- Department of Neurosurgery, Tsukuba Medical Center Hospital,
- Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan.
Correspondence Address:
Eiichi Ishikawa, Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan.
DOI:10.25259/SNI_1196_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Satoshi Miyamoto1, Go Ikeda1, Ken Akimoto1, Ryota Mashiko1, Kazuya Uemura1, Eiichi Ishikawa2. Brainstem anesthesia during removal operation of ventriculoperitoneal shunt – A case report. 31-Mar-2022;13:122
How to cite this URL: Satoshi Miyamoto1, Go Ikeda1, Ken Akimoto1, Ryota Mashiko1, Kazuya Uemura1, Eiichi Ishikawa2. Brainstem anesthesia during removal operation of ventriculoperitoneal shunt – A case report. 31-Mar-2022;13:122. Available from: https://surgicalneurologyint.com/surgicalint-articles/11497/
Abstract
Background: Brainstem anesthesia is a transient loss of brainstem function usually associated with retrobulbar block and rarely seen by neurosurgeons.
Case Description: Here, we report a case of brainstem anesthesia during shunt revision operation in a 79-year-old woman. Local anesthesia administered at the end of surgery was thought to have infiltrated the subarachnoid space through a burr hole, causing prolonged unconsciousness and cranial nerves’ impairment. Spontaneous resolution occurred during systemic support.
Conclusion: As brainstem anesthesia may occur by leakage of local anesthetic through small burr holes, timing injections carefully can avoid this rare complication.
Keywords: Brainstem anesthesia, Burr hole surgery, Local anesthetics, Neurosurgery
INTRODUCTION
Brainstem anesthesia is a transient loss of brainstem function due to anesthetic drug infiltration,[
CASE REPORT
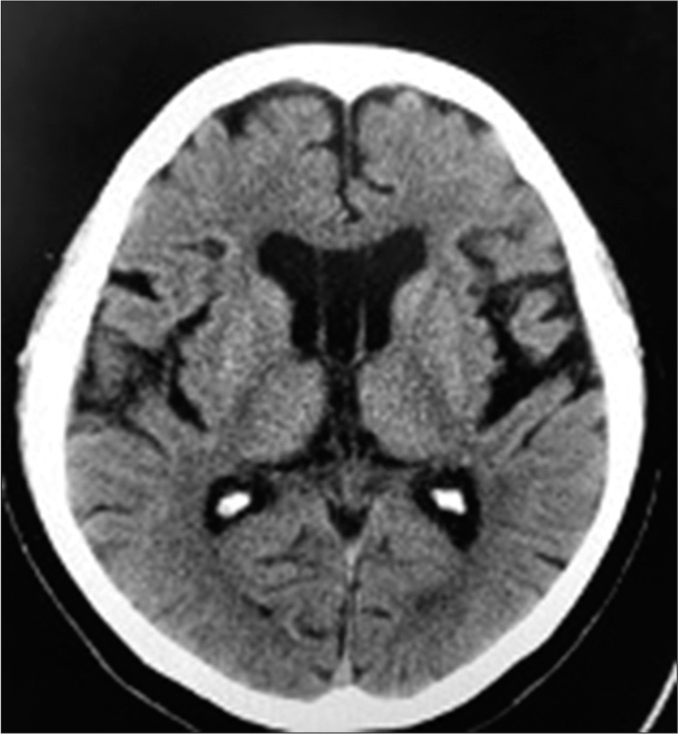
A 79-year-old female experiencing gait disturbance, cognitive impairment, and urinary incontinence for about a year presented at our hospital. CT head scanning showed enlarged ventricles (Evan’s index 0.31) and no other remarkable signs [
During the operation, propofol (60 mg), rocuronium (35 mg), and remifentanil (0.7 mg/h) were used as general anesthesia with 5% desflurane and remifentanil (0.6 mg/h) continuously infused for maintenance. We injected 10 ml of 0.5% lidocaine with epinephrine into the chest skin incision site and cut the skin to expose the shunt valve; cranial and rostral shunt tubes were removed without resistance. A clip anchor was left at the scalp so we injected 7 ml of 0.5% lidocaine with epinephrine into the previous skin incision site around the burr hole and removed it. The skin was closed after 10 ml of 0.75% bupivacaine was added into the subcutaneous layer to reduce postoperative pain. The total operation and anesthetic times were 22 and 58 min, respectively.
