- Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
- Department of Neurology, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
Correspondence Address:
Andrew K. Conner
Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma, United States.
DOI:10.25259/SNI_126_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Camille K. Milton1, David L. Gordon2, Chad A. Glenn1, Andrew K. Conner1. Cerebral venous thrombosis of the sphenoparietal sinus: A case report. 03-May-2021;12:197
How to cite this URL: Camille K. Milton1, David L. Gordon2, Chad A. Glenn1, Andrew K. Conner1. Cerebral venous thrombosis of the sphenoparietal sinus: A case report. 03-May-2021;12:197. Available from: https://surgicalneurologyint.com/surgicalint-articles/10786/
Abstract
Background: Cerebral venous thrombosis (CVT) is a rare cause of stroke that preferentially affects reproductive aged females and patients with hereditary or acquired thrombotic risk factors. The superior sagittal sinus and transverse sinus are the two most common sites for thrombus formation.
Case Description: We report a case of CVT arising in a very rare location, the sphenoparietal sinus. A 32-year-old woman with a history of factor V Leiden mutation and multiple prior episodes of venous thromboembolism presented with a new-onset seizure, headache, and emesis. CT angiography ultimately revealed thrombosis of the left sphenoparietal sinus. The patient received anticoagulation with apixaban with resolution of symptoms and without complications.
Conclusion: This case serves as an uncommon example of sphenoparietal sinus thrombosis managed with novel oral anticoagulant treatment.
Keywords: Anticoagulant agents, Cerebral venous sinus thrombosis, Cerebral venous sinuses, Thrombolytic therapy, Thrombophilia
INTRODUCTION
Cerebral venous thrombosis (CVT) is a relatively rare condition accounting for 0.5% of stroke cases.[
CVT most commonly arises within the dural venous sinuses, but may also affect the superficial cortical veins or the deep venous system.[
We report a case of CVT localized to the sphenoparietal sinus occurring in a woman with factor V Leiden mutation. The clinical presentation, diagnostic evaluation, and management of this unusual diagnosis are described. In addition, we discuss the significance of this case in the context of CVT literature.
CASE REPORT
A 32-year-old woman was transferred to our service from an outside hospital emergency department after presenting with a new-onset complex-partial seizure with secondary generalization, headache, and emesis. The patient had a history of factor V Leiden mutation, cigarette smoking, and obesity (BMI 40.6). She had suffered a miscarriage and multiple prior episodes of venous thromboembolism with subsequent placement of an IVC filter. Six months before presentation, the patient had discontinued warfarin anticoagulation for stated financial reasons.
Five days before presentation, the patient awoke with a left frontal headache accompanied by nausea and vomiting. These symptoms persisted and, on the day of presentation, she experienced a complex partial seizure with secondary generalization. The seizure was manifested by expressive aphasia, right hand numbness, and left head deviation culminating in generalized tonic-clonic activity and a postictal state lasting several minutes.
