- Department of Neurosurgery, Sir Sunderlal Hospital, IMS, BHU, Varanasi, Uttar Pradesh, India
- Department Clinical Microbiology, DLW, Varanasi, Uttar Pradesh, India
Correspondence Address:
Sharad Pandey
Department of Neurosurgery, Sir Sunderlal Hospital, IMS, BHU, Varanasi, Uttar Pradesh, India
DOI:10.4103/2152-7806.163177
Copyright: © 2015 Pandey S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Pandey S, Pandey D, Shende N, Sahu A, Sharma V. Cerebral intraventricular echinococcosis in an adult. Surg Neurol Int 18-Aug-2015;6:138
How to cite this URL: Pandey S, Pandey D, Shende N, Sahu A, Sharma V. Cerebral intraventricular echinococcosis in an adult. Surg Neurol Int 18-Aug-2015;6:138. Available from: http://surgicalneurologyint.com/surgicalint_articles/cerebral-intraventricular-echinococcosis-in-an-adult/
Abstract
Background:Echinococcosis in humans occurs as a result of infection by the larval stages of taeniid cestodes of the genus echinococcus. Intracranial hydatid cysts usually develop at an intraparenchymal site. Hydatid cyst within the cerebral ventricle is quite unusual.
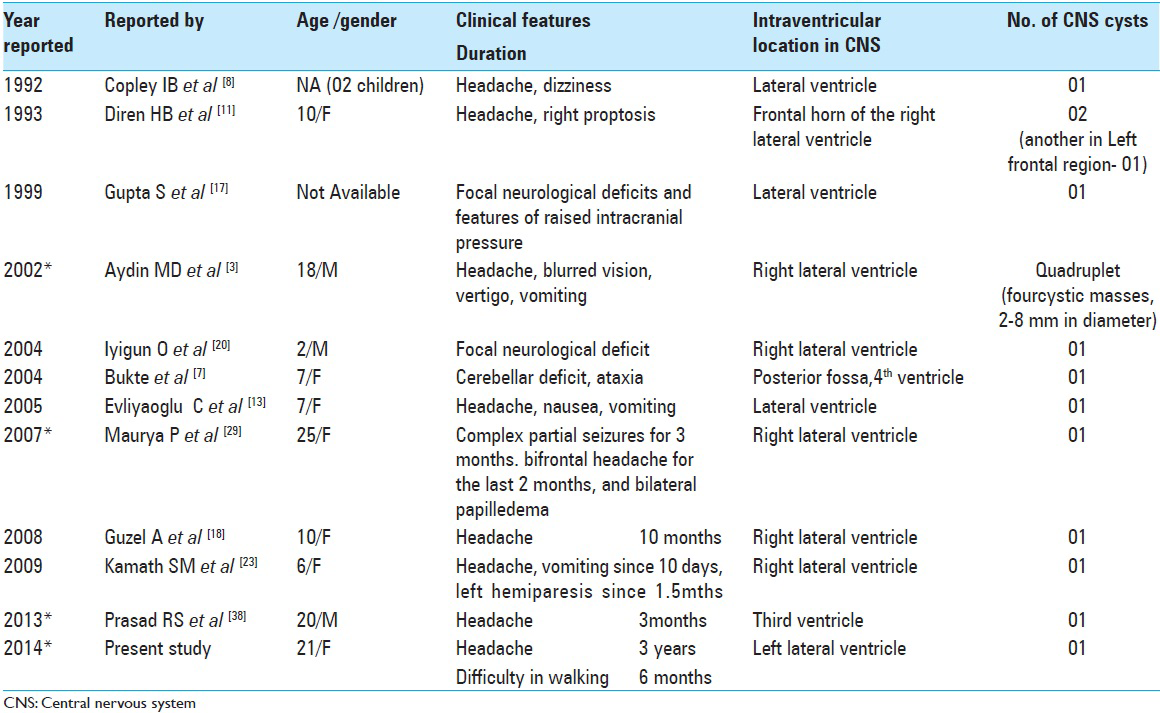
Methods:We reviewed the literature on adult intraventricular hydatid cyst and found case reports mainly in children with an only handful of cases in adults. We reported a rare case of cerebral intraventricular (left lateral ventricle) hydatid cyst in a 21-year-old adult female.
Results:Although cerebral hydatid cysts are most commonly seen in children and young adults cerebral intraventricular hydatid cyst are comparatively rarer in adults.
Conclusion:The possibility of infection with Echinococcus granulosus should be included in the differential diagnosis of raised intracranial hypertension in patients from endemic areas.
