- Neurosurgery Section, Hospital Universitario Fundación Santa Fé de Bogotá, Bogotá D.C, Colombia.
DOI:10.25259/SNI_380_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Diego Fernando Gómez-Amarillo, Luis Fernando Pulido, Isabella Mejía, Catalina García-Baena, María Fernanda Cárdenas, Lina María Gómez, Yuli Viviana Fuentes, Daniela Volcinschi-Moros, Daniel Jaramillo-Velásquez, Juan Fernando Ramón, Juan Armando Mejía, Enrique Jiménez, Fernando Hakim. Cerebrospinal fluid closing pressure-guided tap test for the diagnosis of idiopathic normal pressure hydrocephalus: A descriptive cross-sectional study. 02-Oct-2020;11:315
How to cite this URL: Diego Fernando Gómez-Amarillo, Luis Fernando Pulido, Isabella Mejía, Catalina García-Baena, María Fernanda Cárdenas, Lina María Gómez, Yuli Viviana Fuentes, Daniela Volcinschi-Moros, Daniel Jaramillo-Velásquez, Juan Fernando Ramón, Juan Armando Mejía, Enrique Jiménez, Fernando Hakim. Cerebrospinal fluid closing pressure-guided tap test for the diagnosis of idiopathic normal pressure hydrocephalus: A descriptive cross-sectional study. 02-Oct-2020;11:315. Available from: https://surgicalneurologyint.com/surgicalint-articles/10307/
Abstract
Background: Tap test improves symptoms of idiopathic normal pressure hydrocephalus (iNPH); hence, it is widely used as a diagnostic procedure. However, it has a low sensitivity and there is no consensus on the parameters that should be used nor the volume to be extracted. We propose draining cerebrospinal fluid (CSF) during tap test until a closing pressure of 0 cm H2O is reached as a standard practice. We use this method with all our patients at our clinic.
Methods: This is a descriptive cross-sectional study where all patients with presumptive diagnosis of iNPH from January 2014 to December 2019 were included in the study. We used a univariate descriptive analysis and stratified analysis to compare the opening pressure and the volume of CSF extracted during the lumbar puncture, between patients in whom a diagnosis of iNPH was confirmed and those in which it was discarded.
Results: A total of 92 patients were included in the study. The mean age at the time of presentation was 79.4 years and 63 patients were male. The diagnosis of iNPH was confirmed in 73.9% patients. The mean opening pressure was 14.4 cm H2O mean volume of CSF extracted was 43.4 mL.
Conclusion: CSF extraction guided by a closing pressure of 0 cm H2O instead of tap test with a fixed volume of CSF alone may be an effective method of optimizing iNPH symptomatic improvement and diagnosis.
Keywords: Cerebrospinal fluid closing pressure, Cerebrospinal fluid drainage, Cerebrospinal fluid extraction, Closing pressure-guided, Idiopathic normal pressure hydrocephalus, Tap test
INTRODUCTION
Idiopathic normal pressure hydrocephalus (iNPH) is the most common cause of hydrocephalus in the adult population and a major cause of reversible dementia with surgical management.[
Different diagnostic methods have been described which include external lumbar drainage (ELD), infusion test, cerebral magnetic resonance imaging testing of elasticity, and cerebrospinal fluid (CSF) biochemical parameter testing.[
CSF drainage during tap test, emulates the effect shunting surgery would have and theoretically predicts the outcome.[
However, tap test has a low sensitivity, so a negative result may not exclude the diagnosis and additional tests with higher sensitivity may be needed.[
Volume of CSF within the spinal subarachnoid space is variable among individuals; therefore, pressure changes after CSF extraction is different for each patient. This is our rationale for extracting CSF until a closing pressure of 0 cm H2O is reached instead of a fixed volume. We hypothesize that this method guarantees an adequate quantity of drained fluid and we share here our experience. As there is no diagnostic test considered to be the gold standard, we gather all the available information including symptoms, MRI findings, and symptom improvement after CSF drainage.
MATERIALS AND METHODS
This is a descriptive cross-sectional study, in which medical records of patients treated for NPH in our institution between January 2014 and December 2019 were studied.
The parameters of the procedure for each subject included: opening pressure, volume of CSF extracted, and closing pressure. We included patients with suspected NPH-defined as the classic triad of symptoms. All patients underwent standard brain MRI, gait, and neuropsychologic tests before and after lumbar puncture. During lumbar puncture, CSF was drained until a pressure of 0 cm H2O was reached using a manometer.
Data were collected in an Excel® spreadsheet and analyzed using STATA® version 14. We used a univariate descriptive analysis. Absolute and relative frequencies were used for qualitative variables; central tendency and dispersion measures for quantitative variables. We determined if a quantitative variable had a normal distribution with the Shapiro–Wilk test using a significance level of 5% (P < 0.05). For variables with normal distribution, mean and standard deviations (SD) were used. For those without normal distribution median and interquartile ranges were used.
