- Department of Neurosurgery, Federal University of São Paulo,
- Department of Neurosurgery, Universidade Federal de São Paulo,
- Department of Neurosurgery, Unifesp, Napoleão de Barros,
- Department of Neurosurgery, Universidade Federal de São Paulo,
- Department of Neurosurgery, Sao Paulo Federal University, São Paulo, Brazil.
Correspondence Address:
Feres Eduardo Aparecido Chaddad Neto, Department of Neurosurgery, Federal University of São Paulo, São Paulo, Brazil.
DOI:10.25259/SNI_736_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: João Vitor Fernandes Lima1, Marcos Devanir Silva da Costa2, Bruno Loof de Amorim3, Jose Ernesto Chang Mulato3, Hugo Leonardo Doria Netto4, Jose Maria Campos Filho4, Feres Eduardo Aparecido Chaddad Neto5. Cerebral abscess secondary to embolization of arteriovenous malformation: A case report and literature review. 08-Nov-2021;12:553
How to cite this URL: João Vitor Fernandes Lima1, Marcos Devanir Silva da Costa2, Bruno Loof de Amorim3, Jose Ernesto Chang Mulato3, Hugo Leonardo Doria Netto4, Jose Maria Campos Filho4, Feres Eduardo Aparecido Chaddad Neto5. Cerebral abscess secondary to embolization of arteriovenous malformation: A case report and literature review. 08-Nov-2021;12:553. Available from: https://surgicalneurologyint.com/surgicalint-articles/11221/
Abstract
Background: Infectious complications of the central nervous system secondary to endovascular procedures have rarely been reported. However, the number of complications has grown exponentially owing to the popularization of these procedures. The success rate of these procedures varies with the pathology, the patient, and surgical performance. Although brain abscesses have been extensively reported, their presence after endovascular procedures has not been described in detail in the literature. We present a case of brain abscess induced by embolization of an arteriovenous malformation (AVM), discuss the main indications, techniques, procedural complications, and review the associated literature.
Case Description: A 13-year-old boy presented to us with a history of hemorrhagic stroke secondary to a cerebral AVM rupture. He underwent incomplete AVM resection (2014), with subsequent incomplete embolization (2017), and permanence of the endovenous catheter as a procedural complication. Physical examination revealed purulent exudate through the cervical surgical wound. We performed cervicotomy to remove the catheter but had no success in removing the intracranial material segment. The patient was subsequently diagnosed with a brain abscess (2018) and treated with antibiotics. Our team performed resection of the residual AVM, abscess, and the catheter-associated with the region.
Conclusion: The patient showed significant clinical improvement after surgical resection of the malformation. No residual lesions were observed in the imaging examinations. Further, we reviewed the literature to find other cases of similar complications and their association with the endovascular procedure. We did not find complications in patients younger than the one presented in this case. Factors such as incomplete embolisation increase the risk of unfavourable outcomes.
Keywords: Abscess, Arteriovenous malformation, Complication, Embolization, Infection
INTRODUCTION
Endovascular embolization of arteriovenous malformations (AVMs) was first described in the 1960s by Luessenhop and Spence, who injected methyl methacrylate pellets to occlude inflow vessels feeding in an AVM.[
The success rate in the treatment of the most diverse pathologies with embolization varies: AVMs (60%),[
Previous studies have addressed the complications related to endovascular procedures. Infection-related complications are generally rare but may contribute to the associated morbidity. With the popularization of the endovascular procedure, infection-related complications will likely become increasingly frequent. Complicated post-procedural infections causing cerebral abscesses have been reported in isolated case reports.[
MATERIALS AND METHODS
For the literature review, we searched on platforms like PubMed and Google Scholar for articles containing the following keywords: transvenous, embolization, AVMs, complication, endovascular, infection, and abscess. We considered all study designs, including both primary (case reports and case series) and secondary research (narrative and systematic reviews). The most relevant 577 articles were filtered, and the corresponding cases were included in the analysis to build our literature review table. Our study follows the Helsinki the principles of the declaration of Helsinki.