Keywords: Adult, cerebral intraventricular hydatid cyst, children, Echinococcosis
INTRODUCTION
Echinococcosis or hydatid disease, an endemic zoonotic disease, occurs as a result of infection by the larval stages of taeniid cestodes of the genus echinococcus. The two most commonly associated with human disease are Echinococcus granulosus whose cyst has limiting membrane and Echinococcus multilocularis (alveolar) which are less common but more serious and is almost always fatal. Several studies have shown that these diseases are an increasing public health concern and that they can be regarded as emerging or re-emerging diseases.[
CASE REPORT
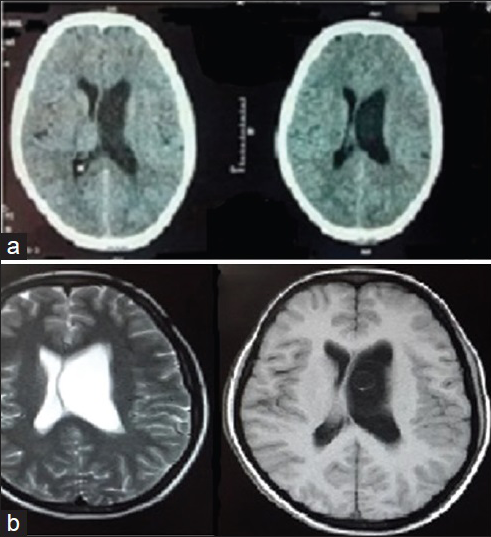
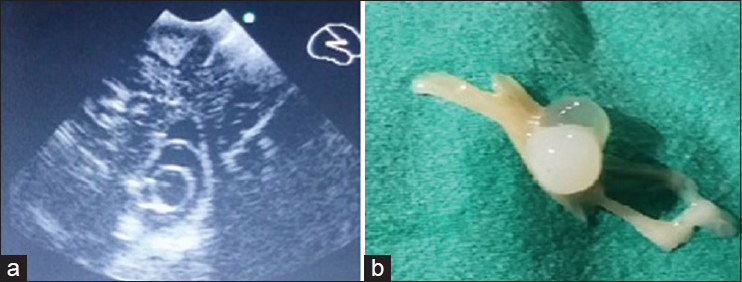
Twenty-one-year-old adult female with rural background presented in the OPD with chief complaints of headache since 3 years and difficulty in walking since 6 months. Physical examination was unremarkable. A neurologic examination revealed bilateral papilledema. The hematological investigation was within normal limits. No abnormality was found in X-ray chest, echocardiography, ultrasonography (USG) abdomen, and pelvis. Computed tomography (CT) scan of brain revealed mild asymmetrical dilatation of left ventricle with normal size right lateral, third and fourth ventricles without periventricular edematous changes suggesting possibility of outlet obstruction of lateral ventricle [
DISCUSSION AND REVIEW OF LITERATURE
Echinococcosis is also known as hydatidosis or hydatid disease. Six species have been recognized, but four are of public health concern: E. granulosus (causes cystic echinococcosis), E. multilocularis (causes alveolar echinococcosis), and Echinococcus vogeli and Echinococcus oligarthrus (which cause polycystic echinococcosis).[
Echinococcosis is a zoonosis in which the definitive host is a carnivore that harbors the adult tapeworm in the small intestine.[
The greatest prevalence of cystic echinococcosis in human and animal hosts is found in countries of the temperate zones including southern South America, the entire Mediterranean littoral, southern and central parts of the former Soviet Union, Central Asia, China, Australia, and parts of Africa.[
Hydatid is a Greek word meaning “a drop of water.” Hydatid cyst commonly occurs in the liver (55–70%), lung (18–30%), followed by the kidneys muscles, spleen, soft tissues, brain, and bone.[
Hydatid cysts constitute 3–4% of all intracranial space occupying lesions.[
