- Department of Neurosurgery, Goethe-University Hospital, Frankfurt am Main, Germany
- Edinger- Institut of Neuropathology, Goethe-University Hospital, Frankfurt am Main, Germany
Correspondence Address:
Nina Brawanski
Department of Neurosurgery, Goethe-University Hospital, Frankfurt am Main, Germany
DOI:10.4103/2152-7806.193924
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nina Brawanski, Peter Baumgarten, Jürgen Konczalla, Volker Seifert, Christian Senft. Cerebral foreign body granuloma in brain triggering generalized seizures without obvious craniocerebral injury: A case report and review of the literature. 11-Nov-2016;7:
How to cite this URL: Nina Brawanski, Peter Baumgarten, Jürgen Konczalla, Volker Seifert, Christian Senft. Cerebral foreign body granuloma in brain triggering generalized seizures without obvious craniocerebral injury: A case report and review of the literature. 11-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/cerebral-foreign-body-granuloma-brain-triggering-generalized-seizures-without-obvious-craniocerebral-injury-case-report-review-literature/
Abstract
Background:Intracerebral foreign body granuloma is rarely reported. We present the case of a male patient with a cerebral foreign body granuloma.
Case Description:Initial admission of a 67-year-old male patient was after an aphasia followed by secondary generalized seizures. Cranial computed tomography (CCT) showed a metal-dense, wedge-shaped foreign body in the range of the frontal sinus on the left side, breaking through the frontal sinus, and creating a connection to the frontal cerebral lobe. The patient did not report previous trauma or accident. A concomitant inflammatory response could not be excluded in CCT imaging. In clinical examination, the patient showed no sensorimotor deficit. Operative resection and dural reconstruction was performed. Several tiny, metal-like foreign-body fragments and one stone-like body could be detected and removed. Histopathological examination showed an intracerebral granuloma with areas of acute granulocytic inflammatory reaction.
Conclusion:Cerebral foreign body granuloma is a rare entity without initially provoking clinical symptoms, and causing clinical symptoms even years after the initial event. In most reported cases, wooden or metallic bodies are reported. In addition, hemostatic materials and non-resorbable cotton sheets can cause intracerebral granuloma. There is a high risk of infection with a high mortality rate in case of an existent intracranial abscess. In case of first presentation of seizures, a foreign body should be kept in mind if a traumatic injury cannot be reported. Therefore, possible foreign bodies provoking clinical symptoms such as seizures should always be radiologically excluded, and if present and operatively accessible, removal should be done as soon as possible.
Keywords: Cerebral granuloma, foreign body, seizures
INTRODUCTION
Foreign body granuloma in brain is rarely reported. In a PubMed search from 1974 to 2015, only 43 cases were observed (cerebral cholesterol granulomas were excluded in the search). New onset seizures are considered to be typical manifestations, along with infections such as meningitis or cerebritis.[
We present the case of a 67-year-old male patient suffering from late-onset seizures caused by a frontal foreign body granuloma due to a foreign body breaking through the frontal sinus on the left side without obvious craniocerebral injury.
CASE PRESENTATION
Patient data
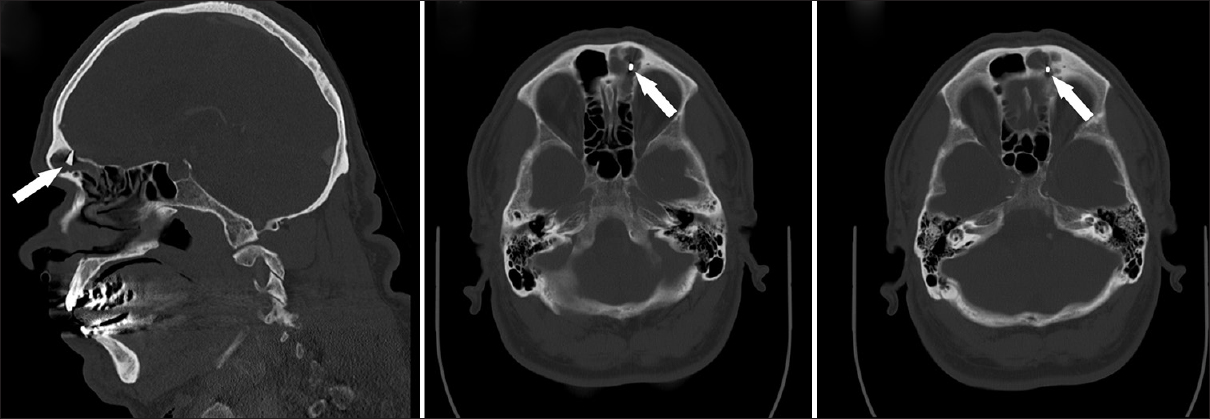
We present the case of a 67-year-old male patient. Initially, he was admitted to the Department of Neurology because of secondary generalized seizures after presenting with aphasia. An anticonvulsive medication with levetiracetam was initiated. Blood tests did not show increased inflammatory parameters, merely a mild leukocytosis. In initial cranial imaging using cranial computed tomography (CCT) with CT angiography a metal-dense, wedge-shaped foreign body in the range of frontal sinus on the left side was detected, which braked through the frontal sinus and created a connection to the frontal cerebral lobe. There was no defect of the skull. In addition, the left frontal lobe showed a hypodense area [
The patient was alert and reported that there had been no traumatic injuries. However, he could vaguely remember being told as a boy that there was “something” in his nose. In a cMRI (approximately 20 years ago), the foreign body arguably could be observed, however, no inspection was conducted at the time. In clinical examination the patient showed no focal deficit. Further seizures did not occur during his stay in the hospital under anticonvulsive therapy.