CASE REPORT
History and presentation
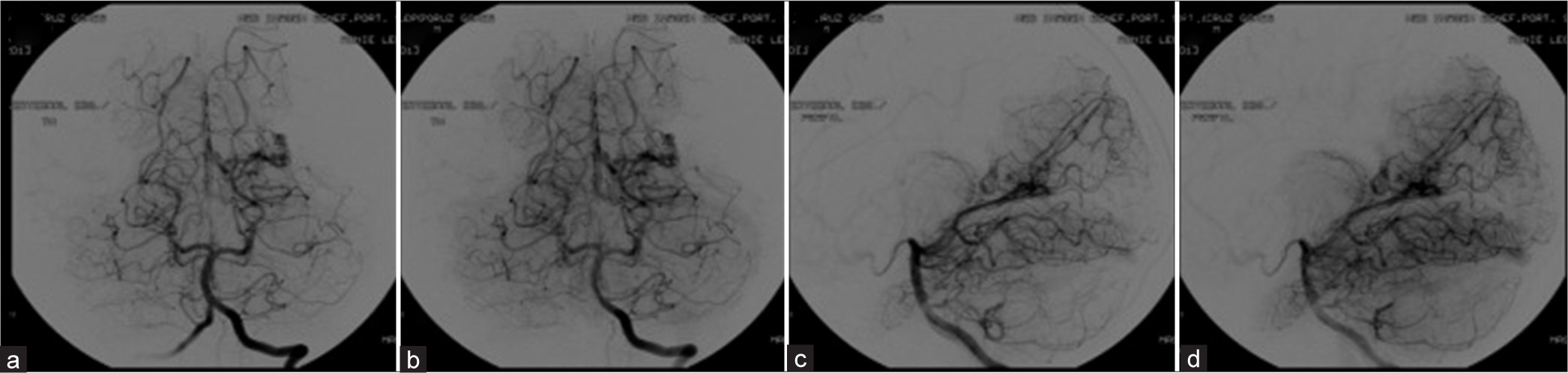
A 13-year-old boy, previously assisted by an external team, presented with a hemorrhagic stroke secondary to an AVM rupture in 2013. A 2013 angiography revealed a left occipital lobe AVM, fed by the calcarine and the posterior inferior temporal artery branches, with superficial venous drainage through the medial occipital vein into the posterior third of the superior sagittal sinus, and deep drainage through the occipital vein into the vein of Galen, thus classifying it as a Spetzler–Martin grade III AVM [
Figure 1:
Pre-surgical cerebral angiography of the vertebro-basilar circulation (2013) in anteroposterior (a and b) and lateral projections (c and d) showiing AVM of the posterior circulation supplied by branches of the left posterior cerebral artery in its P4 segment with deep venous drainage to the basal vein of Rosenthal.
The patient underwent partial resection of the malformation in 2014. We complemented the treatment with embolization in August 2017, with the intraluminal permanence of the endovenous catheter evolving as a complication after gluing to the vein. We performed cervicotomy to remove the catheter but could not remove the intracranial part. The patient was subsequently diagnosed with a brain abscess (2018) after a physical examination revealed purulent exudate through the cervical surgical wound. He presented neurologically with contralateral homonymous hemianopsia, without any other symptoms.