The most common location in CNS infection is the hemispheric parenchyma, in the perfusion territory of the middle cerebral artery, especially in the parietal lobe.[
The cerebral hydatid cysts are usually slow growing; the growth rate has been variably reported between 1.5 and 10 cm/year.[
Clinically patients present with nonspecific signs and symptoms, most common ones being a headache, papilledema, vomiting, and symptoms of raised intracranial pressure can be seen.[
Cerebral hydatid cysts are most commonly seen in children and young adults.[
Among the laboratory investigations the immunoblot test, where available is the test of choice (98% specific and 91% sensitive). The “arc 5” antigen is present in E. granulosus hydatid fluid and can be identified easily as it shows a well-defined immunoelectrophoretic pattern. Arc 5 test is also diagnostic except for cross reactions with Taenia solium cysticercosis infection. Several other tests enzyme-linked-immunosorbent-assay, indirect hemagglutination, immunofluorescence are useful, but both false negative and false positive results are common.[
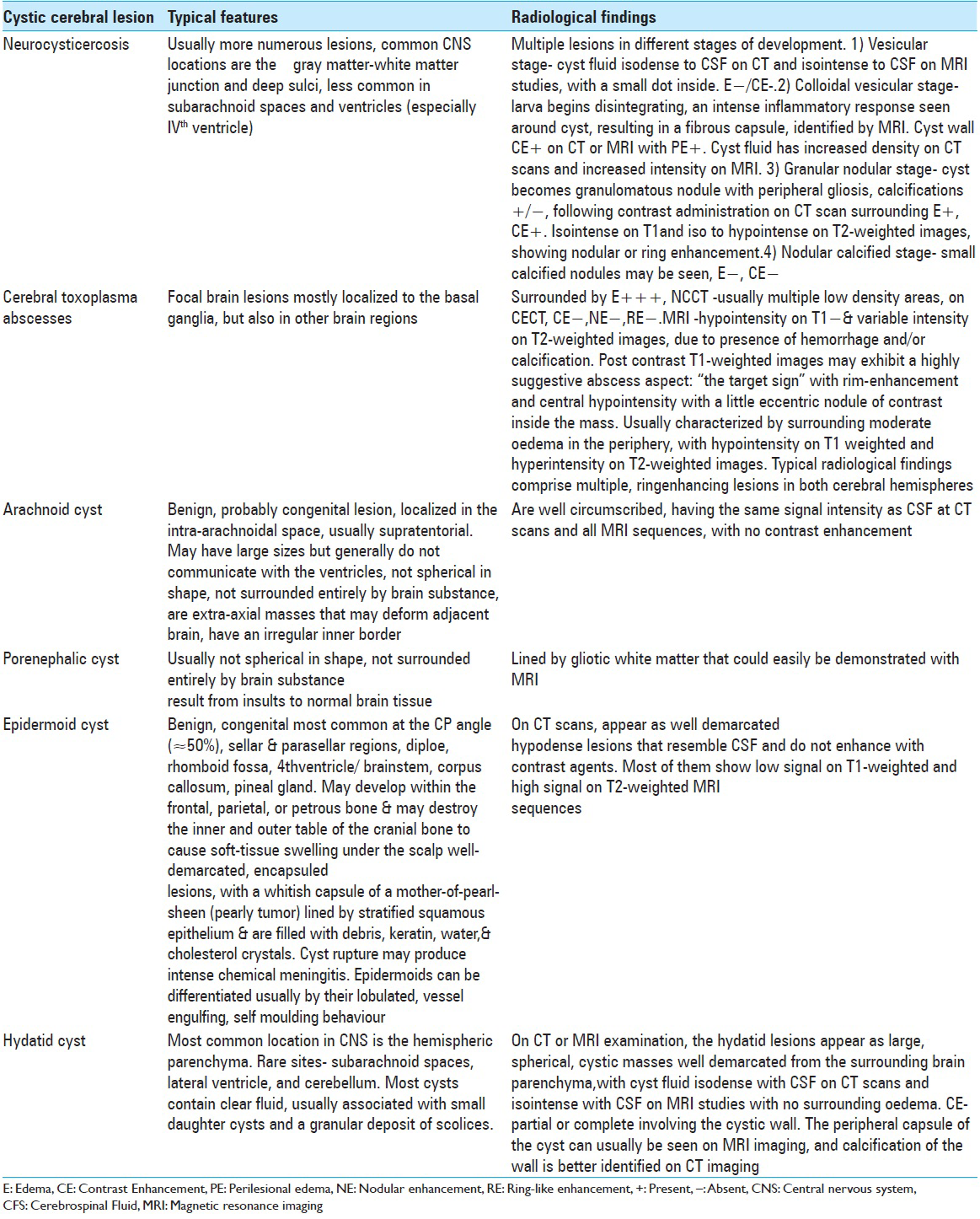
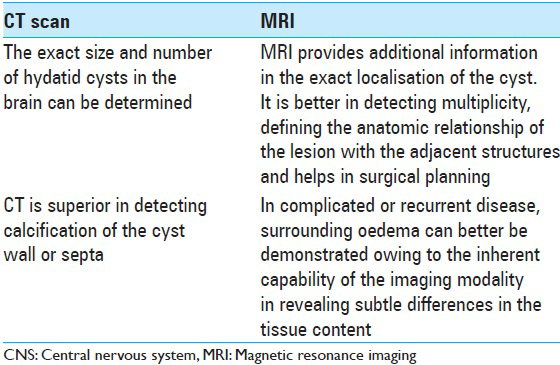
Imaging studies such as CT scan and MRI are necessary for preoperative diagnosis.[
Both CT and MRI demonstrate a spherical, well-defined, smooth, thin-walled, homogeneous cystic lesion with a fluid density similar to the cerebrospinal fluid (CSF), with or without septations or calcification.[
In cerebral cystic echinococcosis, CT and MRI findings are more typical than in cerebral alveolar echinococcosis. On CT and MRI, cerebral alveolar echinococcosis lesion appears as a solid, semisolid, or multilocular cystic mass with definite margins. Calcification and surrounding edema are common. Contrast enhancement occurs within the region of inflammatory reaction around the cysts.[
Another, one of the recent modalities is MRS. It uses 1H signals to determine the relative concentrations of target brain metabolites. Few MRS studies are available to give comprehensive information on cerebral echinococcosis. Kohli et al. performed in vivo and in vitro studies in a patient of intracranial hydatid cyst. Besides lactate, alanine and acetate, a large resonance for pyruvate was observed. MRS pattern appeared different from the other cystic lesions of the brain, and they suggested MRS as an adjunct to imaging in the differential diagnosis of intracranial hydatid. The role of MRS in monitoring drug therapy was also highlighted.[