At the outside hospital emergency department, she received levetiracetam 1500 mg BID and CT head imaging revealed two small areas of hypodensity in the left subinsular and frontal opercular areas. The patient was then transferred to our tertiary care institution for definitive management. On arrival, the patient’s neurological examination was intact and she reported a severe (8/10) headache. MRI imaging performed at our institution revealed increased FLAIR signal indicative of vasogenic edema. DWI and ADC findings in this area were thought to represent acute hemorrhage and not acute ischemia. CT head angiography was then performed, revealing CVT of the left sphenoparietal sinus. Imaging findings are shown in [
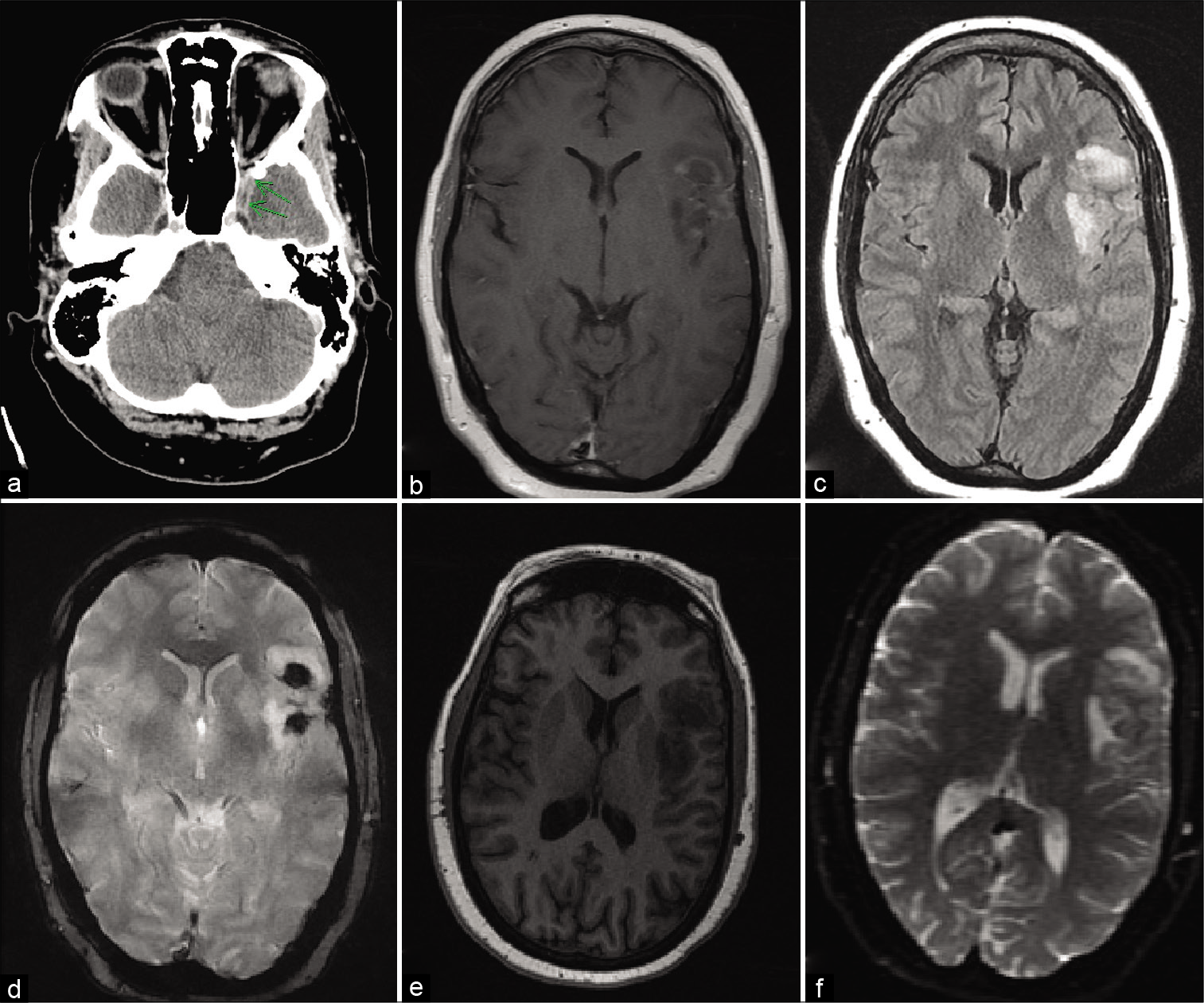
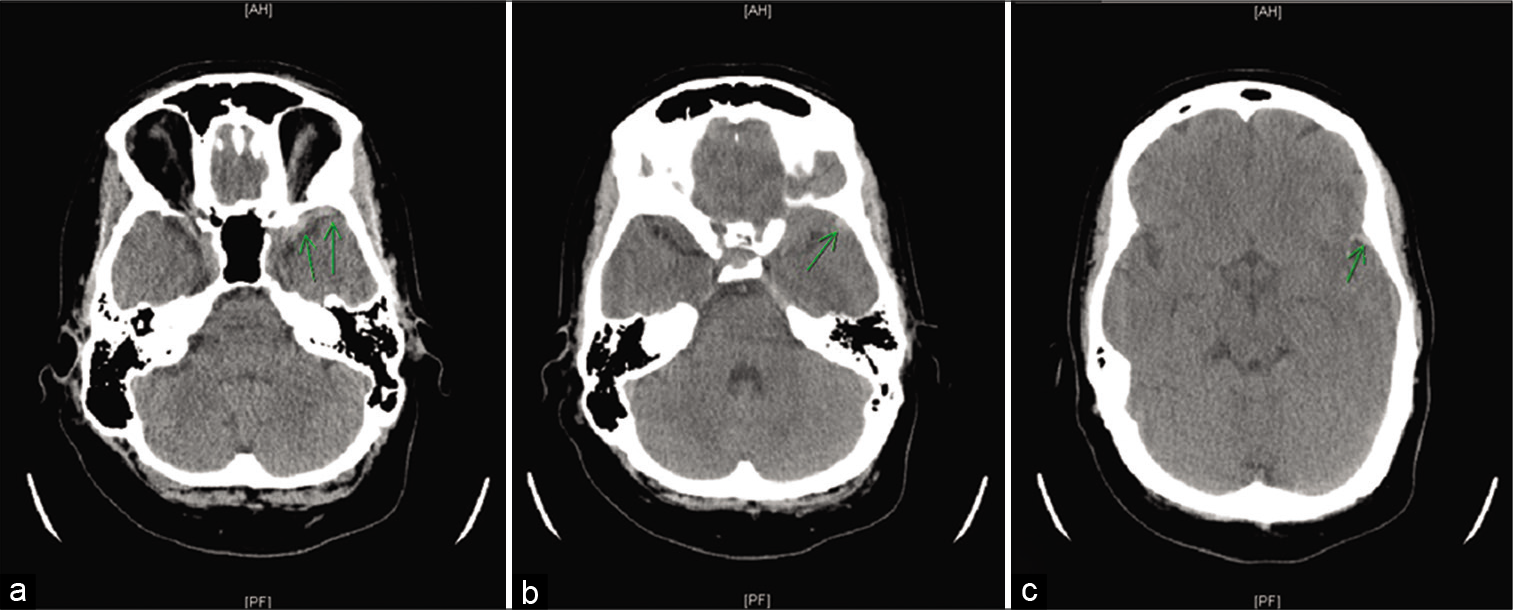
Figure 1:
Delayed postcontrast head CT obtained with CT angiography showing suggestion of a filling defect (arrows) in the region of the left sphenoparietal sinus (a), T1 with contrast (b), T2 flair (c), GRE (d), FSPGR BRAVO (e), and DWI (f) MRI sequences demonstrating findings of FLAIR hyperintensity, diffusion restriction, susceptibility blooming, and mild enhancement in the region of the left frontal-temporal operculum and insula indicative of venous infarct.
The patient continued to receive levetiracetam 1500 mg BID initiated at the outside hospital emergency department and began apixaban 5 mg BID with a recommendation to continue this medication lifelong. The patient was followed clinically, and no posttreatment imaging studies were performed. Following a 3-day hospital stay, the patient reported a significant reduction in headache severity and was discharged home.
DISCUSSION
While the presentation of CVT is highly variable, it commonly produces one of the following clinical syndromes: (1) intracranial hypertension (headache, papilledema, and visual disturbance), (2) focal neurologic syndrome (focal deficits and seizures), or (3) encephalopathy.[
The anatomy of the sphenoparietal sinus, first identified by Breschet in 1829, has received limited attention from the medical literature.[
Our review of the English language literature for reports of sphenoparietal sinus thrombosis identified only one previously published case. In 2018, Di Caprera et al. reported a case of sphenoparietal sinus thrombosis found in a 38-year-old Italian woman with no identifiable risk factors.[
Low-molecular-weight heparin followed by warfarin administration remains the standard of care for CVT,[
CONCLUSION
We have described an uncommon case of CVT of the sphenoparietal sinus successfully managed with DOAC administration. While rare, one should consider the diagnosis of sphenoparietal sinus thrombosis in patients presenting with signs and symptoms of CVT and the characteristic imaging findings reported herein.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. A Clinical Trial Comparing Efficacy and Safety of Dabigatran Etexilate with Warfarin in Patients with Cerebral Venous and Dural Sinus;. Available from: https://www.clinicaltrials.gov/show/nct02913326. [Last accessed on 2021 Jan 31].
