- Department of Neurosurgery, Atal Bihari Vajpeyi Institute of Medical Sciences and RML Hospital, Delhi,
- Department of Pathology, Atal Bihari Vajpeyi Institute of Medical Sciences and RML Hospital, Delhi,
- Department of Neurosurgery, Atal Bihari Vajpeyi Institute of Medical Sciences, Noida,
- Department of Neurosurgery, Atal Bihari Vajpeyi Institute of Medical Sciences, Ghaziabad, Uttar Pradesh, India.
Correspondence Address:
Ajay Choudhary, Departments of Neurosurgery, Atal Bihari Vajpeyi Institute of Medical Sciences and RML Hospital, Delhi, India.
DOI:10.25259/SNI_512_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kaviraj Kaushik1, Ajay Choudhary1, Arvind Ahuja2, Rahul Varshney3, Rajesh Sharma4. Camalote sign in intraventricular hydatid cyst: A rare presentation of uncommon disease. 25-Oct-2021;12:541
How to cite this URL: Kaviraj Kaushik1, Ajay Choudhary1, Arvind Ahuja2, Rahul Varshney3, Rajesh Sharma4. Camalote sign in intraventricular hydatid cyst: A rare presentation of uncommon disease. 25-Oct-2021;12:541. Available from: https://surgicalneurologyint.com/surgicalint-articles/11196/
Abstract
Background: Hydatid cyst is a common zoonotic condition in endemic areas. Intraventricular hydatid cyst is a rare entity with less than 50 cases published in literature. Floating water lily sign (also called Camalote sign) is very rare in intracranial hydatid cysts. Only a single case report of this sign exists in literature in intraventricular hydatidosis suggesting rupture of hydatid cyst leading to CSF dissemination and frequent poor outcome.
Case Description: This case report describes the successful management of a 5-year-old child who presented with signs and symptoms of raised intracranial pressure due to large intraventricular hydatid cyst in the right frontal horn, and magnetic resonanace imaging of the brain showed hydatid cyst with typical camalote sign.
Conclusion: Although very rare, the presence of camalote sign in intraventricular cysts is very categorical in establishing preoperative diagnosis of hydatid cyst, especially in endemic areas.
Keywords: Camalote sign, Floating water lily sign, Hydatid cyst, Intraventricular cyst
INTRODUCTION
Cerebral hydatid cysts involve <2% of intracranial space-occupying lesions, usually located in supratentorial white matter.[
CASE REPORT
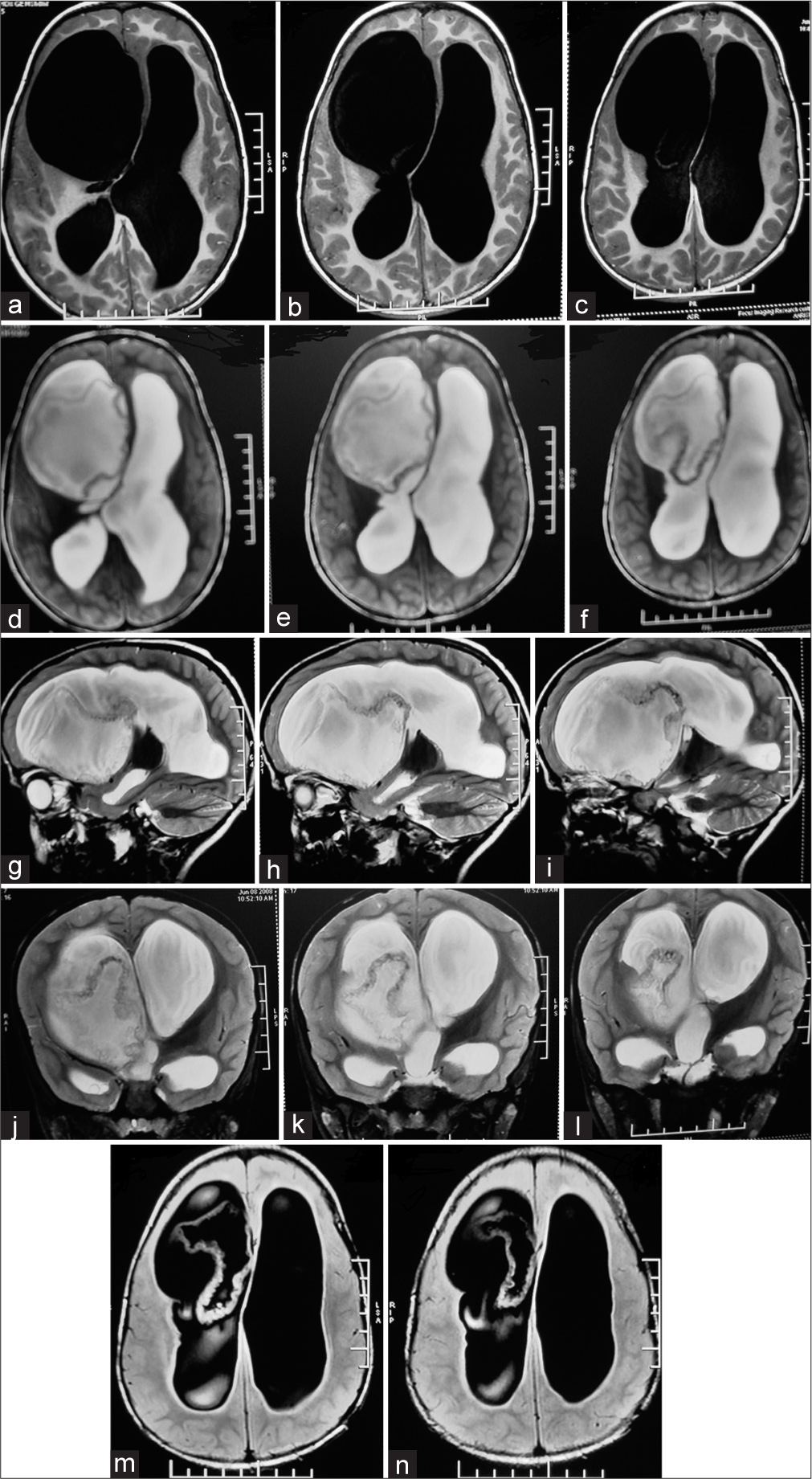