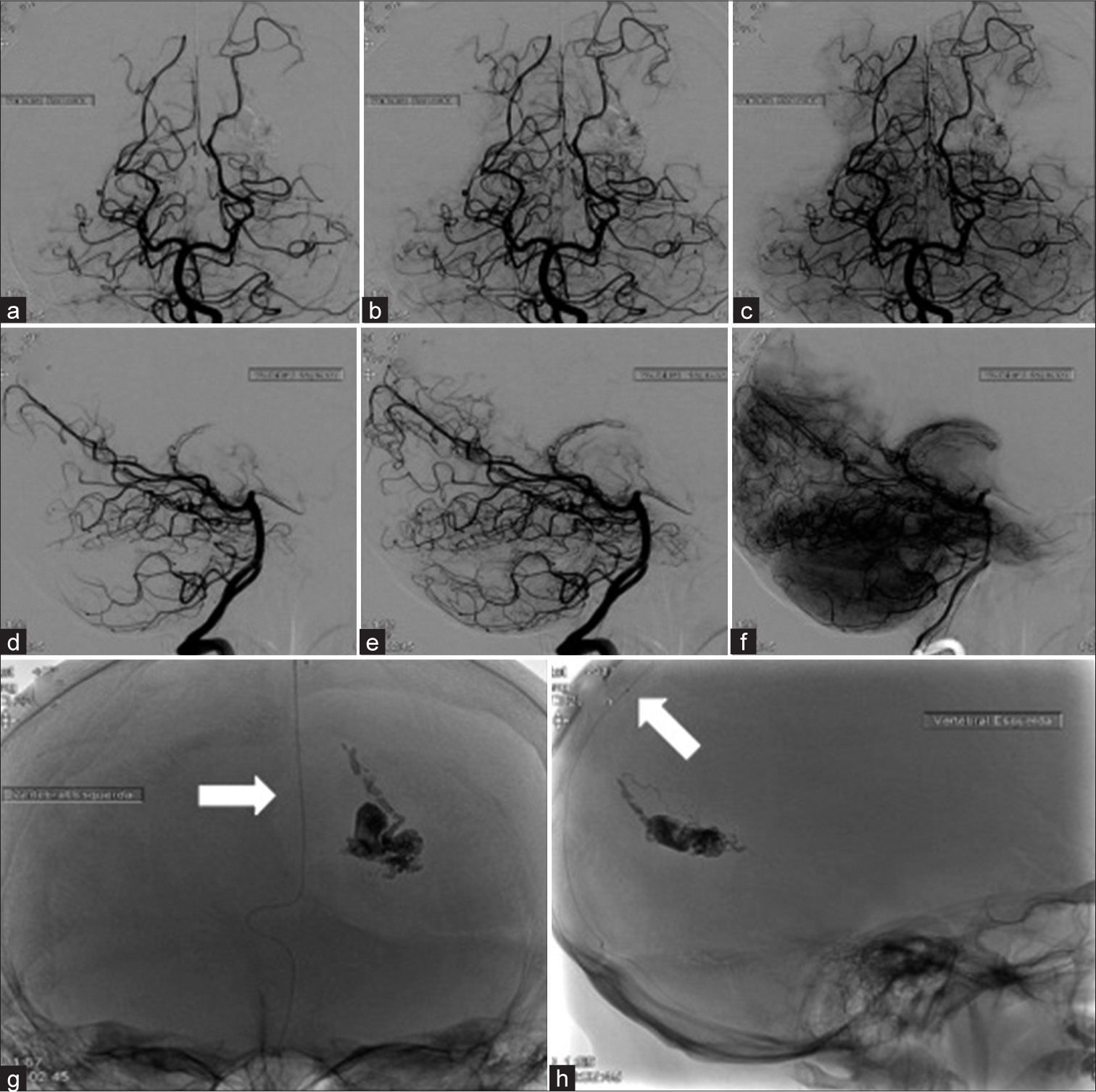
The patient was admitted to our hospital in February 2019. He was reinvestigated using cerebral angiography, which demonstrated residual AVM with the embolization material and the presence of an endovenous catheter in the posterior third of the superior sagittal sinus up to the right jugular vein [
Figure 2:
Cerebral angiography of the vertebro-basilar circulation prior to 2019 surgery in anteroposterior (a-c) and lateral projections (d-f) In early to late angiographic phases respectively where residual AVM and intraluminal embolization material are observed. Anteroposterior (g) and lateral projections (h) showing the route of the intraluminal catheter from the right jugular foramen to the posterior third of the superior sagittal sinus is observed (white arrow).
