- Department of Neurosurgery, Kagawa Rosai Hospital, Marugame City, Kagawa, Japan.
DOI:10.25259/SNI_319_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masatoshi Yunoki, Michiari Umakoshi, Masaki Tatano, Ryoji Imoto. Cauda equina syndrome due to lumbar disc herniation and ossification of the yellow ligament. 03-May-2021;12:202
How to cite this URL: Masatoshi Yunoki, Michiari Umakoshi, Masaki Tatano, Ryoji Imoto. Cauda equina syndrome due to lumbar disc herniation and ossification of the yellow ligament. 03-May-2021;12:202. Available from: https://surgicalneurologyint.com/surgicalint-articles/10782/
Abstract
Background: Patients with lumbar disc herniation at a level with significant stenosis due to ossification of the yellow ligament (OYL) may rarely present with rapid neurological deterioration warranting emergent surgery.
Case Description: A 40-year-old female developed an acute cauda equina syndrome (CES) attributed to an acute lumbar disc herniation and to marked canal stenosis due to OYL. As the patient underwent a 9 h delayed removal of the ossified ligament and discectomy, she sustained only minimal recovery.
Conclusion: Patients diagnosed with acute lumbar disc herniation and severe stenosis due to OYL who present with acute CES warrant emergent surgical decompression to avoid permanent postoperative neurological sequelae.
Keywords: Cauda equina syndrome, Lumbar disc herniation, Ossification of the yellow ligament
INTRODUCTION
Patients with significant lumbar stenosis due to ossification of the yellow ligament (OYL) and an acute lumbar disc herniation may acutely develop new neurological deficits.[
CASE PRESENTATION
Fifteen years ago, this now 40-year-old female had undergone a L5S1 discectomy [
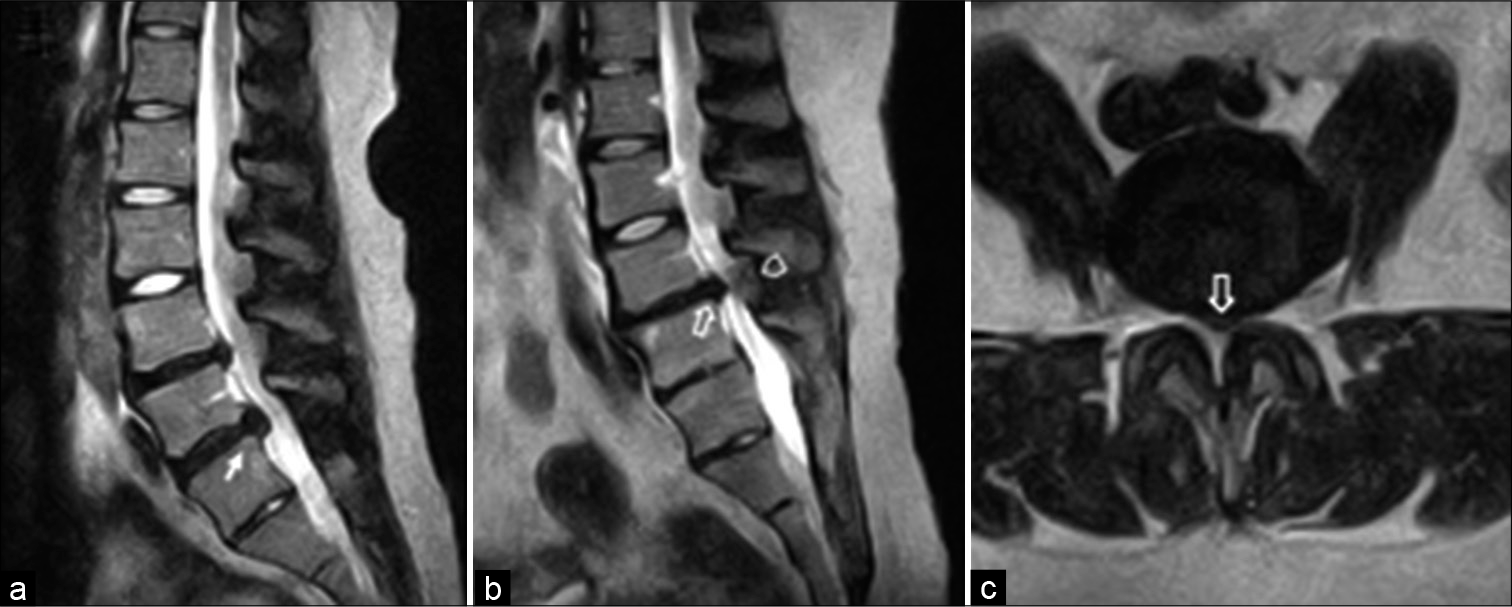
Figure 1:
Mid-sagittal T2-weighted magnetic resonance imaging (MRI) 15 years before admission showed an L5/S1 disc herniation (on of the Yellow Ligament. or longitudinal (a). Mid-sagittal and axial T2-weighted MRI 10 months before admission demonstrated cauda equina compression at L4/5 caused by a hypointense anterior central disc herniation (⇧) and a posterior isointense lesion (⌂) (b and c).