Because of the assumed infection (a concomitant intracerebral abscess could not be excluded) and the existing connection to the frontal cerebral lobe, surgery was recommended. Thereby, removal of the foreign body and the frontobasal covering was planned. In addition, inspection of the left frontal lobe, smear tests, and eventual clearing of the suspected intracranial abscess was planned.
Operation
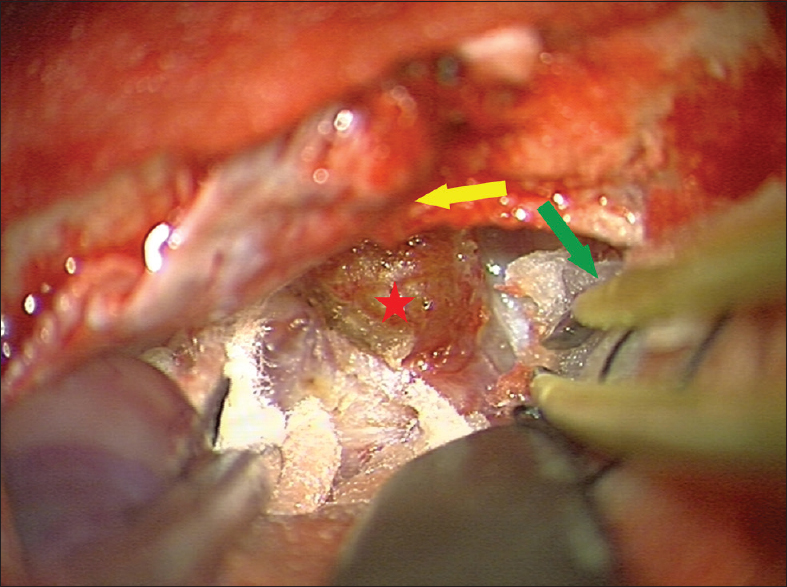
We chose a small left frontobasal, paramedian (3 × 3 cm craniotomy) access path across a bifrontal cut. Thereby, the frontal galea periost was conserved for the later planned frontobasal covering. After retracting the left frontal lobe, a frontobasal lesion (1 × 1 cm) with cerebral infiltration appeared [
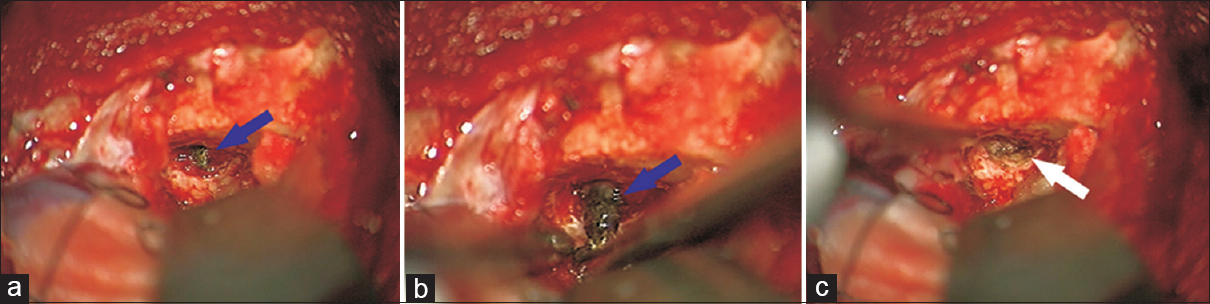
Figure 3
(a, b) After resection of granuloma, a metal-dense, wedge-shaped foreign body in the range of the frontal sinus on the left side can be seen, breaking through the frontal sinus and creating a connection to the frontal cerebral lobe, can be seen. After resection of the foreign body, direct view to the frontal sinus with a chronic inflammatory reaction is seen (c)
Clinical course
Postoperatively, the patient fast recovered from the operation. Intravenous antibiotic therapy was continued for at least 3 weeks. Microbiological examination of the intraoperatively obtained material from the frontal sinus resulted in the detection of Klebsiella pneumoniae. Antibiotic therapy was adapted corresponding to antibiotic recommendation. A systemic inflammatory response did not occur at any time during the patient's stay in our hospital. Also, no further seizures occurred. There were no signs of a postoperative frontobasal fistula. The patient was transferred to a rehabilitation center.
