after pulmonary nocardiosis. She was treated with antibiotic therapy, which resulted in improvement of neurological condition and neuroimaging, with a decrease in lesion size of 13.8 mm axially and 12.2 mm sagittally.
Drug therapy must be considered the first choice for brainstem abscesses, principally due to the difficulty of surgical access.[
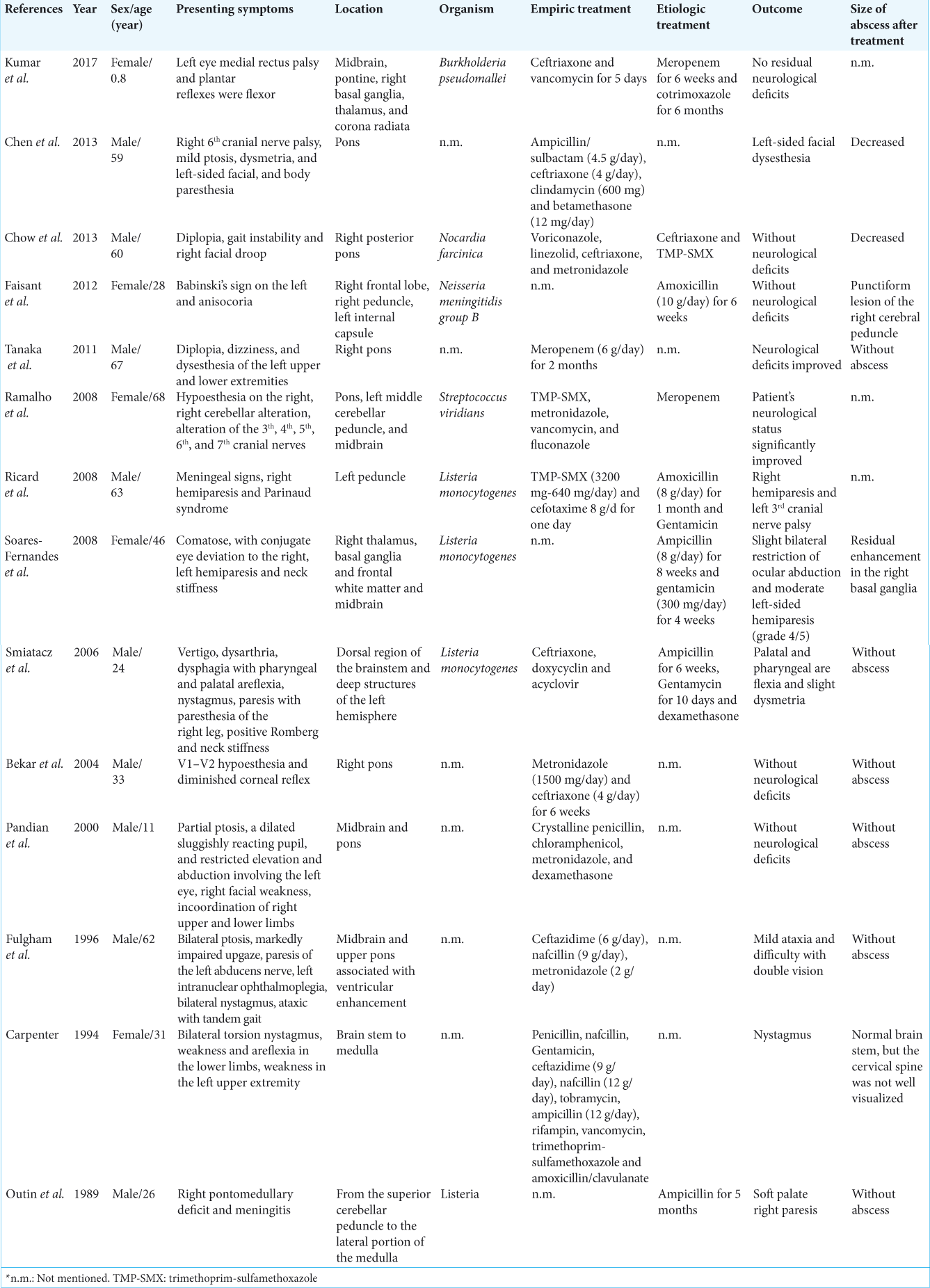
We found 14 case reports describing antibiotic therapy for the treatment of brainstem abscess.[
Empirical treatment with broad-spectrum antibiotics must be started immediately and maintained for 6 to 8 weeks or more, with sequential brain MRI to monitor the effectiveness of the treatment every 2 weeks.[
Infections caused by nocardia may affect the skin, lung, and lymph nodes and may disseminate to the central nervous system (CNS).[
In this case report and literature review, we showed that conservative treatment of brainstem abscess may lead to a positive outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aliaga L, Fatoul G, Guirao E, Peña A, Rodríguez-Granger J, Cobo F. Nocardia paucivorans brain abscess. Clinical and microbiological characteristics. IDCases. 2018. 13: e00422-
2. Arias M, Dapena D, Arias-Rivas S, Vázquez F. Widespread brainstem abscess resolved with medical therapy. Neurologia. 2007. 22: 118-21
3. Arrache D, Zait H, Rodriguez-Nava V, Bergeron E, Durand T, Yahiaoui M. Cerebral and pulmonary nocardiosis to Nocardia abscessus in an immunocompetent Algerian patient. J Mycol Med. 2018. 28: 531-7
4. Arzoglou V, D’Angelo L, Koutzoglou M, Di Rocco C. Abscess of the medulla oblongata in a toddler: Case report and technical considerations based on magnetic resonance imaging tractography. Neurosurgery. 2011. 69: E483-7
5. Baburao A, Prasad S, Prakash S, Narayanswamy H. Pulmonary nocardiosis: Report of two cases from a tertiary care hospital. Indian J Pathol Microbiol. 2019. 62: 153-5
6. Bekar A, Kocaeli H, Yilmaz E, Doğan S. Trigeminal neuralgia caused by a pontine abscess: Case report. Neurosurgery. 2004. 55: E1450-2
7. Bulthuis VJ, Gubler FS, Teernstra OP, Temel Y. A case of a brain stem abscess with a favorable outcome. Surg Neurol Int. 2015. 6: 161-
8. Carpenter JL. Brain stem abscesses: Cure with medical therapy, case report, and review. Clin Infect Dis. 1994. 18: 219-26
9. Chen MH, Kao HW, Cheng CA. Complete resolution of a solitary pontine abscess in a patient with dental caries. Am J Emerg Med. 2013. 31: 892.e3-4
10. Chow FC, Marson A, Liu C. Successful medical management of a Nocardia farcinica multiloculated pontine abscess. BMJ Case Rep. 2013. 2013: bcr2013201308-