A 5-year-old male child was brought to our department with chief complaints of holocranial headache, irritability, occasional vomiting for 3 months, and altered sensorium for 3 days. On examination, patient was in altered sensorium with GCS of E3V4M6. Magnetic resonanace imaging (MRI) brain were suggestive of a large ruptured intraventricular cyst with irregular floating cyst wall in the right frontal horn giving a typical Camalote sign appearance [
Figure 1:
(a-c) T1 MRI axial image sequences showing hypointense intraventricular cyst 1 (d-f) T2 MRI axial image sequences showing hyperintense intraventricular cyst with ruptured hypointense wall in the right lateral ventricle (Camalote sign) 1 (g-i) T2 MRI Saggital image sequences again showing the ruptured cyst and cyst wall sedimenting down 1 (j-l) T2 MRI Coronal image sequences confirming the ruptured hydatid cyst1. (m and n) MRI FLAIR images in axial cuts distinctly defining the cyst wall.
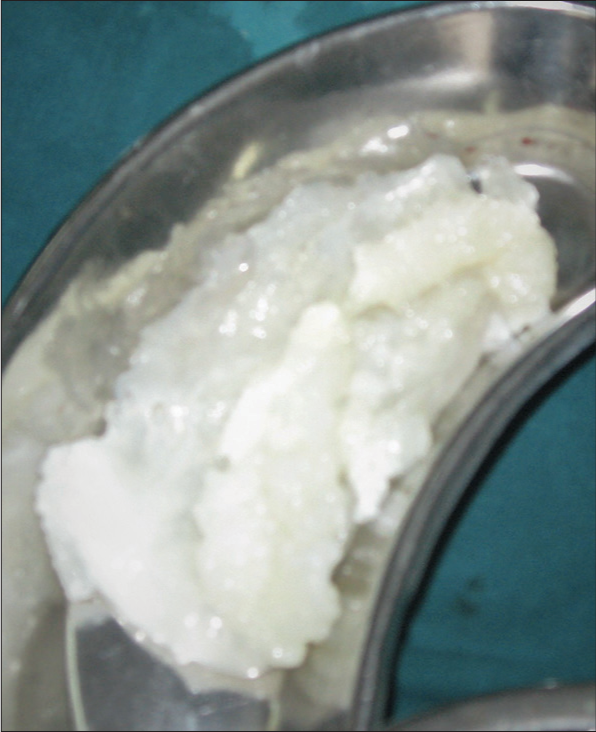
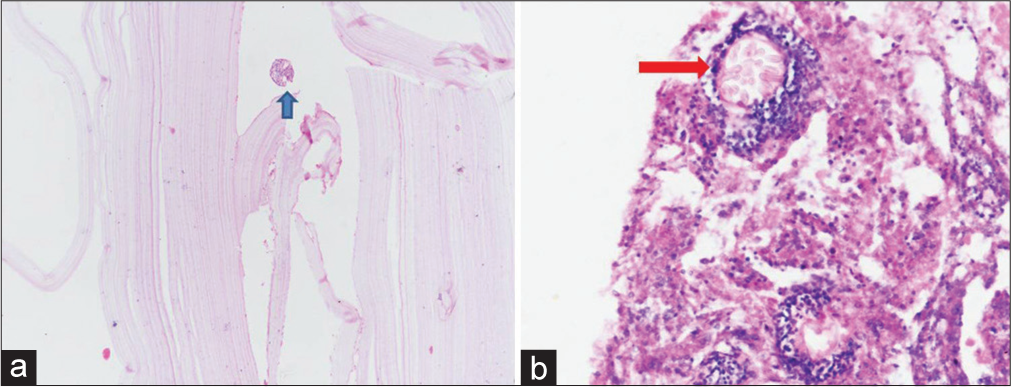
Histopathology also confirmed the diagnosis [
DISCUSSION
Hydatidosis is common endemic zoonotic condition in grazing areas of world caused by flatworm cystodes: Echinococcus granulosus (unilocular) and Echinococcus multilocularis (alveolar form). Humans as accidental hosts, ingest larval form of Echinococcus with contaminated food. From the intestine, they are taken to liver through portal circulation, from where they may spread to different parts of body through systemic circulation. Common site of involvement is intraparenchymal especially MCA territory distribution (most common in parietal lobes) where it reaches as embolic spread.[
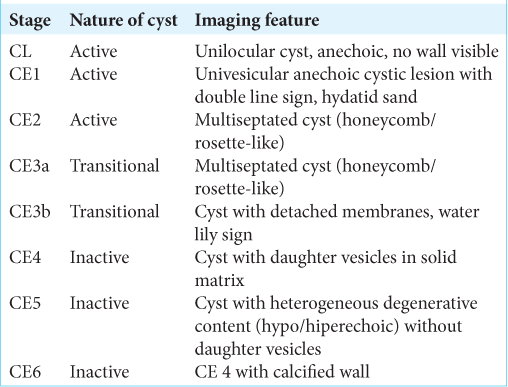
World Health Organisation has classified pericyst being made up of host tissues without surrounding edema. The cyst wall do not enhance with contrast imaging except in rare cases having secondary infection in cyst. The WHO classifies hydatid cyst in the six stages on basis of its evolution [
Computed tomography (CT) and MRI features of hydatid cyst are of a spherical well defined, thin walled, homogenous cystic lesion with CSF like fluid density. These imaging features mandates ruling out differential diagnosis of arachnoid cyst, dermoid or epidermoid cyst. Calcification or septations may be present rarely. Presence of daughter cyst is pathognomonic for hydatid cyst but uncommon in radiology.
Conventional water lily sign is present on ultrasound, X-rays, CT scan or MRI in stage 3A when the endocyst wall is detached from the pericyst and floats freely into the cystic fluid.[
The conventional Dowling’s technique has been described with an aim to take out the intact cyst by hydrostatic expulsion holds good for parenchymal cysts. However, intraoperative rupture has been described in around 25% of cases even with the use of this technique.[