Histopathological findings
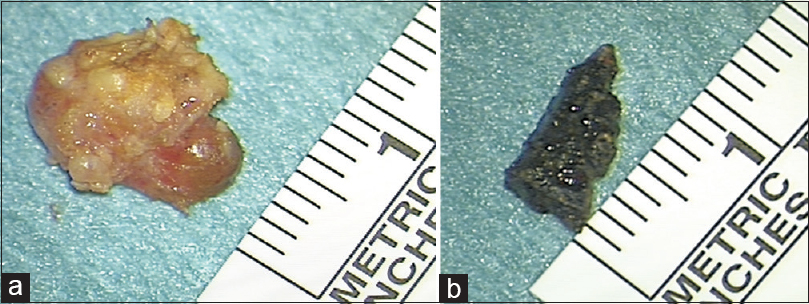
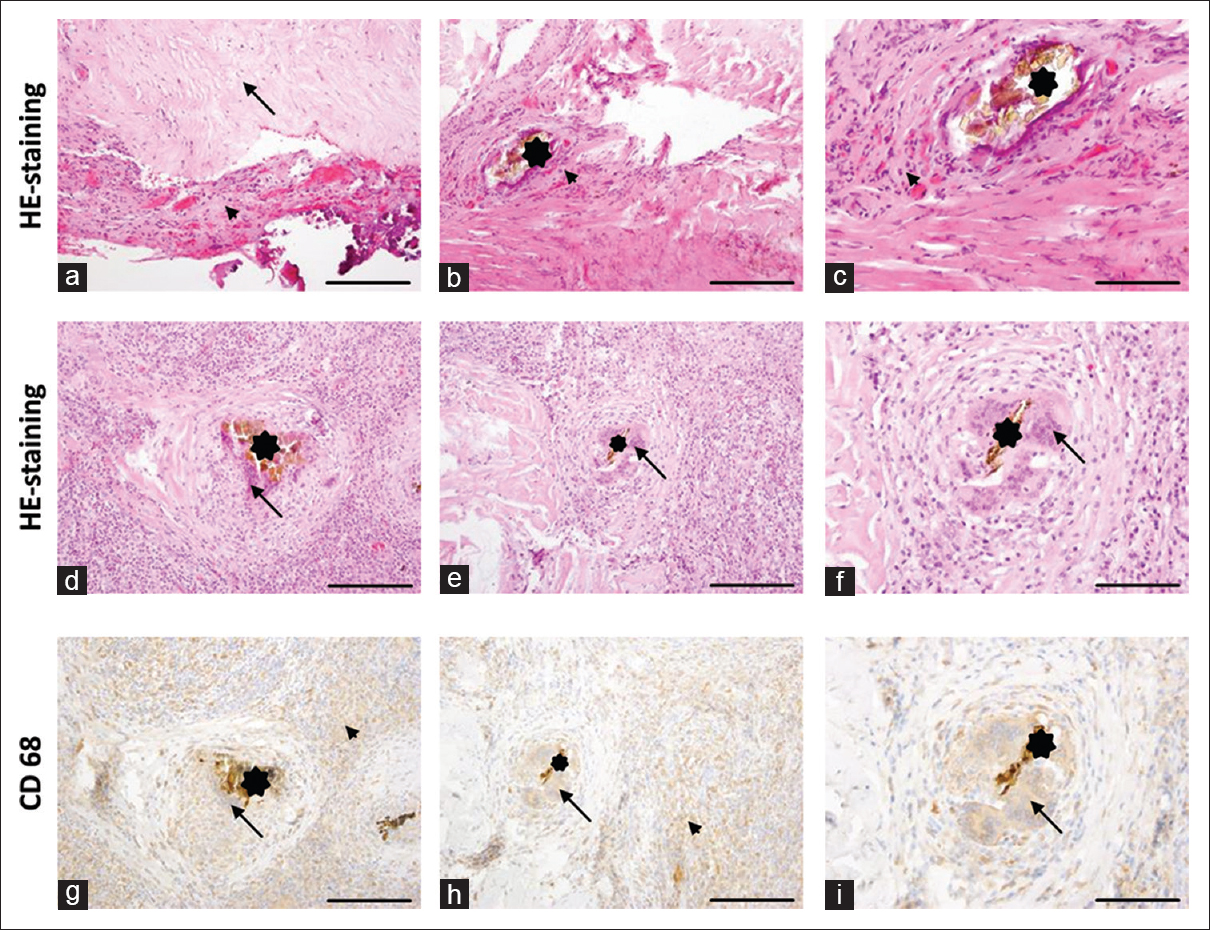
Histopathological examination showed intracerebral granuloma presenting parts of an acute granulocytic inflammatory reaction. Examination of the removed frontobasal dura showed an inflammation reaction with the detection of leucocytes. The material resected from the left frontal sinus showed connective tissue and a necrotic cell detritus with a lymphatic, plasma cellular, and monozytic infiltration [Figure
Figure 5
Histopathological findings showing hematoxylin and eosin (H and E) staining of representative areas of the dura specimens loose (a, arrow) and proliferating connecting tissue (a-c; arrow head), with only very few fragments of the alleged foreign particle (b, c; asterisk) surrounded by connecting tissue proliferations with higher vascularization (b, c; arrow head) and focal mineralization (a). (d-f) H and E staining of the representative areas of the foreign body granuloma with giant cells (arrows) surrounding fragments of the foreign body (asterisk). (g-j) Immunohistochemical staining against CD68 showing positivity of the giant cells (g-j; arrows) and surrounding macrophages (arrow heads). Similar immunohistochemistry protocols for different antibodies have been previously published.[
DISCUSSION
Foreign body granuloma is a rare entity. In a PubMed search, a total of 43 cases from 1974 to 2015 were noted. The most common causes of symptomatic epilepsy are brain infections and traumatic brain injuries.[
In most reported cases, wooden foreign bodies (such as chopsticks or pencils)[
Miller et al.[
Considering a reported mortality rate due to intracranial abscess caused by intracerebral foreign bodies in 57% of the affected patients, it is important to keep this rare entity in mind, especially since mortality rates can be reduced by a fast surgical therapy.
Furthermore, in times of war and violent conflicts, as well as a growing number of refugee influx in numerous parts of the world, the number of patients suffering from intracerebral granuloma caused by craniocerebral injuries may possibly increase.