Other investigations such as USG whole abdomen and pelvis, echocardiography, X-ray chest were unremarkable. These investigations are necessary to differentiate primary and secondary hydatid cysts. Primary intracranial hydatid infection is caused by embryos passing hepatic and pulmonary barriers. These are the most common types and are solitary. Secondary cysts are usually multiple which may follow embolization of ruptured cardiac cyst or spontaneous, traumatic and surgical rupture of a primary cyst in other organs.[
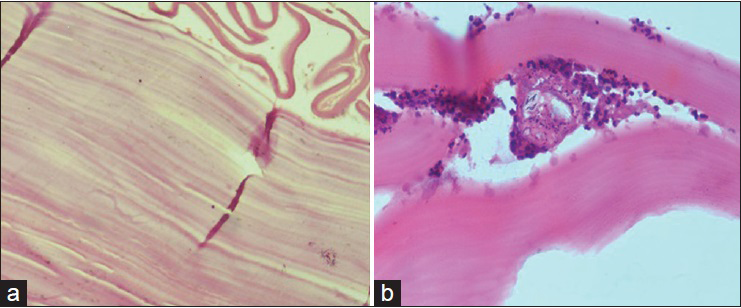
Histopathology helps in confirming the diagnosis. Hydatid cyst (cystic echinococcosis) consists of three layers:
Endocyst – in which is the inner germinal layer. Scolices, brood capsules, and daughter cysts originate from this layer by endo-proliferation or internal budding. To the contrary, a cyst of alveolar echinococcosis proliferates by external budding of the germinal membrane and progressively infiltrates the surrounding tissue Ectocyst - is the outer laminated layer Pericyst - signifies host reaction to the cyst. It is a fibrous capsule, which contains blood vessels that provide nutrients for the parasite.
Rapid decompression caused by evacuation of a large cyst may result in disturbances in autoregulatory mechanisms such as sudden decrease in pressure followed by cerebral edema, hyperpyrexia, cardiorespiratory failure, subdural collection, and the development of a porencephalic cyst which needs to be watched in postoperative period.[
Medical management involves the use of protoscolicidal agents such as praziquantel, albendazole. Praziquantel does not pass through the hydatid cyst wall, but high levels are seen in the CSF. As it has a powerful, lethal action on free scolices, it may be used in the event of spillage of the cyst fluids. Although protoscolicidal agents do not penetrate large hydatid cysts in sufficient quantity, highly soluble albendazole can used over a prolonged period for the treatment of small multiple cysts in inaccessible sites. A combination of praziquantel and albendazole is more effective than either drug used alone.[
CONCLUSION
Cerebral hydatid cysts although rare, can prove to be dangerous if not diagnosed and treated earlier. Slow growth rate and appearance of symptoms in later stage of the disease adds to the morbidity and mortality. Therefore, clinical suspicion in cystic lesions of CNS is important for a correct diagnosis. Imaging techniques and histopathology aid neurosurgeon to reach a correct diagnosis and plan treatment accordingly. Preventing infection in humans depends on the education to improve hygiene and sanitation.