CONCLUSION
Intraventricular location of hydatid cyst is very uncommon but it should be kept as a differential diagnosis especially in endemic areas. The presence of camalote sign on imaging in such rare sites is very helpful in confirming the diagnosis preoperatively for appropriate surgical planning in such cases.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Copley IB, Fripp PJ, Erasmus AM, Otto DD. Unusual presentations of cerebral hydatid disease in children. Br J Neurosurg. 1992. 6: 203-10
2. Golzari SE, Sokouti M. Pericyst: The outermost layer of hydatid cyst. World J Gastroenterol. 2014. 20: 1377-8
3. Grecu I, Rizea O, Lupescu IG.editors. The Water Lily Sign: A Specific and Valuable Imaging Feature Poster No. C-1246. 2017. p.
4. Guzel A, Tatli M, Maciaczyk J, Altinors N. Primary cerebral intraventricular hydatid cyst: A case report and review of the literature. J Child Neurol. 2008. 23: 585-8
5. Hajhouji F, Aniba K, Laghmari M, Lmejjati M, Ghannane H, Benali SA. Epilepsy: Unusual presentation of cerebral hydatid disease in Children. Pan Afr Med J. 2016. 25: 58
6. Krüger J, Ritz A, Ingunza W, Frowein RA, Wilcke O, Karimi-Nejad A, Brock M, Klinger M.editors. A case of intraventricular hydatid cyst. Head Injuries. Tumors of the Cerebellar Region. Advances in Neurosurgery. Berlin, Heidelberg: Springer; 1978. 5:
7. Oscar H, Brutto D, Figueroa JF, Garcia HH.editors. Parasaitic infections. Youmans and Winn Neurological Surgery. Amsterdam, Netherlands: Elsevier; 2017. p. 354-5
8. .editors. PAIR: Puncture, Aspiration, Injection, Re-Aspiration. An Option for the Treatment of Cystic Echinococcosis. 2021. p.
9. Pandey S, Pandey D, Shende N, Sahu A, Sharma V. Cerebral intraventricular echinococcosis in an adult. Surg Neurol Int. 2015. 6: 138
10. Sadashiva N, Shukla D, Devi BI. Rupture of intraventricular hydatid cyst: Camalote sign. World Neurosurg. 2018. 110: 115-6
11. Singounas EG, Leventis AS, Sakas DM, Lampadarios DA, Karvounis PC. Successful treatment of intracerebral hydatid cysts with albendazole: Case report and review of the literature. Neurosurgery. 1992. 31: 571-4
12. Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W. Diagnosing and staging of cystic echinococcosis: How do CT and MRI perform in comparison to ultrasound?. PLoS Negl Trop Dis. 2012. 6: e1880
13. Thakur SH, Joshi PC, Kelkar AB, Seth N. Unusual presentation of hydatid cyst-ruptured intraventricular hydatid. Indian J Radiol Imaging. 2017. 27: 282-5