Thereafter, he underwent microsurgery, with reopening of planes, complete resection of the AVM transulcal route, removal of residual granuloma.
The catheter remained in the posterior third of the superior sagittal sinus extending up to the cervical region of the right jugular vein. Antibiotics were administered (linezolid and ceftriaxone) in the postoperative period and the patient started to show a good response, without new febrile episodes.
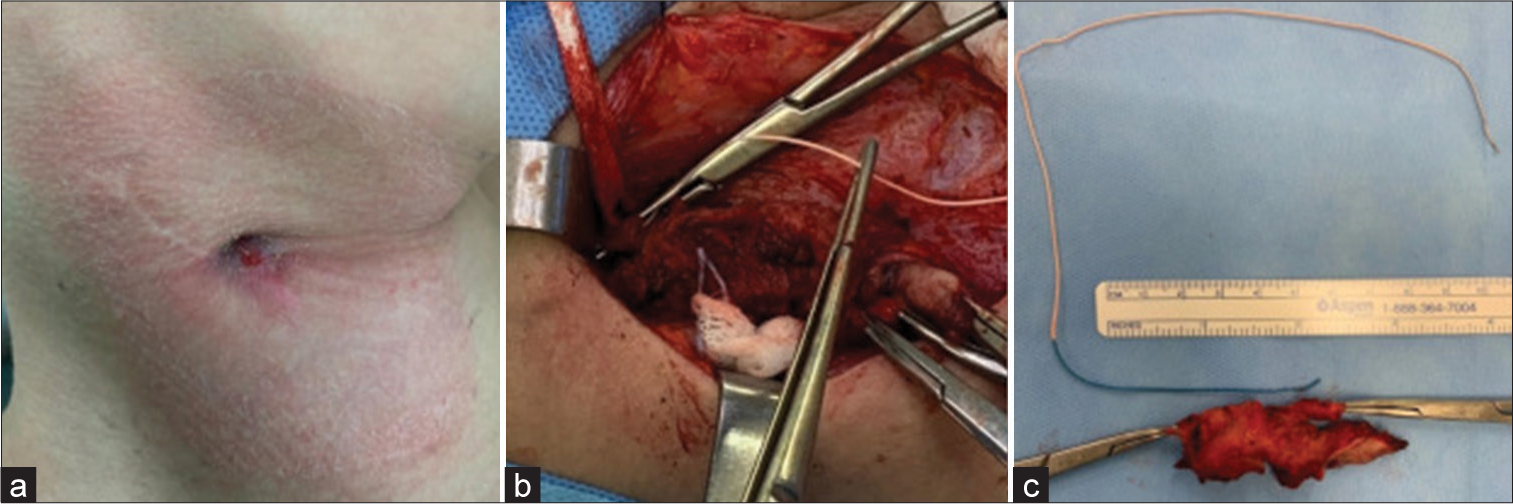
In February 2020, the patient presented with thrombosis of the right jugular vein and purulent exudate through the cervical wound. We started anticoagulation therapy with warfarin and performed a right cervicotomy. We opened the jugular vein to remove the catheter and subsequently ligated the vein [