References
1. Abbassioun K, Amirjamshidi A. Diagnosis and management of hydatid cyst of the central nervous system: Part 1: General considerations and hydatid disease of the brain. Neurosurg Q. 2001. 11: 1-9
2. Ammann RW, Eckert J. Cestodes. Echinococcus. Gastroenterol Clin North Am. 1996. 25: 655-89
3. Aydin MD, Ozkan U, Altinörs N. Quadruplets hydatid cysts in brain ventricles: A case report. Clin Neurol Neurosurg. 2002. 104: 300-2
4. Bensaid AH, Dietemann JL, de la Palavesa MM, Klinkert A, Kastler B, Gangi A. Intracranial alveolar echinococcosis: CT and MRI. Neuroradiology. 1994. 36: 289-91
5. Beskonakli E, Cayli S, Yalçinlar Y. Primary intracranial extradural hydatid cyst extending above and below the tentorium. Br J Neurosurg. 1996. 10: 315-6
6. Boles DM. Cerebral echinococciasis. Surg Neurol. 1981. 16: 280-2
7. Bükte Y, Kemaloglu S, Nazaroglu H, Ozkan U, Ceviz A, Simsek M. Cerebral hydatid disease: CT and MR imaging findings. Swiss Med Wkly. 2004. 134: 459-67
8. Copley IB, Fripp PJ, Erasmus AM, Otto DD. Unusual presentations of cerebral hydatid disease in children. Br J Neurosurg. 1992. 6: 203-10
9. Dharker SR, Dharker RS, Vaishya ND, Sharma ML, Chaurasia BD. Cerebral hydatid cysts in central India. Surg Neurol. 1977. 8: 31-4
10. Dharker SR, Ramamurthi B, Tandon PN.editors. Hydatid disease. Text Book of Neurosurgery. New Delhi: Churchill Livingstone; 1996. p. 535-44
11. Diren HB, Ozcanli H, Boluk M, Kilic C. Unilocular orbital, cerebral and intraventricular hydatid cysts: CT diagnosis. Neuroradiology. 1993. 35: 149-50
12. Ersahin Y, Mutluer S, Güzelbag E. Intracranial hydatid cysts in children. Neurosurgery. 1993. 33: 219-24
13. Evliyaoglu C, Keskil S. Possible spontaneous “birth” of a hydatid cyst into the lateral ventricle. Childs Nerv Syst. 2005. 21: 425-8
14. Garcia LS, Bruckner DA.editors. Tissue-cestodes: Larval forms. In: Diagnostic Medical Parasitology. Washington, DC: ASM Press; 2001. p. 387-403
15. Geramizadeh B. Unusual locations of the hydatid cyst: A review from Iran. Iran J Med Sci. 2013. 38: 2-14
16. . Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ. 1996. 74: 231-42
17. Gupta S, Desai K, Goel A. Intracranial hydatid cyst: A report of five cases and review of literature. Neurol India. 1999. 47: 214-7
18. Guzel A, Tatli M, Maciaczyk J, Altinors N. Primary cerebral intraventricular hydatid cyst: A case report and review of the literature. J Child Neurol. 2008. 23: 585-8
19. Haliloglu M, Saatci I, Akhan O, Ozmen MN, Besim A. Spectrum of imaging findings in pediatric hydatid disease. AJR Am J Roentgenol. 1997. 169: 1627-31
20. Iyigun O, Uysal S, Sancak R, Hokelek M, Uyar Y, Bernay F. Multiple organ involvement hydatid cysts in a 2-year-old boy. J Trop Pediatr. 2004. 50: 374-6
21. Jiménez-Mejías ME, Castillo-Ojeda E, Cuello Contreras JA, García Gutiérrez D, Romero Arce J, Pachón Díaz J. Cerebral hydatidosis. Analysis of a series of 23 cases. Med Clin (Barc). 1991. 97: 125-32
22. Kak VK, Mathuriya SN, Chopra JS, Sawhney BI.editors. Hydatid disease of the nervous system. Neurology in Tropics. London: Churchill Livingstone; 1999. p. 244-58
23. Kamath SM, Mysorekar VV, Rao SG, Varma RG. Intraventricular hydatid cyst in a child. Indian J Pathol Microbiol. 2009. 52: 571-2
24. Karak PK, Mittal M, Bhatia S, Mukhopadhyay S, Berry M. Isolated cerebral hydatid cyst with pathognomonic CT sign. Neuroradiology. 1992. 34: 9-10
