- Department of Neurosurgery, University of Minnesota, Minneapolis, Minnesota, United States.
Correspondence Address:
Shiwei Huang, Department of Neurosurgery, University of Minnesota, Minneapolis, Minnesota, United States.
DOI:10.25259/SNI_808_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shiwei Huang, Daniel Guillaume. Cerebral spinal fluid overdrainage from shunt tap using large bore coring needle: A case report. 23-Dec-2022;13:592
How to cite this URL: Shiwei Huang, Daniel Guillaume. Cerebral spinal fluid overdrainage from shunt tap using large bore coring needle: A case report. 23-Dec-2022;13:592. Available from: https://surgicalneurologyint.com/surgicalint-articles/12071/
Abstract
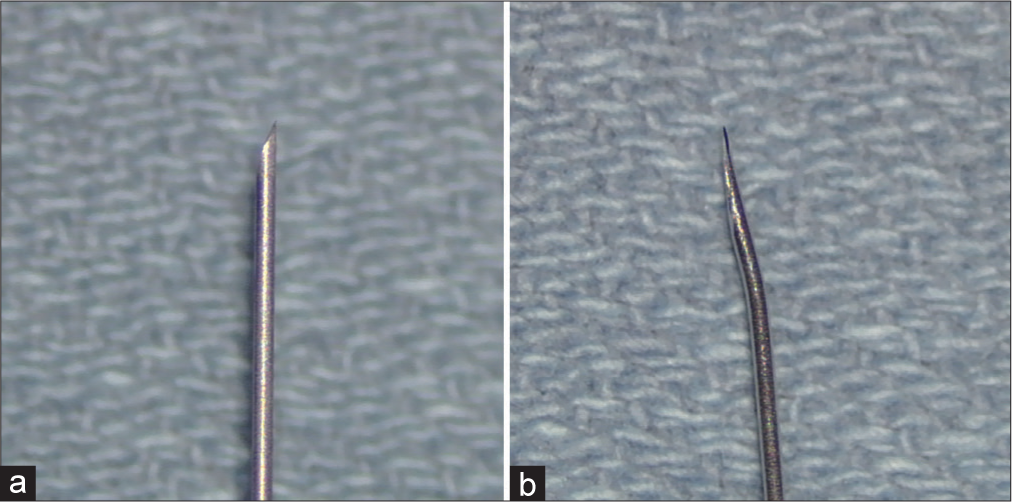
Background: Tapping a ventriculoperitoneal shunt percutaneously using a coring needle, such as a butterfly needle, is a common neurosurgical practice despite manufacturers’ recommendation to use a Huber type non-coring needle.
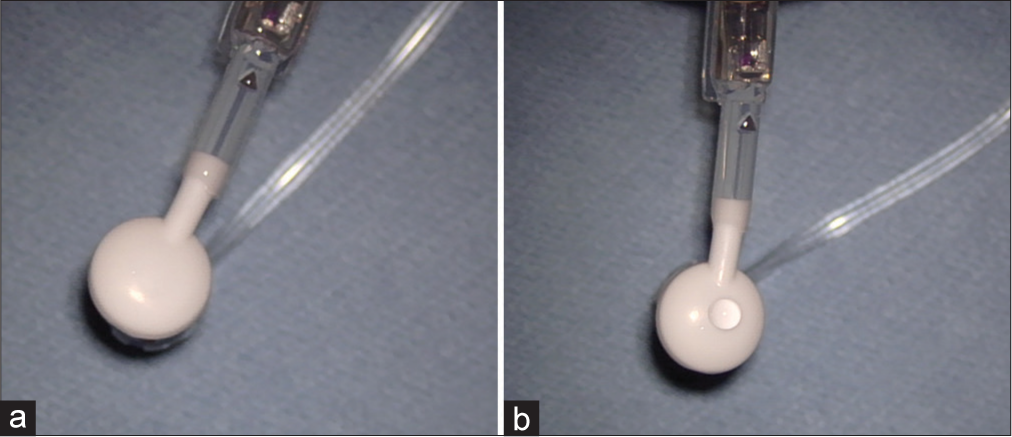
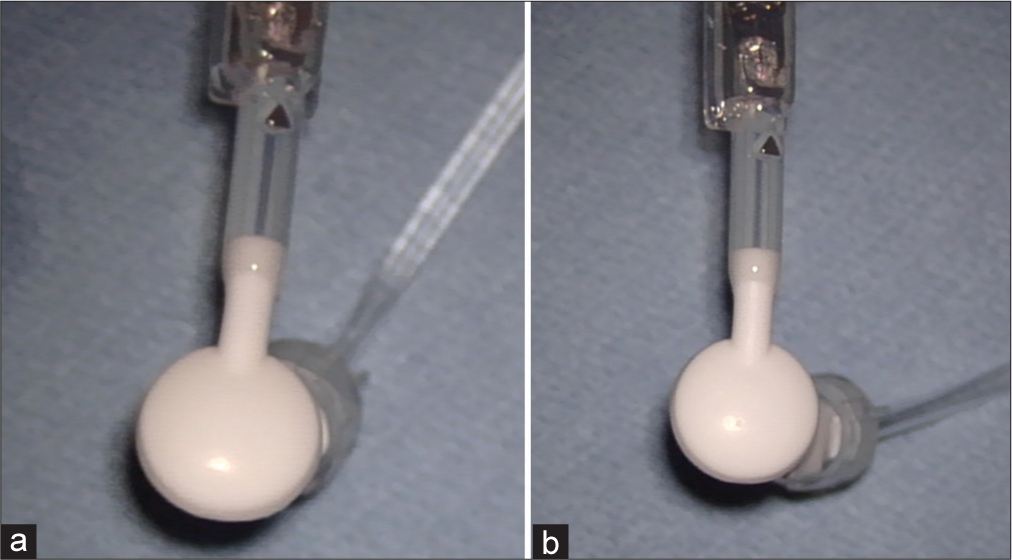
Case Description: A 26-year-old woman, with congenital hydrocephalus and history of multiple shunt revision and shunt taps, presented with symptoms consistent with intracranial hypotension. During her shunt revision, cerebrospinal fluid (CSF) was found to be leaking from her shunt reservoir defects which were believed to be caused by prior shunt taps. An in vitro study duplicated this finding in which several areas of leak were observed from the valve tapped using the coring needle, while none was observed from the valve tapped using the non-coring needle.