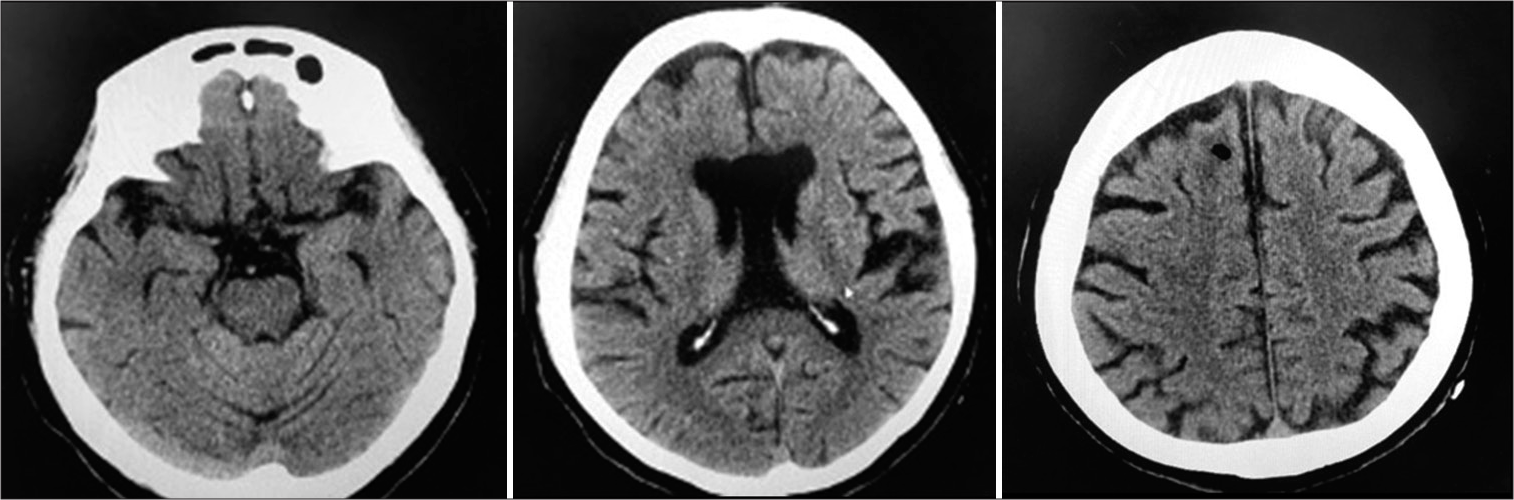
Anesthesia was reversed by Sugammadex and train of four stimulation showed diminishment of muscle relaxants, but spontaneous respiration was still not observed. At this time, vital signs were blood pressure 90/50 mmHg, pulse 80 bpm, SpO2 98%, and body temperature 35.8°C with a Japan Coma Scale score of 300 even after naloxone administration. Pupils were dilated bilaterally and light, cough, and vestibuloocular reflexes were lost. Emergent head CT showed no abnormal lesions such as hemorrhages, infarctions, or cerebral herniations [
DISCUSSION
Brainstem anesthesia
Brainstem anesthesia is a transient loss of brainstem function due to anesthetic drugs,[
Symptoms, diagnosis, and treatment
Symptoms of brainstem anesthesia are loss of consciousness, apnea, and cranial nerve paralyses, resulting in dysphagia, dysarthria, loss of pupillary light reflex, and/or dilated pupils,[
Present case
In this case, brainstem anesthesia was first noticed through prolonged unconsciousness and dilated bilateral pupils after general anesthesia. We first suspected hemorrhagic or ischemic complications but no abnormal signs were found on postoperative CT and local anesthetic intoxication was excluded because hemodynamic changes due to epinephrine were not observed. In addition, intoxication by local anesthetics often causes cardiotoxicity, such as arrhythmia,[
Comparison with the previous case
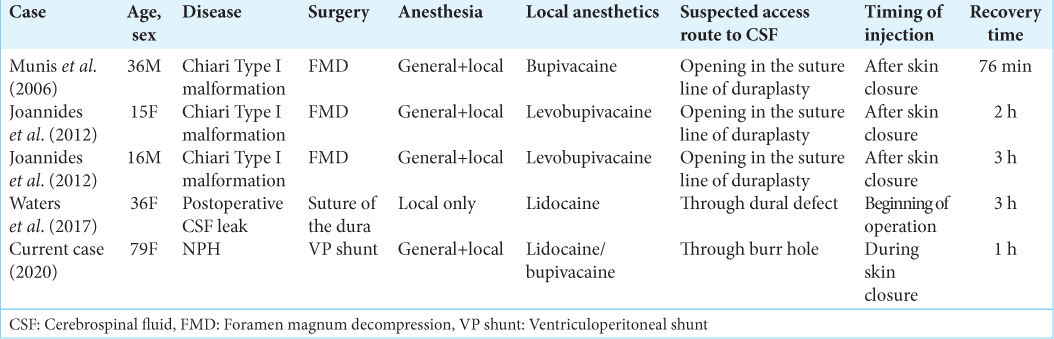
Brainstem anesthesia after neurosurgery is very rare and only four cases have been reported in PubMed (search terms: brainstem and anesthesia [
In 80% of brainstem anesthesia cases, local anesthesia was conducted at the end of the operation. Thus, the timing of injection can increase the risk of brainstem anesthesia from possible openings in the dura mater that allows infiltration of local anesthetics. As seen in our case, the cranial tube tract, leading to the subarachnoid space from the burr hole, was open for lidocaine or bupivacaine. If we had instead injected lidocaine or bupivacaine at the beginning of the surgery, we might have avoided this phenomenon since the tract would have been packed with the tube and connective tissue. As such, the timing of local anesthesia should be carefully decided to prevent risks of brainstem anesthesia.