CONCLUSION
Intracerebral foreign body granuloma is rarely reported. In case of seizures presenting for the first time, this possible cause should always be kept in mind, although without remembering any traumatic brain injury in anamnesis. Therefore, in cranial imaging, possible foreign bodies provoking clinical symptoms should always be excluded, and in case of a detected intracranial foreign body, removal should be done as soon as possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abbassioun K, Ameli NO, Morshed AA. Intracranial sewing needles: Review of 13 cases. J Neurol Neurosurg Psychiatry. 1979. 42: 1046-9
2. Annegers JF, Hauser WA, Coan SP, Rocca RW. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998. 338: 20-4
3. Baumgarten P, Blank AE, Franz K, Hattingen E, Dunst M, Zeiner P. Differential expression of vascular endothelial growth factor A, its receptors VEGFR-1, -2, and -3 and co-receptors neuropilin-1 and -2 does not predict bevacizumab response in human astrocytomas. Neurooncology. 2016. 18: 173-83
4. Chunhua Q, Qun W. A late-onset seizure due to a retained intracranial foreign body--pencil lead: A case report and review. J Craniofac Surg. 2014. 25: e109-10
5. Miller CF, Brodkey JS, Colombi BJ. The danger of intracranial wood. Surg Neurol. 1977. 7: 95-103
6. Nakayama T, Shimazaki K, Ono J, Ohsato K, Yamaura A. Intracranial foreign body granuloma caused by fine cotton fibers: A case report. No Shinkei Geka. 1994. 22: 1081-4
7. Nishio Y, Hayashi N, Hamada H, Hirashima Y, Endo S. A case of delayed brain abscess due to a retained intracranial wooden foreign body: A case report and review of the last 20 years. Acta Neurochir. 2004. 146: 847-50
8. Saeidiborojeni HR, Fakheri T, Iizadi B. Intracranial foreign body granuloma simulating brain tumor: A case report. J Res Med Sci. 2011. 16: 358-60
9. Ribalta T, McCutcheon IE, Neto AG, Gupta D, Kumar AJ, Biddle DA. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Arch Pathol Lab Med. 2004. 128: 749-58