Conclusion: Taping a shunt using a coring needle can damage the shunt reservoir and cause CSF overdrainage.
Keywords: Ventriculoperitoneal shunt, Intracranial hypotension, Huber needle
INTRODUCTION
Strides have been made in hydrocephalus treatment since the first description of this condition. Placement of a ventriculoperitoneal shunt has improved the clinical course and quality of life of patients with hydrocephalus. Accessing the shunt through the reservoir through a percutaneous shunt tap can reveal shunt obstruction and infection. It is less invasive than surgical exploration, well tolerated, and carries low overall risks.[
CASE DESCRIPTION
A 26-year-old female presented with congenital hydrocephalus secondary to congenital aqueduct stenosis status post ventriculoperitoneal shunt placement at 5 years of age. Since then, she required shunt revisions at the age of 8, 12, and 13. During the last shunt revision, a CODMAN® HAKIM® Programmable Valve was placed, she initially reported symptom resolution but over the years she intermittently presented to outside hospitals due to headaches, nausea, and vomiting. Given her multiple prior shunt revisions and the fact that those symptoms were similar to her presenting symptoms of shunt malfunction, her shunt was tapped multiple times to assess patency. Outside records showed that her shunt was tapped using 21G and 23G butterfly needles, and the shunt appeared to be patent. Her imaging did not reveal enlarged ventricles, and she ultimately presented to our institution for second opinion. While under the care of our institution, her shunt was tapped once with 21G needle to assess the proximal flow, and two separate nuclear medicine studies were done during which time her shunt was assessed using a 23G butterfly needle and a 25G butterfly needle. All those studies demonstrated, her shunt was functional. She underwent two separate intracranial monitor placement which showed normal to low pressure. In the interim her symptoms, especially the positional headache, worsened, and ultimately her shunt was explored. Intraoperatively, it was discovered that there were multiple areas of leakage from the reservoir presumably from the previous shunt taps. Her proximal catheter was changed, and the valve was replaced with a CODMAN® CERTAS® Plus Programmable Valve. Since the surgery, she reported symptom improvements especially in positional headaches and energy levels.
DISCUSSION
Huber needles are non-coring needles designed to access an implantable venous access device, such as a port without making a “core biopsy” of the port membrane and thus damaging the port membrane.[
CONCLUSION
Shunt taps should always be performed with small bore non-coring Huber type needles as recommended by manufacturers to avoid damaging the shunt system.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. CODMAN CERTAS® Plus Programmable Valve CODMAN CERTAS® Tool Kit. Available from: https://www.integralife.com/file/general/1596745162.pdf [Last accessed on 2021 Sep 17].
2. CODMAN HAKIM® Programmable Valves. Available from: https://www.integralife.com/file/general/1592942265.pdf [Last accessed on 2021 Sep 17].
3. Fougo JL, editors. Huber Needle: Different Types, Uses, Prevention of Accidents. Total Implant Venous Access Devices. Milano: Springer; 2012. p. 29-33
4. Miller JP, Fulop SC, Dashti SR, Robinson S, Cohen AR. Rethinking the indications for the ventriculoperitoneal shunt tap. J Neurosurg Pediatr. 2008. 1: 435-8
5. Noetzel MJ, Baker RP. Shunt fluid examination: Risks and benefits in the evaluation of shunt malfunction and infection. J Neurosurg. 1984. 61: 328-32
6. Rickham P. A ventriculostomy reservoir. Br Med J. 1964. 2: 173
7. Rocque BG, Lapsiwala S, Iskandar BJ. Ventricular shunt tap as a predictor of proximal shunt malfunction in children: A prospective study. J Neurosurg Pediatr. 2008. 1: 439-43
8. Sood S, Kim S, Ham SD, Canady AI, Greninger N. Useful components of the shunt tap test for evaluation of shunt malfunction. Childs Nerv Syst. 1993. 9: 157-61
9. Spiegelman L, Asija R, Da Silva SL, Krieger MD, McComb JG. What is the risk of infecting a cerebrospinal fluid–diverting shunt with percutaneous tapping?. J Neurosurg Pediatr. 2014. 14: 336-9
10. Strata® Products. Available from: https://www.manuals.medtronic.com/content/dam/emanuals/st/contrib_250941.pdf [Last accessed on 2021 Sep 17].