- Department of Surgery, Section of Neurosurgery, Providence Hospital and Medical Centers, Michigan State University, East Lansing, United States of America
- Department of Neurosurgery, Michigan Spine and Brain Surgeons PLLC, Providence Hospital and Medical Centers, MI 48075, United States of America
Correspondence Address:
Stephanie Reed Falatko
Department of Surgery, Section of Neurosurgery, Providence Hospital and Medical Centers, Michigan State University, East Lansing, United States of America
Department of Neurosurgery, Michigan Spine and Brain Surgeons PLLC, Providence Hospital and Medical Centers, MI 48075, United States of America
DOI:10.4103/2152-7806.161787
Copyright: © 2015 Falatko SR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Falatko SR, Kelkar P, Setty P, Tong D, Soo TM. C1–C2 cryptic cerebrospinal fluid leak directly identified by pressurized radionuclide cisternography: Case report and review of the literature. Surg Neurol Int 29-Jul-2015;6:126
How to cite this URL: Falatko SR, Kelkar P, Setty P, Tong D, Soo TM. C1–C2 cryptic cerebrospinal fluid leak directly identified by pressurized radionuclide cisternography: Case report and review of the literature. Surg Neurol Int 29-Jul-2015;6:126. Available from: http://surgicalneurologyint.com/surgicalint_articles/c1-c2-cryptic-cerebrospinal-fluid-leak-directly-identified-by-pressurized-radionuclide-cisternography-case-report-and-review-of-the-literature/
Abstract
Background:Patients with chronic postural headaches may suffer from spontaneous intracranial hypotension (SIH). Trauma, degenerative disc spurring and connective tissue disorders are documented risk factors; in most cases there is no inciting event. Despite sophisticated means of evaluating the neuraxis, many cerebrospinal fluid (CSF) leaks are radiographically occult and treatment is focused on thoracic and cervical-thoracic regions. Although lumbar epidural blood patch (EBP) is the initial treatment of choice after failed conservative management, several studies document the need for treatment aimed at the specific leak area.
Case Description:This report describes the case of a 42-year-old female with scleroderma and sudden onset postural headaches. Magnetic resonance imaging revealed diffuse pachymeningeal enhancement suggestive of intracranial hypotension. Computed tomographic myelography demonstrated a collection of fluid ventral to the cervical thecal sac; an exact location for CSF egress was not identified. Conservative measures followed by lumbar EBP failed to alleviate her symptoms. The patient underwent placement of a lumbar drain and dynamic radionuclide cisternography (RIC). Panoramic images of the spine were taken at the time of the pressurized saline injection. The CSF leak was clearly visualized at C1–2. Treatment was focused at this region using percutaneous injection of autologous blood and fibrin glue.
Conclusion:SIH is disabling if left untreated. Spinal CSF leaks are often discrete and difficult to identify using static imaging. The use of pressurized, RIC by lumbar drain injection allows for the real-time evaluation of CSF dynamics and can more precisely identify slow flow leaks often missed with static imaging.
Keywords: Epidural blood patch, percutaneous, radionuclide cisternography, spontaneous cerebrospinal fluid leak, spontaneous intracranial hypotension
INTRODUCTION
Background and importance
Spontaneous intracranial hypotension (SIH) typically results from a spontaneous cerebrospinal fluid (CSF) leak,[
Clinical presentation
Presentation and examination
This patient is a 42-year-old Caucasian female with a history of scleroderma who presented with sudden onset holocranial headache associated with nausea, vomiting, and photophobia, improving with recumbence. The onset of symptoms was unprovoked. The patient denied recent trauma, lumbar puncture or history of headaches. Physical examination revealed a nontoxic-appearing female with stable hemodynamic parameters; who was neurologically intact. The patient had no obvious physical manifestations of scleroderma, and home medications were geared toward symptom management.
Neuro-diagnostics
Noncontrast CT and CT angiography were negative for intracranial hemorrhage, mass or vascular lesion. An attempt was made by the emergency room physician to obtain a lumbar puncture. However, the procedure was aborted as CSF pressures were sub-atmospheric and a fluid sample could not be obtained. The patient was admitted for bed rest and intravenous fluid hydration with the presumptive diagnosis of SIH.