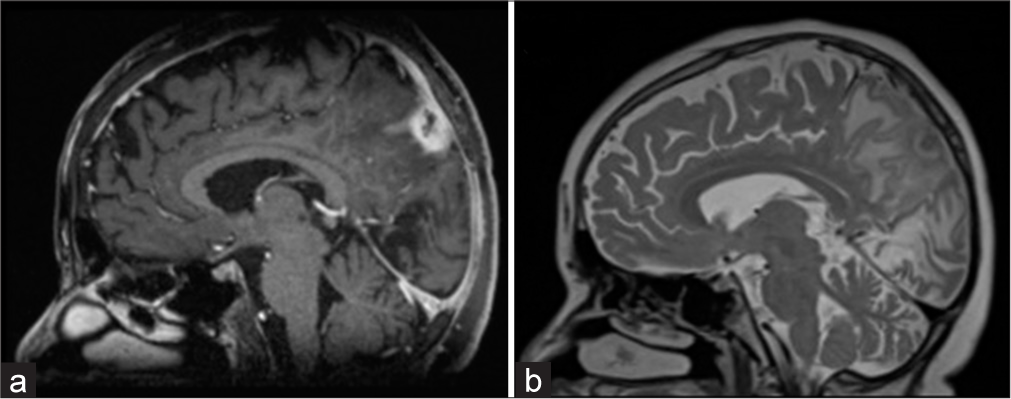
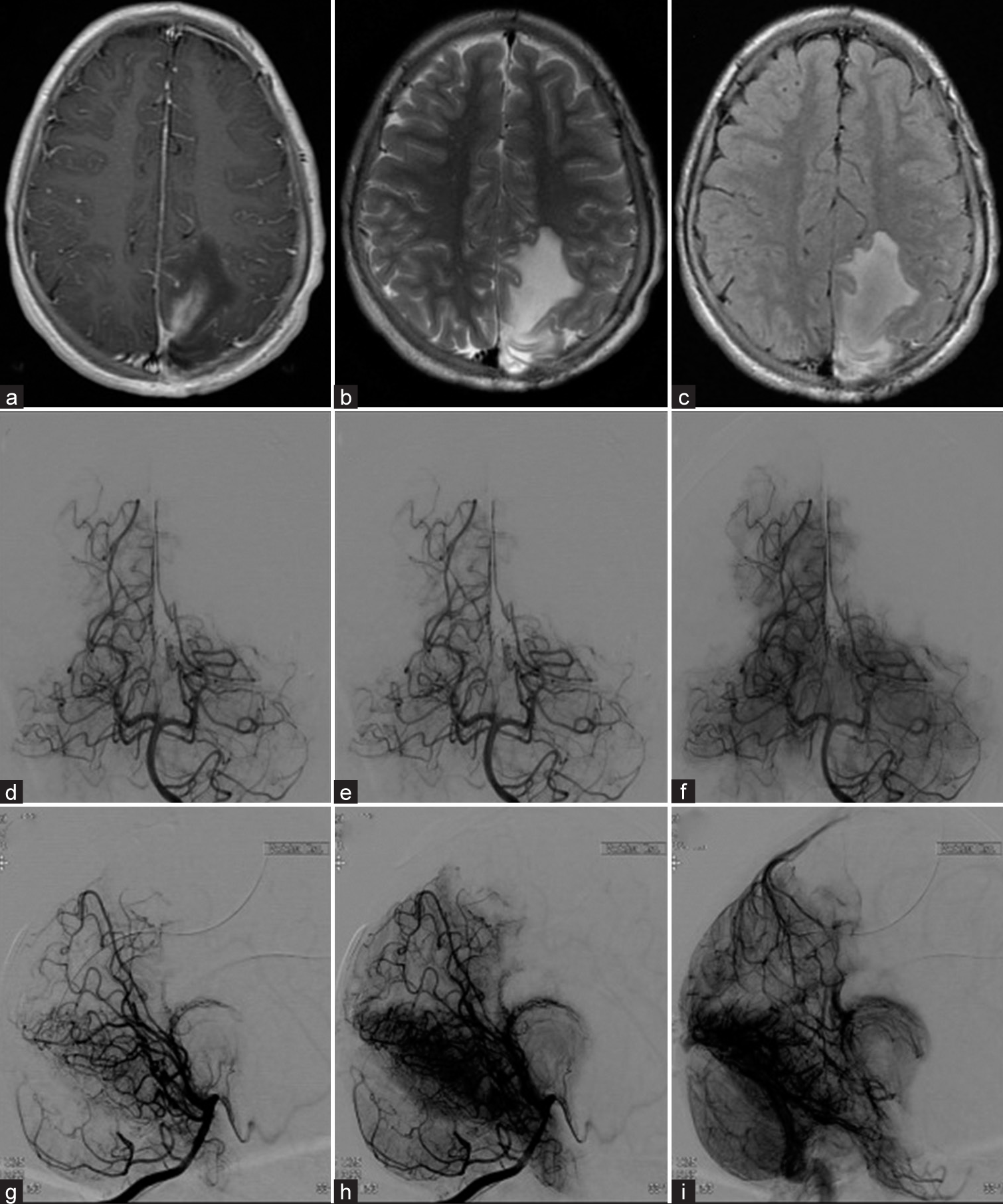
The patient is currently asymptomatic, without neurological deficits or new febrile episodes. Postoperative MRI scans of the brain showed expected changes without the presence of residual lesions, including edema in the surgical location. Cerebral angiography revealed the absence of residual AVMs [
Figure 5:
Post-surgical control magnetic resonance imaging in axial sections, weighted in T1 with gadolinium (a), T2 (b) and FLAIR (c), observing postsurgical changes without residual lesion. Post-surgical control cerebral angiography of the vertebro-basilar circulation in anteroposterior (d-f) and lateral projections (g-i) in early to late angiographic phases respectively where without evidence of residual AVM is observed.