A stratified analysis was used to compare the opening pressure and the volume of CSF extracted during lumbar puncture, between the patients in whom the diagnosis of NPH was confirmed and those in whom it was discarded.
RESULTS
A total of 93 patients with clinical suspicion of iNPH were evaluated using a modified tap test whereby CSF was extracted until a closing pressure of 0 cm H2O was reached. Of these, 92 patients were included in the study (one was excluded because the CSF opening pressure was not recorded).
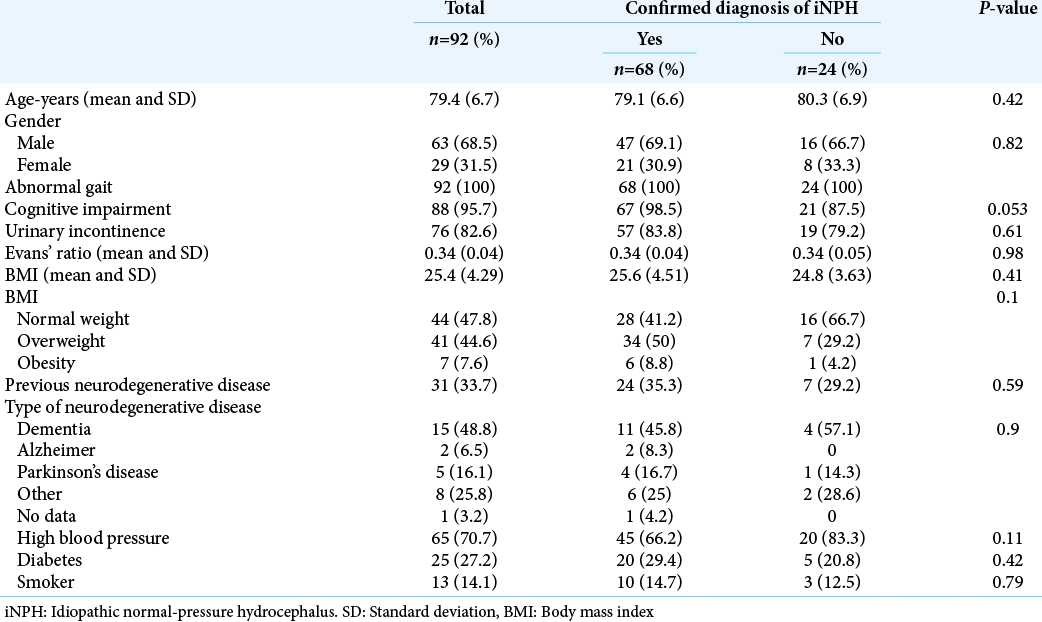
The mean age at the time of evaluation was 79.4 years (SD 6.7) and it ranged from 52 to 96 years. Sixty-three patients (68.5%) were male. Regarding symptoms: 100% of them presented with gait disturbance at the moment of evaluation, 88 patients (95.7%) had cognitive disturbances, and 76 (82.6%) had urinary incontinence [
Of the 92 patients that were included, 68 (73.9%) had a confirmed diagnosis of iNPH. The mean opening pressure was 14.4 cm H2O (SD 4.8) and average volume of CSF extracted was 43.4 mL (SD 10.8). When carrying out the analysis of patient characteristics, discriminating groups according to the diagnosis of iNPH, no statistically significant differences were identified between the groups [
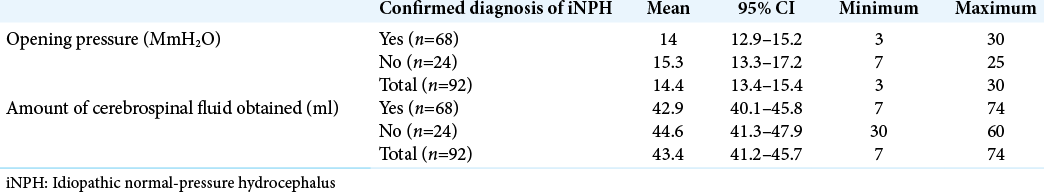
A stratified analysis of the opening pressure and the amount of fluid obtained during lumbar puncture was performed comparing patients with a confirmed diagnosis of iNPH and those without iNPH. Average values for opening pressure and extracted volume in the group with iNPH and those without iNPH were 14.0 cm H2O and 42.9 mL and 15.3 cm H2O and 44.6 mL, respectively. According to this, no significant difference was found between the groups [
DISCUSSION
Diagnosis of iNPH was confirmed in 73.9% of patients using this modified tap test. High clinical suspicion along with the modified tap test might be an effective diagnostic method for this pathology. The specificities of tap test (33–100%) and ELD (80–100%) are comparable. Although infusion test, which determines CSF flow resistance, has a higher sensitivity compared to tap test (57–100 vs. 28–62%), they both have comparable PPV values.[
Although all tests have disadvantages, ELD is considered an exact method due to its high PPV and NPV and has been used for over 20 years; however, it is not as common. It requires a brief period of inpatient admission and the most frequent complication is meningitis, which is seen in 2–3% of patients.[
Kahlon et al. concluded that infusion test and tap test have a high PPV in predicting outcome after shunting. However, infusion test is more sensitive and tap test more specific. This means, the latter may indicate surgery when positive, but may require additional testing when negative.[
The optimal volume of CSF that should be extracted during the lumbar puncture for tap test has not been determined, much variation exists on the recommended amount, and there is no significant association between the volume of CSF removed and gait outcomes when extracted volume falls within the 28–50 mL range.[
To the best of our knowledge, there is no such procedure such as the modified tap test we describe in this study, first proposed by Doctor Salomon Hakim and later corroborated.[
CONCLUSION