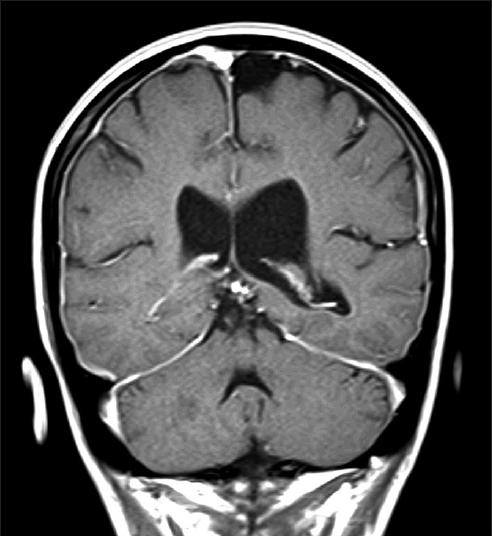
The patient was further assessed with an MRI of the brain with gadolinium. Diffuse smooth pachymeningeal enhancement over the cerebral convexities was consistent with meningeal hyperemia and intracranial hypotension[
Diagnostic intervention
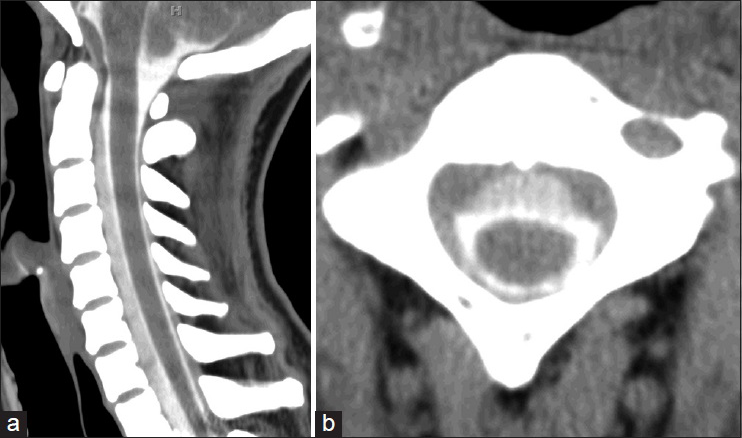
Efforts were then focused at identifying the source of the leak, as lumbar EBP had proved unsuccessful. CTM of the entire spinal axis demonstrated a subtly enhancing epidural fluid collection anterior to the cervical spinal cord [
Figure 2
Computed tomography (CT) of the cervical spine following intrathecal administration of contrast. (a) Sagittal and (b) axial CT demonstrates contrast anterior to the cervical thecal sac. This collection is attenuated in comparison to the intra-dural contrast. The presence of this ventral epidural fluid collection suggests cerebrospinal fluid-contrast egress
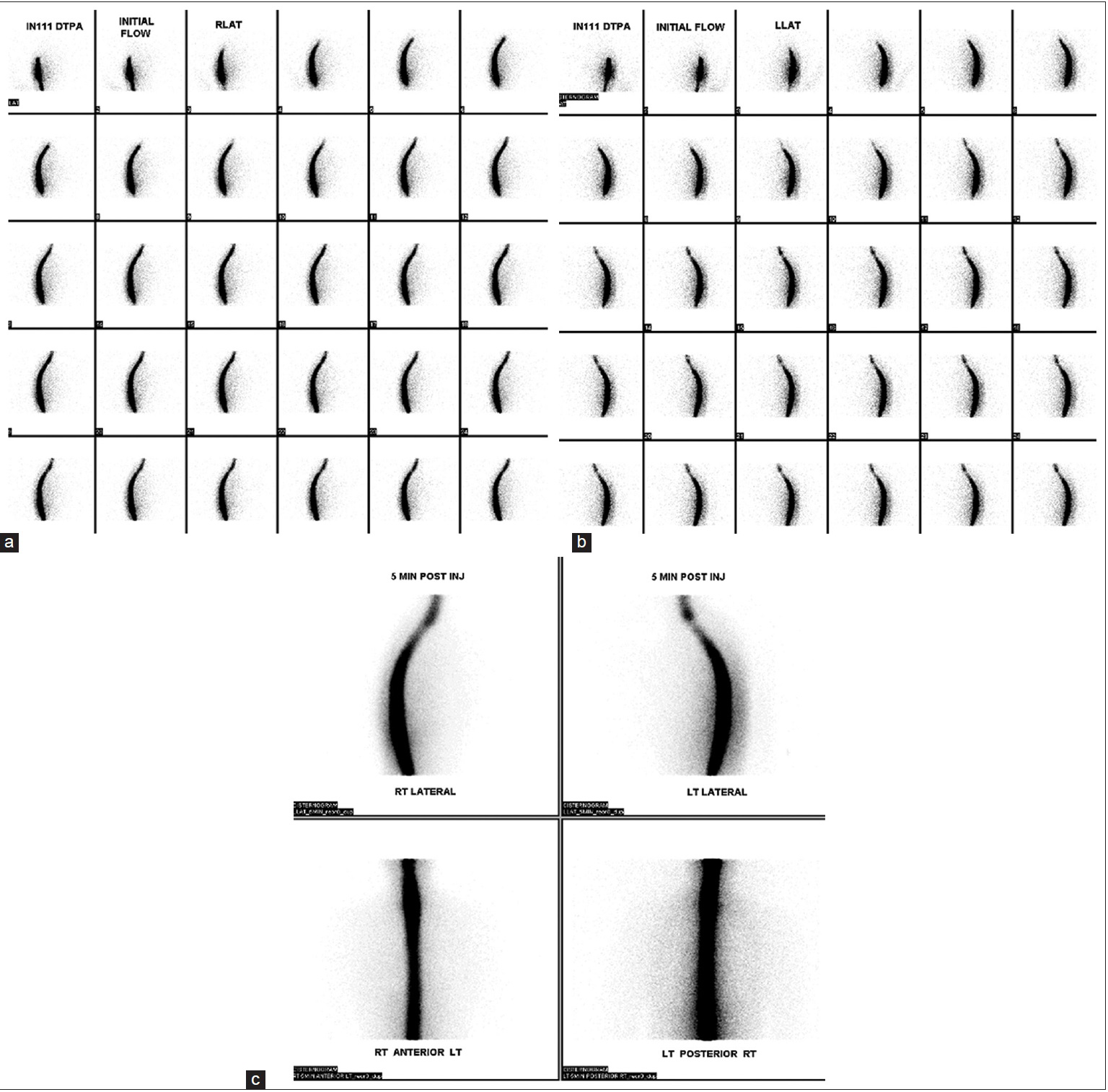
The patient was then brought to nuclear medicine for injection of radiotracer via the lumbar drain. The patient was placed in the left lateral position and two cubic centimeters (cc) of indium-111-diethyl-enetriamine penta-acetic acid radiotracer was administered via lumbar drain. Immediate postinjection static images revealed a photopenic region in the mid-cervical spine likely attributable to the extradural fluid accumulation seen on CTM [