25. Khaldi M, Mohamed S, Kallel J, Khouja N. Brain hydatidosis: Report on 117 cases. Childs Nerv Syst. 2000. 16: 765-9
26. King C, Mandell G, Bennett J, Dolin R.editors. Cestodes (tapeworms). Principles and Practices of Infectious Diseases. New York: Churchill Livingstone; 2000. p. 633-40
27. Kohli A, Gupta RK, Poptani H, Roy R. In vivo proton magnetic resonance spectroscopy in a case of intracranial hydatid cyst. Neurology. 1995. 45: 562-4
28. Krajewski R, Stelmasiak Z. Cerebral hydatid cysts in children. Childs Nerv Syst. 1991. 7: 154-5
29. Maurya P, Singh VP, Prasad R, Bhaikhel KS, Sharma V, Kuma M. Intraventricular hydatid cyst causing entrapped temporal horn syndrome: A case report and review of literature. J Pediatr Neurosci. 2007. 2: 20-2
30. Menkü A, Kulaksizoglu O, Tucer B, Kurtsoy A, Akdemir H. Successful surgical excision of a gigantic cerebral hydatid cyst. Minim Invasive Neurosurg. 2004. 47: 61-4
31. Miabi Z, Hashemi HM, Ghaffarpour H, Ghelichna H, Media R. Clinicoradiological findings and treatment outcome in patients with intracranial hydatid cyst. Acta Med Iran. 2005. 43: 359-64
32. Moro P, Schantz PM. Echinococcosis: A review. Int J Infect Dis. 2009. 13: 125-33
33. Moro PL, Schantz PM. Echinococcosis: Historical landmarks and progress in research and control. Ann Trop Med Parasitol. 2006. 100: 703-14
34. Oprişan A, Popescu BO. Intracranial cysts: An imagery diagnostic challenge. Scientific World Journal 2013. 2013. p.
35. Pasaoglu A, Orhon C, Akdemir H. Multiple primary hydatid cysts of the brain. Turk J Pediatr. 1989. 31: 57-61
36. Patrikar DM, Mitra KR, Bhutada VR. Cerebral hydatid disease. Australas Radiol. 1993. 37: 226-7
37. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003. 23: 475-94
38. Prasad RS, Singh K, Sharma V. Primary Intracranial Hydatid Cysts: Review of Ten Cases. World J Surg Res. 2013. 4: 12-8
39. Raja Reddy D, Rao BD, Prabhakar V, Subramanian MV. Hydatid disease of the central nervous system. Indian J Surg. 1972. 34: 191-
40. Reittner P, Szolar DH, Schmid M. Case report. Systemic manifestation of Echinococcus alveolaris infection. J Comput Assist Tomogr. 1996. 20: 1030-2
41. Rivierez M, el-Azhari A, el Tantaoui M, Alaoui M. Hydatid cyst of the cavernous sinus. A case. Neurochirurgie. 1992. 38: 46-9
42. Sadjjadi SM. Present situation of echinococcosis in the Middle East and Arabic North Africa. Parasitol Int. 2006. 55: S197-202
43. Sardana VR, Dharker SR, Mittal RS, Nathani R. Multiple intracranial hydatid cysts. Neurol India. 1991. 39: 205-8
44. Sharma SC, Ray RC. Primary hydatid cyst of the brain in an adult: Report of a case. Neurosurgery. 1988. 23: 374-6
45. Sierra J, Oviedo J, Berthier M, Leiguarda R. Growth rate of secondary hydatid cysts of the brain. Case report. J Neurosurg. 1985. 62: 781-2
46. Tunaci M, Tunaci A, Engin G, Ozkorkmaz B, Ahishali B, Rozanes I. MRI of cerebral alveolar echinococcosis. Neuroradiology. 1999. 41: 844-6
47. Tüzün M, Hekimoglu B. Hydatid disease of the CNS: Imaging features. AJR Am J Roentgenol. 1998. 171: 1497-500
48. Yang YR, Sun T, Li Z, Zhang J, Teng J, Liu X. Community surveys and risk factor analysis of human alveolar and cystic echinococcosis in Ningxia Hui Autonomous Region, China. Bull World Health Organ. 2006. 84: 714-21