MR findings
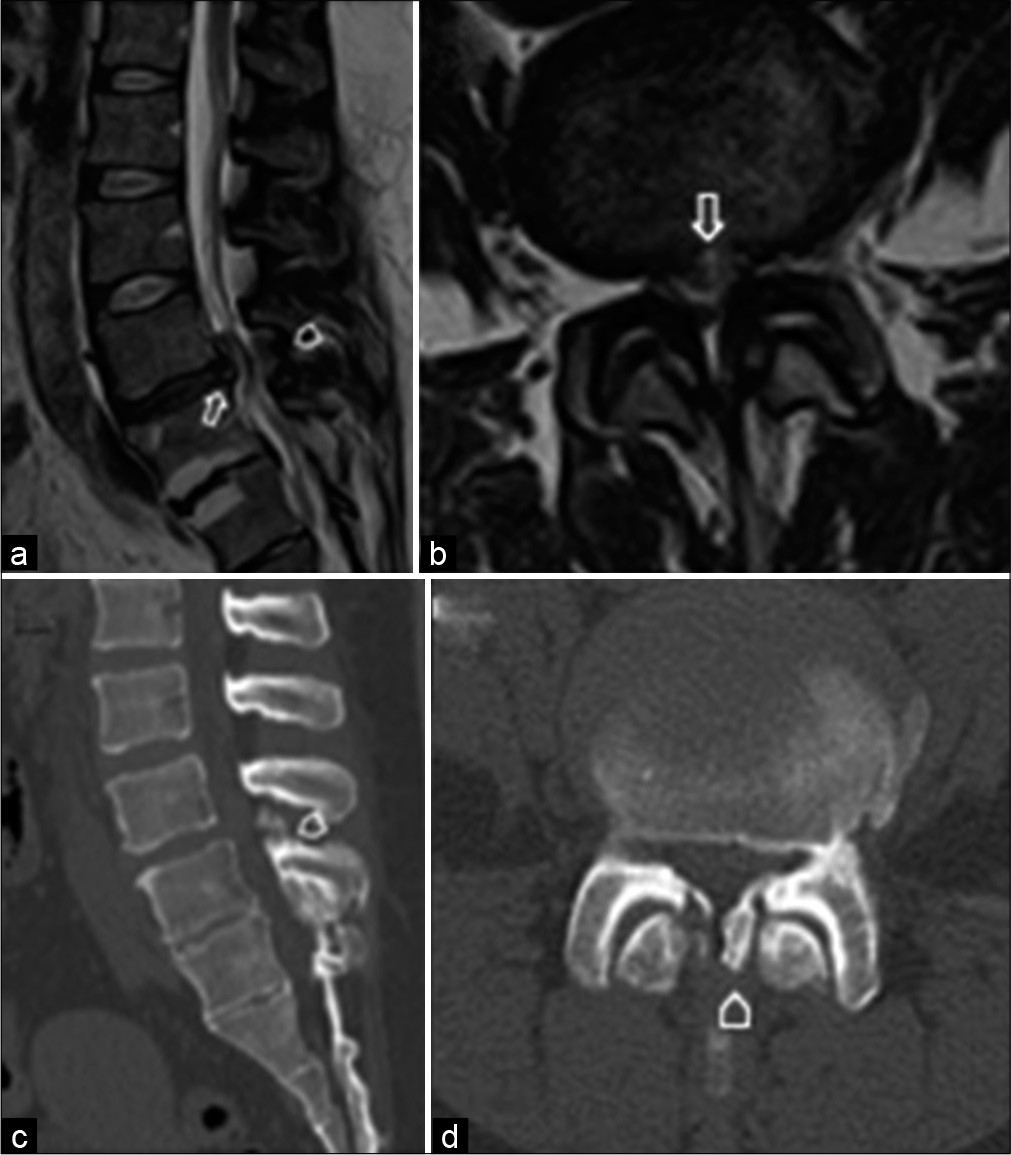
The new magnetic resonance imaging (MRI) and CT both demonstrated worsening of her L4-L5 cauda equina compression due the large central disc herniation and severe stenosis/OYL; the CT further confirmed ossification of the OYL [
Figure 2:
Mid-sagittal and axial T2-weighted magnetic resonance imaging after hospital admission demonstrated cauda equina compression caused by progression of the L4/5 disc herniation (⇧) (a and b). Mid-sagittal and axial computed tomography (CT) revealed ossification of the yellow ligament at the L4/5 level (⌂) (c and d).
Delayed surgery
Notably, the patient should have undergone emergent surgery following the completion of the MR/CT studies. However, surgery was delayed for 9 h by which time she was fully paraplegic (0/5 motor function, L4-S1 loss of sensation, and urinary retention (JOA 2/29).
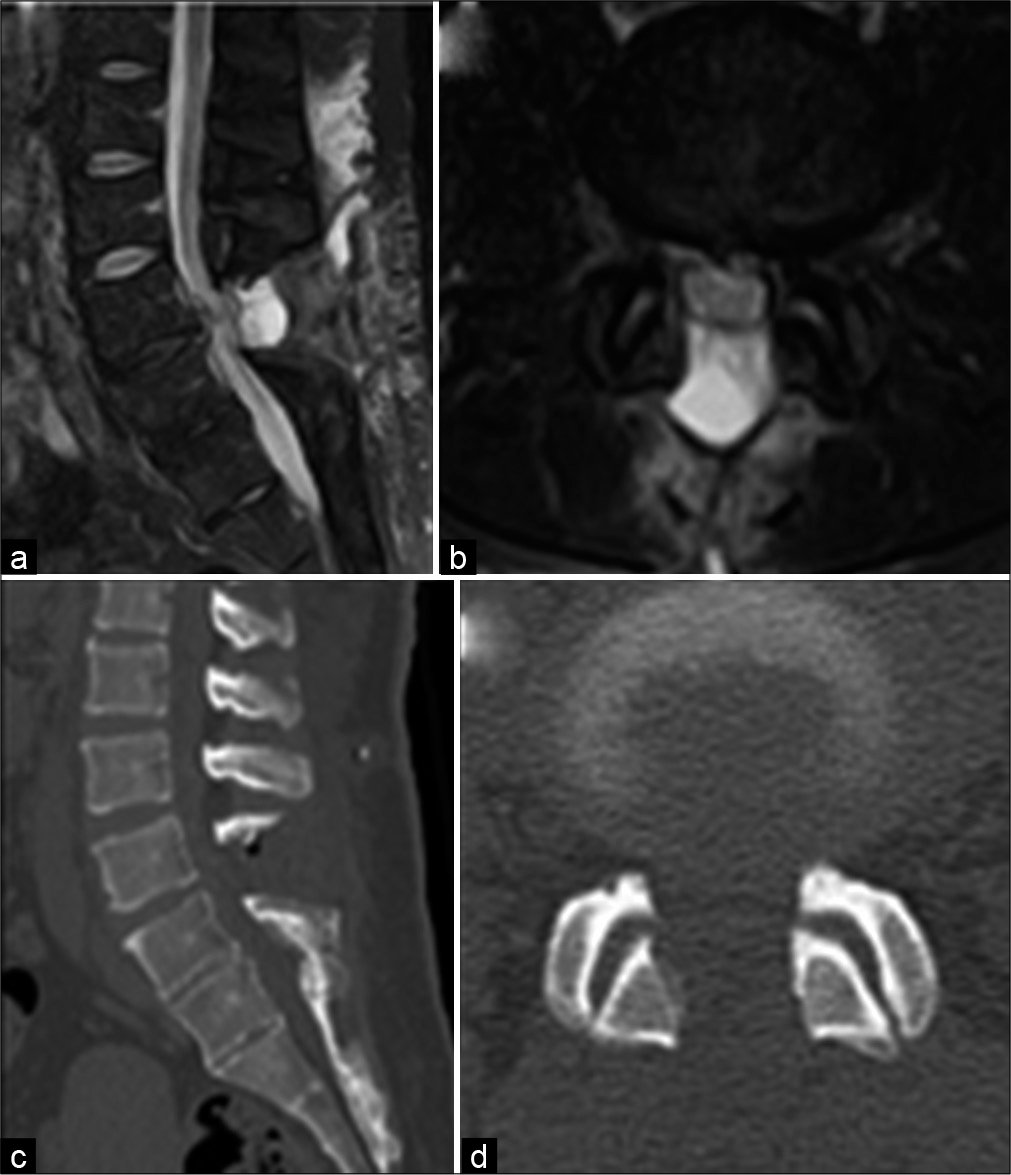
Following a L4-L5 laminectomy for stenosis, OYL, and a partial central discectomy (i.e., not completely removed because of its central location), the patient never fully recovered; she