Compared to ophthalmic surgery
Compared to retrobulbar block during ophthalmic surgery,[
Since local anesthesia during surgery is becoming more common (with multiple reports of its usefulness for postoperative pain control), especially for gastrointestinal surgery,[
CONCLUSION
We experienced a case of brainstem anesthesia through local anesthetic in a shunt tube removal operation. As brainstem anesthesia may happen even through a burr hole, neurosurgeons should be vigilant against it by considering possible pathways for local anesthetics into the subarachnoid space and carefully timing administration of local anesthetics.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowlegdements
The authors would like to thank Dr. Alexander Zaboronok of the University of Tsukuba, Faculty of Medicine, Department of Neurosurgery for professional and language revision and Dr. Bryan J. Mathis of the University of Tsukuba Hospital International Medical Center for language revision.
References
1. Ashaye AO, Ubah JN, Sotumbi PT. Respiratory arrest after retrobulbar anaesthesia. West Afr J Med. 2002. 21: 343-4
2. Chin YC, Kumar CM. Brainstem anaesthesia revisited: Mechanism, presentation and management. Trends Anaesth Crit Care. 2013. 3: 252-6
3. Joannides AJ, Santarius T, Fernandes HM, Laing RJ, Trivedi RA. Transient perioperative brainstem paralysis secondary to a local anesthetic. J Neurosurg Pediatr. 2012. 10: 60-1
4. Malet A, Faure MO, Deletage N, Pereira B, Haas J, Lambert G. The comparative cytotoxic effects of different local anesthetics on a human neuroblastoma cell line. Anesth Analg. 2015. 120: 589-96
5. Munis JR, Marcukaitis AW, Sprung J. Delayed emergence from anesthesia associated with absent brainstem reflexes following suboccipital craniotomy. Neurocrit Care. 2006. 5: 206-9
6. Nakamura R, Nameki K, Konishi J, Terakado H, Maeda T, Suzuki T. A case with loss of consciousness and respiratory arrest following retrobulbar anesthesia. J Jpn Soc Clin Anesth. 2015. 35: 430-3
7. Nicoll JM, Acharya PA, Ahlen K, Baguneid S, Edge KR. Central nervous system complications after 6000 retrobulbar blocks. Anesth Analg. 1987. 66: 1298-302
8. Quantock CL, Goswami T. Death potentially secondary to subTenon’s block. Anaesthesia. 2007. 62: 175-7
9. Roberge CW, McEwen M. The effects of local anesthetics on postoperative pain. Aorn J. 1998. 68: 1003-12
10. Tolesa K, Gebreal GW. Brainstem anesthesia after retrobulbar block: A case report and review of literature. Ethiop J Health Sci. 2016. 26: 589-94
11. Verlinde M, Hollmann MW, Stevens MF, Hermanns H, Werdehausen R, Lirk P. Local anesthetic-induced neurotoxicity. Int J Mol Sci. 2016. 17: 339
12. Waters B, Kroll RR, Muscedere J, Lomax LB, Burjorjee JE. Stepwise rostrocaudal brainstem anesthesia as a complication of local anesthesia: A case report. A A Case Rep. 2017. 9: 277-9
13. Yamashiro H. Differentiation of brain stem anesthesia from high spinal anesthesia using auditory brain stem response. Masui. 1990. 39: 1704-7