- Departments of Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
- Departments of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
- Departments of Wolff Center, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Enyinna L. Nwachuku
Departments of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_377_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Enyinna L. Nwachuku1, Kevin P. Patel2, Audrey L. Paul3, Robert M. Friedlander2, Peter C. Gerszten2. Causes of hospital readmissions within 7 days from the neurosurgical service of a quaternary referral hospital. 01-Aug-2020;11:226
How to cite this URL: Enyinna L. Nwachuku1, Kevin P. Patel2, Audrey L. Paul3, Robert M. Friedlander2, Peter C. Gerszten2. Causes of hospital readmissions within 7 days from the neurosurgical service of a quaternary referral hospital. 01-Aug-2020;11:226. Available from: https://surgicalneurologyint.com/surgicalint-articles/10181/
Abstract
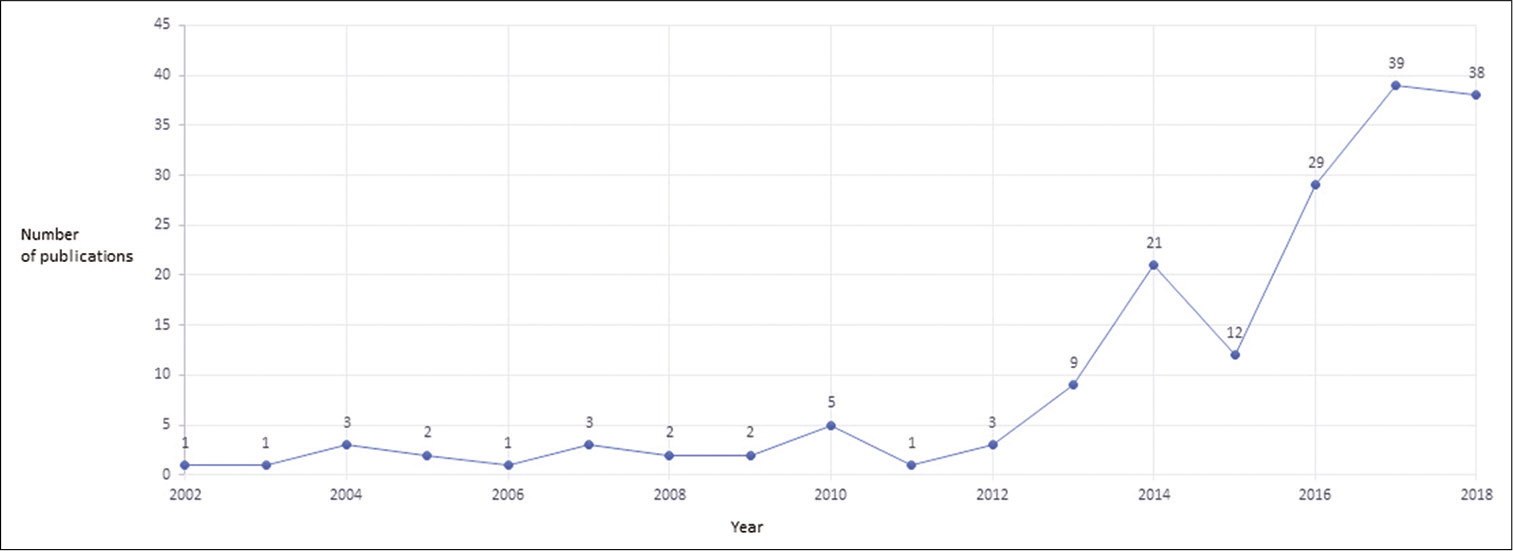
Background: Evaluation of readmission rates as a proxy metric of health-care quality in neurological surgery has grown to become a prevalent area of investigation in the last several years. Significant attention has been paid to 30-day readmission rates due to the financial incentive to health-care providers following the enforcement of the penalties created by the Affordable Care Act. However, relatively little attention has been paid to patients readmitted within 7 days of discharge to large quaternary neurological surgery services. This study was conducted to examine the causes and unique characteristics of 7-day readmission rates from a neurosurgical service at a large quaternary referral hospital.
Methods: A retrospective observational analysis of all 7-day readmissions to the neurosurgical surgery service of the University of Pittsburgh Medical Center, Presbyterian Hospital from August 2017 to June 2019, was performed. Patients were organized into seven categories based on their primary reason for readmission: scheduled surgeries, infection, pain, altered mental status or seizures, general postoperative complications, complications directly resulting from a neurosurgical intervention, and unrelated reasons. Demographic information, the time between initial discharge and subsequent readmission, and discharge disposition were also recorded.