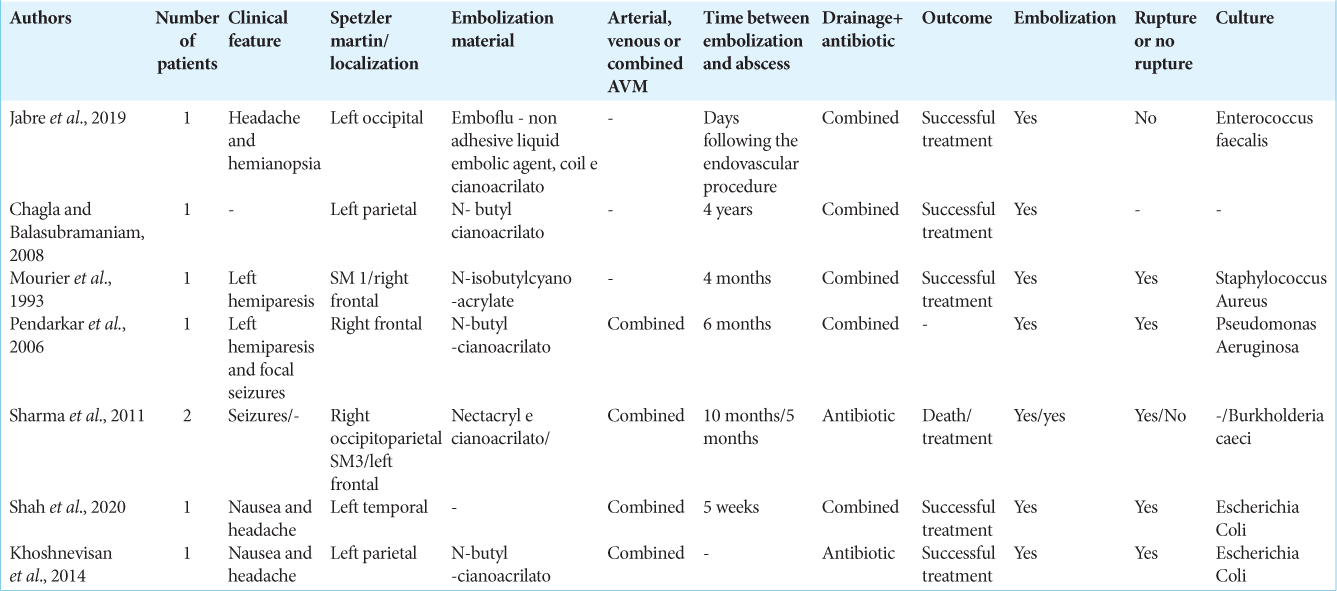
Literature review
[
DISCUSSION
According to the literature reviewed by us, our reported case was the youngest patient who presented with a post-embolization brain abscess (13-year-old). It was, therefore, important to document this case even though abscesses resulting from endovascular procedures are a rare occurrence.