Figure 3
Static nuclear medicine cerebrospinal cisternography following injection of indium-111-diethyl-enetriamine-penta-acetic acid. (a) Right and (b) left lateral initial static images as well as (c) 5 min delayed images were obtained following administration of radiotracer. No evidence of abnormal accumulation of radioisotope is seen with initial or delayed injections. A photopenic region is demonstrated in the mid-cervical spine suggesting extrinsic pressure on the cervical subarachnoid space and corresponding to the epidural fluid collection seen on computed tomography myelography
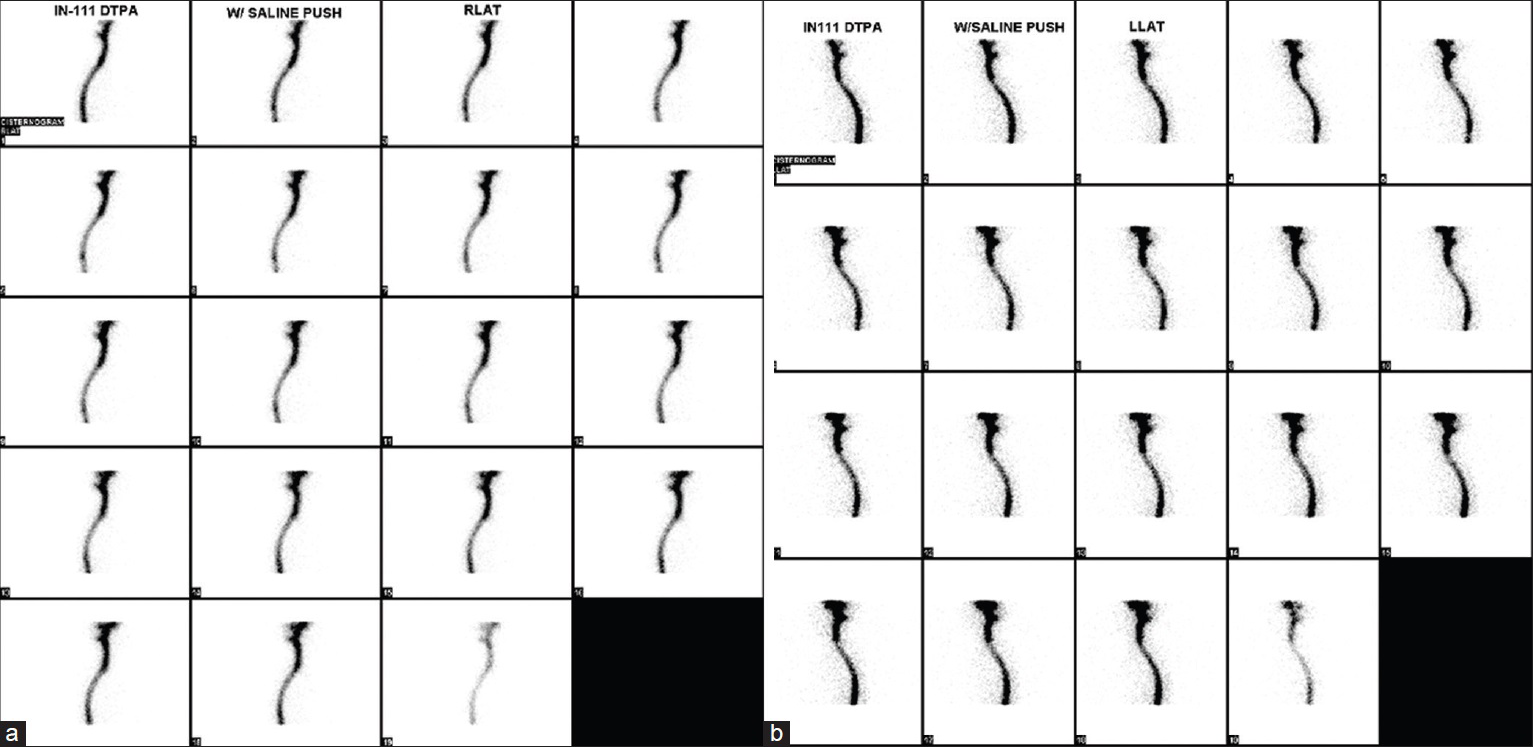
Figure 4
Dynamic nuclear medicine cerebrospinal cisternography following pressurized injection of saline through the lumbar drain. (a) Right and (b) left lateral views are obtained at the time of pressurized saline injection. Evidence of an abnormal accumulation of radioisotope is seen dorsally at C1-2 on both views
Surgical intervention
The patient was referred to the pain clinic for definitive treatment achieved by percutaneous, targeted epidural blood and fibrin patch. Postprocedure, the patient was kept on bed rest for 48 h, followed by a progression of activity as tolerated. She was discharged home on postoperative day six without headache.
DISCUSSION
Spontaneous CSF leaks can result from an abnormality in the cranial or spinal dura. Unlike those in the cranial dura in which patients present with otorrhea or rhinorrhea, spinal CSF leaks generally do not cause any local symptoms and remain undetected unless the diagnosis is actively pursued in a patient suspected of SIH.[
Spontaneous intracranial hypotension secondary to CSF hypovolemia is primarily a self-limited condition; most patients will improve with conservative management.[
The diagnosis of spontaneous CSF leak can be obtained by lumbar puncture with evidence of low CSF pressure. Variable readings, including pressures within the normal range, may be obtained if the CSF leak is intermittent.[
Radionuclide cisternography is also used to identify radioactivity outside the dural sac.[
The case presented here provides an alternative for addressing CSF leaks in which the flow characteristics are slow or intermittent, and thus below the resolution of study for “standard static imaging.” The authors modify the use of an already widely accepted form of neuroimaging for SIH (i.e., RIC) in order to identify cryptic CSF leaks.