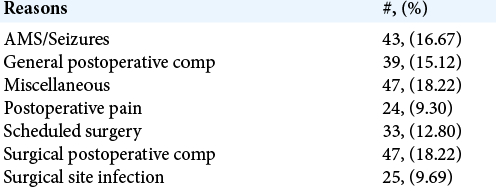
Results: Of 5274 discharges, 258 patients (4.9%) were readmitted within 7 days (55.0% male; mean age 60 years of age). Two-thirds of patients readmitted initially underwent care for cranial pathologies (57% of 258 patients) as opposed to a third for spine pathologies (33% of 258 patients). Complications that directly arose from the neurosurgical intervention (e.g., shunt infection or misplacement, and hardware misplacement) represented 18.9% of total readmission, while general postoperative complications (e.g., urinary tract infection) accounted for 15.1% of total readmission, in which all together were slightly greater than a third of readmissions. Seizures or altered mental status led to less than a fifth of readmissions (17.0%), followed by readmissions from unrelated diagnosis or miscellaneous reasons (17.0%) and scheduled surgeries (13.1%). Taken together, surgical site infections (9.7%) and postoperative pain (9.3%) accounted for 9.7% and 9.3 % of readmissions, respectively.
Conclusion: Approximately 5% of patients discharged in a single year from our quaternary referral center were readmitted within 7-days. Approximately 90% of all 7-day readmissions were unplanned, with one-third resulting directly from perioperative complications. Further investigation to better understand this acutely vulnerable yet previously overlooked population may guide focused efforts to increase the quality of neurosurgical patient care.
Keywords: Complications, General neurosurgery, Hospital disposition, Readmission
INTRODUCTION
Several recent studies suggest that the average cost of general medical readmission was $2200,[
In addition, concerning is the fact that other surgical specialties have witnessed a decline in readmission rates over time, whereas reductions in readmissions for neurological surgery have plateaued and, in some cases, even increased.[
Beyond just their financial burden, evidence suggests that neurosurgical readmissions are associated with significant morbidities, reductions in quality of life, and increased mortality10. Understanding financial and labor costs associated with 30-day readmissions in neurological surgery have resulted in a significant increase in the surveillance of such readmissions. However, the controversy surrounding the use of these rates by HPPR to penalize hospitals has also invited scrutiny of 30-day readmission rates in neurological surgery as a health-care quality metric.[
To the best of our knowledge, the present observational study of 7-day readmissions in neurological surgery is the first of its kind. Three goals were identified at its outset: (1) to identify and better characterize a poorly understood population of patients being readmitted from a neurological surgery service, (2) to decrease the overall readmission rate of all discharged patients from our neurological service, and (3) to guide future efforts to identify the causal mechanisms underlying 7-day readmissions in neurological surgery.
MATERIALS AND METHODS
Analysis
A retrospective observational study of 7-day readmissions between August 2017 and June 2019 to the neurosurgical service of the University of Pittsburgh Medical Center, Presbyterian Hospital (UPMC-PUH), was conducted.
Database
All data were approved for use by the Total Quality and Patient Safety Council as a quality improvement initiative for the department of neurological surgery at UPMC. Eighteen different attending level providers cared for this patient cohort.
Demographic information
Demographic data were collected for all patients: age, sex, and interval number of days between initial discharge and subsequent readmission, along with the patients’ discharge disposition were recorded.
Coding scheme
The primary reason for readmission was organized using a seven-category system: surgical site infection, pain, altered mental status/seizures, postoperative complication, and “unrelated.” These categories were constructed anecdotally based on the clinical observation that comprehensively covers reasons for readmission at UPMC Presbyterian Hospital (PUH). Statistical analyses were organized and conducted through the Microsoft Excel spreadsheet. Figures and graphics were constructed with Tableau.
Data acquisition and anonymization
Batched data of all readmissions to the UPMC-PUH neurosurgery service between August 2017 and June 2019 were graciously provided by the were password protected and anonymized consistent with institutional standards and HIPAA guidelines.
Eligibility
All patients aged 18 or older who were readmitted between August 2017 and June 2019 to the UPMC-PUH Neurological Surgery service within 7-days of their initial discharge were included in our dataset.