2. Agrawal K, Burger K, Rothrock JF. Cerebral sinus thrombosis. Headache. 2016. 56: 1380-9
3. Bousser MG, Ferro JM. Cerebral venous thrombosis: An update. Lancet Neurol. 2007. 6: 162-70
4. Breschet G.editors. Research of the Anatomy, Physiology, and Pathology of the Venus System with Special Emphasis on the Veins of Bones. Paris: Villeret et Rouen; 1829. p.
5. Bushnell C, Saposnik G. Evaluation and management of cerebral venous thrombosis. Continuum (Minneap Minn). 2014. 20: 335-51
6. Coutinho JM, Zuurbier SM, Stam J. Declining mortality in cerebral venous thrombosis: A systematic review. Stroke. 2014. 45: 1338-41
7. Coutinho JM. Cerebral venous thrombosis. J Thromb Haemost. 2015. 13: S238-44
8. di Caprera E, de Corato L, Giuricin V, Pensabene MC, Marfia G, Melis M. Cerebral venous thrombosis presenting like a subdural hemorrhage at magnetic resonance imaging: An Italian case report. Eur J Radiol Open. 2018. 5: 31-4
9. Dmytriw AA, Song JS, Yu E, Poon CS. Cerebral venous thrombosis: State of the art diagnosis and management. Neuroradiology. 2018. 60: 669-85
10. Ferro JM, Coutinho JM, Dentali F, Kobayashi A, Alasheev A, Canhão P. Safety and efficacy of dabigatran etexilate vs dose-adjusted warfarin in patients with cerebral venous thrombosis: A randomized clinical trial. JAMA Neurol. 2019. 76: 1457-65
11. Lee GK, Chen VH, Tan CH, Leow AS, Kong WY, Sia CH. Comparing the efficacy and safety of direct oral anticoagulants with vitamin K antagonist in cerebral venous thrombosis. J Thromb Thrombolysis. 2020. 50: 724-31
12. Patel SI, Obeid H, Matti L, Ramakrishna H, Shamoun FE. Cerebral venous thrombosis: Current and newer anticoagulant treatment options. Neurologist. 2015. 20: 80-8
13. Ruíz DS, Fasel JH, Rüfenacht DA, Gailloud P. The sphenoparietal sinus of breschet: Does it exist? An anatomic study. AJNR Am J Neuroradiol. 2004. 25: 112-20
14. Sader N, de Lotbiniere-Bassett M, Tso MK, Hamilton M. Management of venous sinus thrombosis. Neurosurg Clin N Am. 2018. 29: 585-94
15. Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, Cushman M. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American heart association/ American stroke association. Stroke. 2011. 42: 1158-92
16. Silvis SM, de Sousa DA, Ferro JM, Coutinho JM. Cerebral venous thrombosis. Nat Rev Neurol. 2017. 13: 555-65
17. Silvis SM, Middeldorp S, Zuurbier SM, Cannegieter SC, Coutinho JM. Risk factors for cerebral venous thrombosis. Semin Thromb Hemost. 2016. 42: 622-31
18. Study of Rivaroxaban for CeREbral Venous Thrombosis. Available from: https://www.clinicaltrials.gov/show/nct03178864. [Last accessed on 2021 Jan 31].
19. Tubbs RS, Salter EG, Wellons JC, Blount JP, Oakes WJ. The sphenoparietal sinus. Neurosurgery. 2007. 60: ONS9-12