The use of pressurized RIC to identify the precise location of the CSF leak offers some notable diagnostic advantages to practitioners that may encounter this entity. First, it allows the clinician to obtain a panoramic view[
Historically, RIC has been used as a means of confirming SIH when the accumulation of radioactivity is noted outside the subarachnoid space. Its utility was first applied in the setting of SIH when early accumulation of radiotracer in the urinary bladder and kidneys suggested extravasation of intrathecal tracer with reabsorption via the epidural venous plexus.[
Increasing support for targeted treatment in SIH is found in the literature, especially when initial lumbar epidural blood patching fails to resolve symptoms. Defining the CSF leak as secondary to dural rent or meningeal diverticulum, allows choice of the most appropriate management, whether by targeted percutaneous blood patch or open surgical treatment. EBP is the treatment of choice in patients who have failed an initial trial of conservative management.[
CONCLUSIONS
Slow flow or intermittent CSF leaks represent a diagnostic challenge. Failing to establish a diagnosis and localize the area of a dural breach can lead to disability and chronic pain for patients. Pressurized RIC for spinal CSF leaks offers a means of identifying CSF leaks that were previously considered beyond the resolution of standard imaging. Furthermore, this test can be performed with relatively low risk to the patient, as lumbar drain placement is commonplace in neurosurgical practice. Most importantly, this technique provides a means of avoiding excessive testing in patients with signs of SIH and no identifiable source of CSF leak.
References
1. Ali SA, Cesani F, Zuckermann JA, Nusynowitz ML, Chaljub G. Spinal-cerebrospinal fluid leak demonstrated by radiopharmaceutical cisternography. Clin Nucl Med. 1998. 23: 152-5
2. Angelo F, Giuseppe M, Eliana M, Luisa C, Gennaro B. Spontaneous intracranial hypotension: Diagnostic and therapeutic implications in neurosurgical practice. Neurol Sci. 2011. 32: S287-90
3. Beleña JM, Nuñez M, Yuste J, Plaza-Nieto JF, Jiménez-Jiménez FJ, Serrano S. Spontaneous intracranial hypotension syndrome treated with a double epidural blood patch. Acta Anaesthesiol Scand. 2012. 56: 1332-5
4. Brady-McCreery KM, Speidel S, Hussein MA, Coats DK. Spontaneous intracranial hypotension with unique strabismus due to third and fourth cranial neuropathies. Binocul Vis Strabismus Q. 2002. 17: 43-8
5. Curnes JT, Vincent LM, Kowalsky RJ, McCartney WH, Staab EV. CSF rhinorrhea: Detection and localization using overpressure cisternography with Tc-99m-DTPA. Radiology. 1985. 154: 795-9
6. Ferrante E, Savino A, Brioschi A, Marazzi R, Donato MF, Riva M. Transient oculomotor cranial nerves palsy in spontaneous intracranial hypotension. J Neurosurg Sci. 1998. 42: 177-9
7. Fishman RA, Dillon WP. Dural enhancement and cerebral displacement secondary to intracranial hypotension. Neurology. 1993. 43: 609-11
8. Hayek SM, Fattouh M, Dews T, Kapural L, Malak O, Mekhail N. Successful treatment of spontaneous cerebrospinal fluid leak headache with fluoroscopically guided epidural blood patch: A report of four cases. Pain Med. 2003. 4: 373-8
9. Hoxworth JM, Trentman TL, Kotsenas AL, Thielen KR, Nelson KD, Dodick DW. The role of digital subtraction myelography in the diagnosis and localization of spontaneous spinal CSF leaks. AJR Am J Roentgenol. 2012. 199: 649-53
10. Huang C, Chuang Y, Lee C, Lee R, Lin T. Spontaneous spinal cerebrospinal fluid leak and intracranial hypotension. Clin Imaging. 2000. 24: 270-2