RESULTS
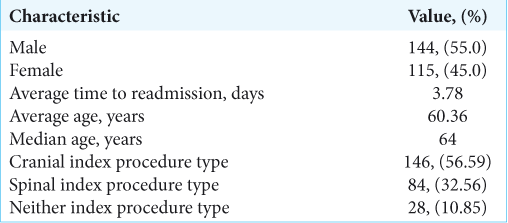
Between July 2017 and June 2019, 5274 patient discharges were performed. During this time, 258 patients (4.9%) were readmitted within 7 days (55.0% men; mean age 60 years) [
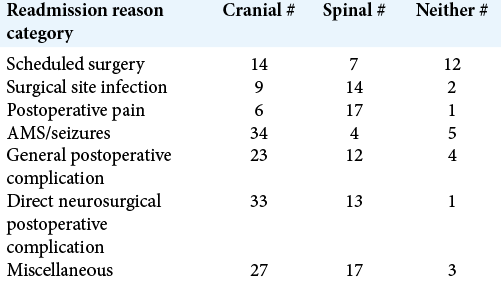
Two-hundred thirty patients out of 258 who were readmitted either underwent cranial (57%) or spinal (32.5%) surgery with miscellaneous procedures accounting for the remaining 11% [
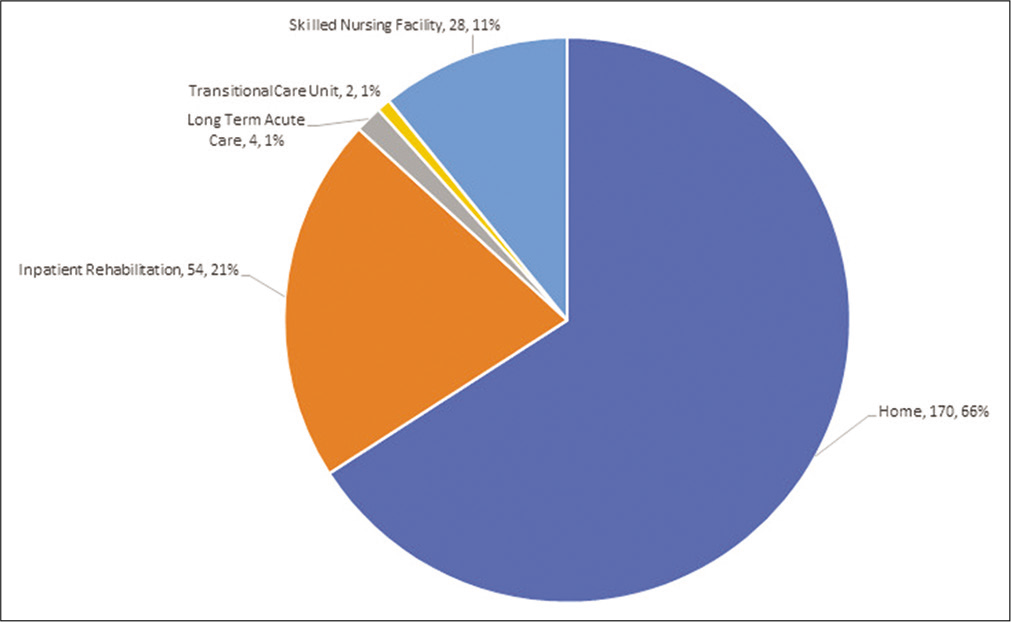
Approximately 66% of patients discharged following inpatient hospitalizations on the neurological surgery service were discharged to home [
DISCUSSION
The aim of this retrospective study was to better understand the reasons that patients were readmitted to the neurological surgery service of a large quaternary referral hospital within 7 days of readmission. The 7-day all-cause readmission rate was nearly 5%. Many interesting points of discussion were revealed from this investigation. It was noted that 57% of readmissions within 7-days resulted from patients who underwent a cranial procedure; the remaining cohorts represented spinal (32%) and miscellaneous interventions (11%). Classically, a significant amount of outpatient resources, both from orthopedic and neurosurgical spine services, have been made possible for outpatient postoperative spine care, that is, home care, wound care nurses, and same-day mid-level providers’ clinics. These types of initiatives have helped to lower spine surgery-related readmissions. However, there are relatively fewer resources available to cranial patients. Furthermore, not many rehabilitation facilities skilled nursing homes or outpatient nurses feel equipped to temporize even the smallest of cranial complications; therefore, these patients are readmitted more often for a higher level of support provided in the inpatient setting.