The gold standard for the diagnosis of NPH is the clinical improvement after CSF drainage, assessed with tap test. Nevertheless, recommendations on the optimal volume of CSF that should be drained are inconsistent and variable. We propose a novel standardized procedure, to the best of our knowledge, not reported in the literature, based on a closing pressure of 0 cm H2O after lumbar puncture to assure enough and adequate volume of fluid extracted. Our approach is reproducible, and our results show that using this method, the number of patients diagnosed with NPH increases when compared with the published literature. This study warrants a diagnostic test study to confirm these results.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med. 1965. 273: 117-26
2. Damasceno BP, Carelli EF, Honorato DC, Facure JJ. The predictive value of cerebrospinal fluid tap-test in normal pressure hydrocephalus. Arq Neuropsiquiatr. 1997. 55: 179-85
3. Damasceno BP. Hidrocefalia de pressão normal: Avaliação diagnóstica e preditiva. Dement Neuropsychol. 2009. 3: 8-15
4. Eide PK, Sorteberg W. Diagnostic intracranial pressure monitoring and surgical management in idiopathic normal pressure hydrocephalus: A 6-year review of 214 patients. Neurosurgery. 2010. 66: 80-90
5. Greenberg BM, Williams MA. Infectious complications of temporary spinal catheter insertion for diagnosis of adult hydrocephalus and idiopathic intracranial hypertension. Neurosurgery. 2008. 62: 431-6
6. Hakim S, Adams RD. The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci. 1965. 2: 307-27
7. Hamilton R, Patel S, Lee EB, Jackson EM, Lopinto J, Arnold SE. Lack of shunt response in suspected idiopathic normal pressure hydrocephalus with Alzheimer disease pathology. Ann Neurol. 2010. 68: 535-40
8. Kahlon B, Sundbärg G, Rehncrona S. Comparison between the lumbar infusion and CSF tap tests to predict outcome after shunt surgery in suspected normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2002. 73: 721-6
9. Klinge P, Marmarou A, Bergsneider M, Relkin N, Black P. Outcome of shunting in idiopathic normal-pressure hydrocephalus and the value of outcome assessment in shunted patients. Neurosurgery. 2005. 57: S40-52
10. Lenfeldt N, Larsson A, Nyberg L, Andersson M, Birgander R, Eklund A. Idiopathic normal pressure hydrocephalus: Increased supplementary motor activity accounts for improvement after CSF drainage. Brain. 2008. 131: 2904-12
11. Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM. The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005. 57: S17-28
12. Marmarou A, Young HF, Aygok GA, Sawauchi S, Tsuji O, Yamamoto T. Diagnosis and management of idiopathic normal-pressure hydrocephalus: A prospective study in 151 patients. J Neurosurg. 2005. 102: 987-97
13. Mckhann G, Mayeux R. Brain drain: A bottom-up approach to normal pressure hydrocephalus. Ann Neurol. 2010. 68: 415-7
14. Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M. Guidelines for management of idiopathic normal pressure hydrocephalus: Second edition. Neurol Med Chir (Tokyo). 2012. 52: 775-809
15. Shprecher D, Schwalb J, Kurlan R. Normal pressure hydrocephalus: Diagnosis and treatment. Curr Neurol Neurosci Rep. 2008. 8: 371-6
16. Thakur SK, Serulle Y, Miskin NP, Rusinek H, Golomb J, George AE. Lumbar puncture test in normal pressure hydrocephalus: Does the volume of csf removed affect the response to tap?. Am J Neuroradiol. 2017. 38: 1456-60
17. Wikkelso C, Andersson H, Blomstrand C, Lindqvist G. The clinical effect of lumbar puncture in normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 1982. 45: 64-9
18. Williams MA, Relkin NR. Diagnosis and management of idiopathic normal-pressure hydrocephalus. Neurol Clin Pract. 2013. 3: 375-85