11. Hyun SH, Lee KH, Lee SJ, Cho YS, Lee EJ, Choi JY. Potential value of radionuclide cisternography in diagnosis and management planning of spontaneous intracranial hypotension. Clin Neurol Neurosurg. 2008. 110: 657-61
12. Kamada M, Fujita Y, Ishii R, Endoh S. Spontaneous intracranial hypotension successfully treated by epidural patching with fibrin glue. Headache. 2000. 40: 844-7
13. Kantor D, Silberstein SD. Cervical epidural blood patch for low CSF pressure headaches. Neurology. 2005. 65: 1138-
14. Leep Hunderfund AN, Mokri B. Second-half-of-the-day headache as a manifestation of spontaneous CSF leak. J Neurol. 2012. 259: 306-10
15. Magnaes B, Solheim D. Controlled overpressure cisternography to localize cerebrospinal fluid rhinorrhea. J Nucl Med. 1977. 18: 109-11
16. Mokri B. Spontaneous cerebrospinal fluid leaks: From intracranial hypotension to cerebrospinal fluid hypovolemia – Evolution of a concept. Mayo Clin Proc. 1999. 74: 1113-23
17. Mokri B. Spontaneous intracranial hypotension. Curr Neurol Neurosci Rep. 2001. 1: 109-17
18. Moriyama E, Ogawa T, Nishida A, Ishikawa S, Beck H. Quantitative analysis of radioisotope cisternography in the diagnosis of intracranial hypotension. J Neurosurg. 2004. 101: 421-6
19. Pleasure SJ, Abosch A, Friedman J, Ko NU, Barbaro N, Dillon W. Spontaneous intracranial hypotension resulting in stupor caused by diencephalic compression. Neurology. 1998. 50: 1854-7
20. Rando TA, Fishman RA. Spontaneous intracranial hypotension: Report of two cases and review of the literature. Neurology. 1992. 42: 481-7
21. Schievink WI, Gordon OK, Tourje J. Connective tissue disorders with spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension: A prospective study. Neurosurgery. 2004. 54: 65-70
22. Schievink WI, Louy C. Precipitating factors of spontaneous spinal CSF leaks and intracranial hypotension. Neurology. 2007. 69: 700-2
23. Schievink WI, Maya MM, Louy C, Moser FG, Tourje J. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. AJNR Am J Neuroradiol. 2008. 29: 853-6
24. Schievink WI, Meyer FB, Atkinson JL, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996. 84: 598-605
25. Schievink WI, Moser FG, Pikul BK. Reversal of coma with an injection of glue. Lancet. 2007. 369: 1402-
26. Schievink WI, Smith KA. Nonpositional headache caused by spontaneous intracranial hypotension. Neurology. 1998. 51: 1768-9
27. Schievink WI, Wijdicks EF, Meyer FB, Sonntag VK. Spontaneous intracranial hypotension mimicking aneurysmal subarachnoid hemorrhage. Neurosurgery. 2001. 48: 513-6
28. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006. 295: 2286-96
29. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks. Cephalalgia. 2008. 28: 1345-56
30. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks: A review. Neurosurg Focus. 2000. 9: e8-
31. Sencakova D, Mokri B, McClelland RL. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001. 57: 1921-3
32. Stone JA, Castillo M, Neelon B, Mukherji SK. Evaluation of CSF leaks: High-resolution CT compared with contrast-enhanced CT and radionuclide cisternography. AJNR Am J Neuroradiol. 1999. 20: 706-12
33. Szeinfeld M, Ihmeidan IH, Moser MM, Machado R, Klose KJ, Serafini AN. Epidural blood patch: Evaluation of the volume and spread of blood injected into the epidural space. Anesthesiology. 1986. 64: 820-2
34. Vishteh AG, Schievink WI, Baskin JJ, Sonntag VK. Cervical bone spur presenting with spontaneous intracranial hypotension. Case report. J Neurosurg. 1998. 89: 483-4
35. Yoo HM, Kim SJ, Choi CG, Lee DH, Lee JH, Suh DC. Detection of CSF leak in spinal CSF leak syndrome using MR myelography: Correlation with radioisotope cisternography. AJNR Am J Neuroradiol. 2008. 29: 649-54