11. Faisant C, Cochin JP, Rapoport N, Evreux F, Vaschalde Y. Cerebral trunk abscess due to Neisseria meningitidis in a 28-year-old immunocompetent patient. Rev Neurol (Paris). 2012. 168: 287-90
12. Filho PT, Zanini MA. Brainstem abscess of undetermined origin: Microsurgical drainage and brief antibiotic therapy. Sao Paulo Med J. 2014. 132: 121-4
13. Fuentes S, Bouillot P, Regis J, Lena G, Choux M. Management of brain stem abscess. Br J Neurosurg. 2001. 15: 57-62
14. Fulgham JR, Wijdicks EF, Wright AJ. Cure of a solitary abscess with antibiotic therapy: Case report. Neurology. 1996. 46: 1451-4
15. Ghannane H, Laghmari M, Aniba K, Lmejjati M, Benali SA. Diagnostic and management of pediatric brain stem abscess, a case-based update. Childs Nerv Syst. 2011. 27: 1053-62
16. Kirchhoff DC, Kirchhoff DF, Muoio V. Abscessos do tronco cerebral: Apresentação de seis casos. Arq Bras Neurocir. 2008. 27: 30-4
17. Kumar MP, Krishnamurthy S, Venkateswaran VS, Mahadevan S, Lalitha M, Sistla S. Brainstem micro-abscesses caused by Burkholderia pseudomallei in a 10-month-old infant: A case report. Paediatr Int Child Health. 2017. 37: 230-2
18. Outin HD, Merrer J, Molho H, Rabault N, Simon N, Nouailhat F. Solitary listerial abscess of the brain stem. Cure with antibiotic treatment. Rev Neurol (Paris). 1989. 145: 153-6
19. Pandian JD, Moosa NV, Cherian PJ, Radhakrishnan K. Brainstem abscess complicating tetralogy of fallot successfully treated with antibiotics alone. Neurol India. 2000. 48: 272-5
20. Ramalho J, Castillo M. Case of the season: Brainstem abscess. Semin Roentgenol. 2008. 43: 168-70
21. Rawat D, Rajasurya V, Chakraborty RK, Sharma S.editors. Nocardiosis. Treasure Island (FL): Stat Pearls; 2020. p.
22. Ricard D, Sallansonnet-Froment M, Defuentes G, de Greslan T, Bounolleau P, Taillia H. Listeria monocytogenes abscess of the brain. Rev Neurol (Paris). 2008. 164: 388-93
23. Smiatacz T, Kowalik MM, Hlebowicz M. Prolonged dysphagia due to Listeriarhombencephalitis with brainstem abscess and acute polyradiculoneuritis. J Infect. 2006. 52: e165-7
24. Soares-Fernandes JP, Beleza P, Cerqueira JJ, Ribeiro M, Maré R, Lourenço E. Simultaneous supratentorial and brainstem abscesses due to Listeria monocytogenes. J Neuroradiol. 2008. 35: 173-6
25. Stein M, Schirotzek I, Preuss M, Scharbrodt W, Oertel M. Brainstem abscess caused by Haemophilus influenza and Peptostreptococcus species. J Clin Neurosci. 2011. 18: 425-8
26. Tanaka T, Sakamoto H, Kato N, Arai T, Hasegawa Y. Successful treatment of brain stem and thalamic abscesses with high-dose meropenem. Brain Nerve. 2011. 63: 891-6