had just 1/5 motor function bilaterally (i.e., residual loss perineal sensation and urinary incontinence – final JOA score 9/29) 1 month later. Of interest, the postoperative MR and CT studies, despite showing mild residual ventral disc, confirmed adequate cauda equina decompression [
DISCUSSION
Lumbar OYL with acute disc herniation
Significant lumbar stenosis attributed to preexisting OYL may be acutely exacerbated by the development of an acute lumbar disc herniation; together, these factors may result in a rapidly progressive CES.[
Treatment of lumbar CES due to lumbar stenosis/disk disease
Many surgeons find that CES typically warrants acute lumbar decompressive surgery, while others advocate operating within 48 h of its’ onset.[
Here, our patient unfortunately underwent delayed surgery, 9 h after presenting to an emergency room with an evolving paraparetic deficit and MR/CT documentation of an L4-L5 CES; this indue delay resulted in only a very limited recovery. Here, therefore, the authors concluded that in the future, early surgery for CES (e.g., in this case attributed to an acute L4-L5 disc and stenosis/OYL) is critical to avoid postoperative residual neurological sequelae.
CONCLUSION
A 40-year-old female with marked L45 lumbar stenosis/ OYL due to a large ventral central disc herniation developed an acute CES. However, surgery was delayed 9 h following her original presentation to an emergency room, and this failure resulted in her significant permanent residual CES/ paraparesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda equina syndrome secondary to lumbar disc herniation: A meta-analysis of surgical outcomes. Spine (Phila Pa 1976). 2000. 25: 1515-22
2. Epstein N. Ossification of the yellow ligament and spondylosis and/or ossification of the posterior longitudinal ligament of the thoracic and lumbar spine. J Spinal Disord. 1999. 12: 250-6
3. Kennedy JG, Soffe KE, McGrath A, Stephens MM, Walsh MG, McManus F. Predictors of outcome in cauda equina syndrome. Eur Spine J. 1999. 8: 317-22
4. Yara T, Kise H, Kuniyoshi S, Ibaraki K, Takara H. Two cases of thoracic herniation associated with ossification of the yellow ligament. Orthop Traumatol. 1992. 41: 385-90