At present, cerebral AVM management requires a multidisciplinary team of experts in vascular neurosurgery, interventionism, and radiotherapy in order to provide the best therapeutic option to the patient based on the morphological characteristics of the AVM. Endovascular embolization plays an important role in adjuvant presurgical therapy.[
Endovascular management targets of AVM focus on “weak points,” flow-related aneurysms, and high-flow fistulas, with the aim of reducing the lesion size and normalizing the blood flow patterns in the surrounding parenchyma.[
Brain abscesses are a well-reported complication after cranial surgeries. However, reports on abscesses developing after endovascular procedures to treat cerebral vascular malformations are sporadic, comprising isolated case reports.[
The hypothesized risks of infectious complications secondary to the endovascular procedures are inadequate handling and in-hospital contamination of medical devices. The most frequently associated agents are Staphylococcus aureus and Pseudomonas aeruginosa, skin-related microorganisms, and in-hospital colonization, respectively.
The pathways for bacterial dissemination proposed in delayed brain abscess associated with endovascular procedures are the percutaneous colonization and hematogenous spreading of systemic infection (bacteraemia, urinary tract infection).[
In our case, we observed in the patient’s history that he was exposed to several risk factors, such as incomplete embolization, surgical manipulation post- embolization, and the intraluminal presence of the embolisation catheter. The history of infection, the cervical manipulation, and an ankle abscess that could have caused the hematogenous migration of pathogens was also taken into account. Cumulatively, all these factors caused the formation of a brain abscess months after all these procedures and could be treated with antibiotic therapy. However, a new surgical intervention was necessary for the complete resection of the AVM and the granuloma. A second intervention was also necessary to remove the intravenous cerebral catheter. The pathology was resolved with adequate evolution. Endovenous antibiotics complemented with the drainage of the abscess with a burr hole led to the reduction of the lesions two months after the initiation of treatment.[
In this case, antimicrobial treatment was necessary with subsequent resection of the AVM, the granuloma, and the catheter-associated with it, finally obtaining good postsurgical results.
CONCLUSION
We conclude that endovascular procedures have several rare complications that are becoming more frequent due to the popularization of the technique. Factors such as incomplete embolization and surgical manipulation increase the risk of unfavorable outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bruno CA, Meyers PM. Endovascular management of arteriovenous malformations of the brain. Interv Neurol. 2013. 1: 109-23
2. Cossu G, Daniel RT, Messerer M. Cerebral abscess after neurovascular embolization: Own experience and review of the literature. Acta Neurochirurgica (Wien). 2017. 159: 583-91
3. Gemmete JJ, Ansari SA, Gandhi DM. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol. 2009. 29: 62-71
4. Khoshnevisan A, Ghorbani A, Allahabadi NS, Farzaneh F, Abdollahzadeh S, Soleymani S. Cerebral abscess complicating embolization of an arteriovenous malformation: Case report and review of literature. Iran J Neurol. 2014. 13: 181-4
5. Mendes GA, Kalani MY, Iosif C, Lucena AF, Carvalho R, Saleme S. Transvenous curative embolization of cerebral arteriovenous malformations: A prospective cohort study. Neurosurgery. 2018. 83: 957-64
6. Morgan MK, Zurin AA, Harrington T, Little N. Changing role for preoperative embolisation in the management of arteriovenous malformations of the brain. J Clin Neurosci. 2000. 7: 527-30
7. Richling B, Killer M, Al-Schameri AR, Ritter L, Agic R, Krenn M. Therapy of brain arteriovenous malformations: Multimodality treatment from a balanced standpoint. Neurosurgery. 2011. 59: S148-57
8. Sharma A, Jagetia A, Loomba P, Singh D, Tandon M. Delayed brain abscess after embolization of arterio-venous malformation: Report of two cases and review of literature. Neurol India. 2011. 59: 620-3