General postoperative complications and direct surgical complications accounted for a little over a third of readmissions (15.1 and 18.9%, respectively). General postoperative complications included readmission for diagnoses such as but not limited to urinary tract infections, pneumonia, pulmonary embolism, and/or deep venous thromboses. Diagnosis of CSF leaks, hardware misplacement, or shunt failures was considered to direct results of neurosurgical care. Unlike other studies of readmissions in neurological surgery,[
Somewhat surprising, 7-day readmissions related to postoperative pain (9.3%) and infection (9.7%) proved to have the lowest incidence among readmitted patients. However, subgroup analyses showed that a patient who underwent spine surgery was a significant proportion in each of the categories. As previous data in the literature have soon, this result is likely from a subset of patients who are narcotic dependent and have significant comorbid conditions which predispose them to surgical site infection, that is, obesity and diabetes mellitus. Furthermore, readmissions for planned elective surgeries and those which are unrelated to neurosurgical care (e.g., patient displeased with rehabilitation or skilled nursing facility) accounted for 13% and 18%, respectively. This information provides an opportunity for more insightful means for institutions to scrutinize such readmission into a separate category that does not get lumped into the cohort, for which hospitals may be penalized.
There are several limitations to this study. These results are a reflection of our hospital’s unique neurosurgical service line that may not compare directly to other hospitals, patient populations, and geographic locations. Our future goals are to increase the sample size and generalizability by collaborating with other large neurosurgical institutions for a multi-center database to increase the investigational rigor of the study.
CONCLUSION
The 7-day readmission rate for the UPMC-PUH neurosurgery service was 5%. Fifty-seven percent of all readmitted patients underwent a cranial intervention in comparison to 32% who had spine procedures. The majority of readmissions were related to direct perioperative complications. Therefore, focal efforts to decrease specific postoperative complications should translate into a reduction in 7- and subsequently 30- day unplanned readmissions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Wolff Center for Clinical Improvement at UPMC for assistance in data acquisition.
References
1. Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: Systematic review and meta-analysis. Neurosurg Focus. 2015. 39: E7
2. Elsamadicy AA, Sergesketter A, Adogwa O, Ongele M, Gottfried ON. Complications and 30-day readmission rates after craniotomy/craniectomy: A single institutional study of 243 consecutive patients. J Clin Neurosci. 2018. 47: 178-82
3. Hines A, Barrett M, Jiang J, Steiner CA.editors. Conditions with the Largest Number of Adult Hospital Readmissions by Payer. Rockville, MD: Agency for Healthcare Research and Quality; 2014. p.
4. Kalagara S, Eltorai AE, Durand WM, DePasse JM, Daniels AH. Machine learning modeling for predicting hospital readmission following lumbar laminectomy. J Neurosurg Spine. 2018. 30: 344-52
5. Moghavem N, Morrison D, Ratliff JK, Hernandez-Boussard T. Cranial neurosurgical 30-day readmissions by clinical indication. J Neurosurg. 2015. 123: 189-97
6. Rau J. New Round of Medicare Readmission Penalties Hits 2, 583 Hospitals. Available from: https://www.khn.org/news/hospital-readmission-penalties-medicare-2583-hospitals [Last accessed on 2019 Oct].
7. Schipmann S, Schwake M, Molina ES, Roeder N, Steudel WI, Warneke N. Quality indicators in cranial neurosurgery: Which are presently substantiated? A systematic review. World Neurosurg. 2017. 104: 104-12
8. Shah MN, Stoev IT, Sanford DE, Gao F, Santiago P, Jaques DP. Are readmission rates on a neurosurgical service indicators of quality of care?. J Neurosurg. 2013. 119: 1043-9
9. Strom JB, Kramer DB, Wang Y, Shen C, Wasfy JH, Landon BE. Short-term rehospitalization across the spectrum of age and insurance types in the United States. PLoS One. 2017. 12: e0180767
10. Taylor BE, Youngerman BE, Goldstein H, Kabat DH, Appelboom G, Gold WE. Causes and timing of unplanned early readmission after neurosurgery. Neurosurgery. 2016. 79: 356-69
11. Wilson MP, Jack AS, Nataraj A, Chow M. Thirty-day readmission rate as a surrogate marker for quality of care in neurosurgical patients: A single-center Canadian experience. J Neurosurg. 2018. 130: 1-7